Lower Abdominal Pain in an Obese Teenage Boy

The Case: An obese 14-year-old boy has had lower abdominal pain for the past 3 days. He denies any nausea, vomiting, diarrhea, fever, or chills.
Physical examination is remarkable for weight of 114 kg and blood pressure of 158/73 mm Hg. Abdominal examination reveals right lower and middle quadrant tenderness with mild rebound; however, Rovsing, psoas, and Murphy signs are negative.
Laboratory results show a white blood cell count of 9600/µL, with 62% segmented neutrophils and 38% lymphocytes.
Acute appendicitis is suspected, and CT of the abdomen is performed.
What is the cause of this teenage boy’s abdominal pain?
•Appendicitis
•Omental infarction
•Intussusception
•Intestinal malrotation
•Acute cholecystitis
•Gonadal torsion
(Answer and discussion begin on next page.)
Answer: Omental infarction
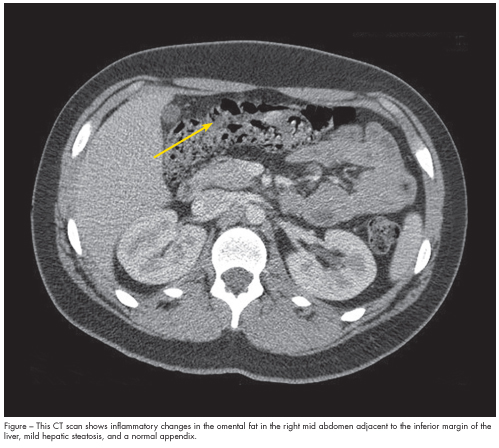
Discussion: The CT scan shows inflammatory changes in the omental fat in the right mid abdomen adjacent to the inferior margin of the liver, mild hepatic steatosis, and a normal appendix (Figure).
The patient was treated conservatively with analgesics and follow-up in 7 days. During that time, he recovered uneventfully and was symptom-free.
OMENTAL INFARCTION: A RARE CAUSE OF ABDOMINAL PAIN IN CHILDREN
Omental infarction was first described by Bush in 1896. About 15% of all cases involve children.1 The incidence in the pediatric population has risen in the past few years—a trend that seems to be related to the prevalence of obesity among children and adolescents.2 Other possible risk factors include trauma, straining, overeating, overexertion, and sudden positional changes. There is a male predominance, which may be attributed to the greater omental fat accumulation in males compared with females.3,4
Etiology. The cause of omental infarction is unclear but has been hypothesized to be a vasculitis of adipose tissue from increased intraabdominal pressure or from vascular congestion.4
Clinical manifestations. Patients classically pre-sent with acute or subacute abdominal pain, often in the right lower quadrant. They are usually afebrile or have low-grade fever. GI symptoms (such as nausea, vomiting, diarrhea, and anorexia) are uncommon. Laboratory findings may include mild leukocytosis and a mildly
elevated C-reactive protein level.3
Diagnostic testing. Ultrasound criteria for the diagnosis of omental infarction requires identification of a hyperechoic mass mainly in the right side of the
abdomen with a normal appendix.5 Although ultrasonography is accurate, it is operator dependent and its use in the diagnosis of omental infarction is limited because most children with this condition are obese. CT is the gold standard diagnostic test.6 The most common finding is a triangular or oval heterogenous fatty mass located between the anterior abdominal wall and the transverse or ascending colon with surrounding
inflammatory changes.5
Management. The choice of treatment remains controversial. Most surgeons favor operative management because it avoids the development of an abscess and adhesions from necrotic tissue and the anticipated recovery time is short. However, omental infarction is benign
and known to resolve spontaneously in children within 2 weeks. Thus, conservative treatment that spares patients unnecessary surgery would be preferable.
For patients without complications, the common practice has been to treat with analgesics on an outpatient basis or admit for observation. Identification of a normal appendix by imaging and confirmation of omental infarction are necessary for consideration of conservative treatment.3
DIFFERENTIAL DIAGNOSIS
Appendicitis is the most common cause of surgery in children who present with abdominal pain. It can occur in children of any age, although it is rare in infants. Patients with appendicitis classically present with visceral, vague, poorly localized, periumbilical pain. Within 6 to 48 hours, the overlying peritoneum becomes inflamed and the pain becomes parietal, well localized, and constant in the right iliac fossa.7 In equivocal cases, abdominal plain films or ultrasound imaging may be helpful but can be limited in some patients, such as those with obesity.8 CT is typically the diagnostic test of choice.
Intussusception most often occurs in infants between 3 months and 1 year of age. Colicky abdominal pain, flexing of the legs, fever, lethargy, and vomiting are characteristic symptoms on presentation. Intestinal obstruction and paucity of wind in the right lower quadrant on plain abdominal films may suggest the diagnosis. The pathological location is typically ileocaecal. Abdominal ultrasound images may establish the diagnosis. Contrast enema (air or contrast reagent) is the most specific and sensitive test for diagnosis and is used for treatment. In cases in which this is unsuccessful or where peritonitis exits, surgical reduction is required.9
Intestinal malrotation is the term used to describe an entire spectrum of rotational and fixation disturbances that can occur during embryonic development. It is commonly identified in the neonatal period but can be found in older children and even adults. Presenting symptoms may include abdominal pain and vomiting. Patients with malrotation are at risk for midgut volvulus and require emergency surgical consultation. Typically this involves upper GI contrast studies. Intestinal malrotation can be detected with CT. The Ladd procedure is the treatment of choice.10
Acute cholecystitis, sudden gallbladder inflammation caused by cystic duct obstruction, is most often caused by gallstones. Most affected children have a predisposing condition, such as a hemoglobinopathy or cystic fibrosis. Common symptoms include epigastric or right upper quadrant pain, anorexia, nausea, and vomiting. Patients usually appear ill, are febrile, and lie still on the examining table. Voluntary and involuntary guarding and abdominal distention are common. Elicitation of a positive Murphy sign is helpful. Ultrasonography is the most commonly used radiological test. Treatment is early cholecystectomy.11
Gonadal torsion, caused by faulty fixation of the testis to the scrotum, can present with acute excruciating lower abdominal or scrotal pain, nausea, and vomiting. The condition usually affects young boys but may affect male patients of any age. It is a urologic emergency. If not treated promptly, constriction of the vascular supply may lead to ischemia and necrosis of the testis.12


