Peer Reviewed
Abdominal Pain in an Adolescent Girl
Correct answer: D. Ovarian mass
A dedicated pelvic ultrasonograph subsequently demonstrated a large, simple-appearing cystic mass measuring 21 cm × 26 cm closely associated with the left adnexa (Figure 2). Doppler flow demonstrated no appreciable blood flow within the mass. The right ovary, uterus, spleen, liver, and kidneys appeared normal. A gynecologist was consulted for management.
Patient Course. The patient was admitted to the gynecology service directly from the ED. Laboratory assessment—including the following tumor markers: lactate dehydrogenase, carcinoembryonic antigen, α-fetoprotein, β-hCG, inhibin B, and cancer antigen-125—as well as magnetic resonance imaging (MRI) of abdomen and pelvis with and without contrast were conducted to better categorize the mass. Levels of the tumor markers were within normal limits.
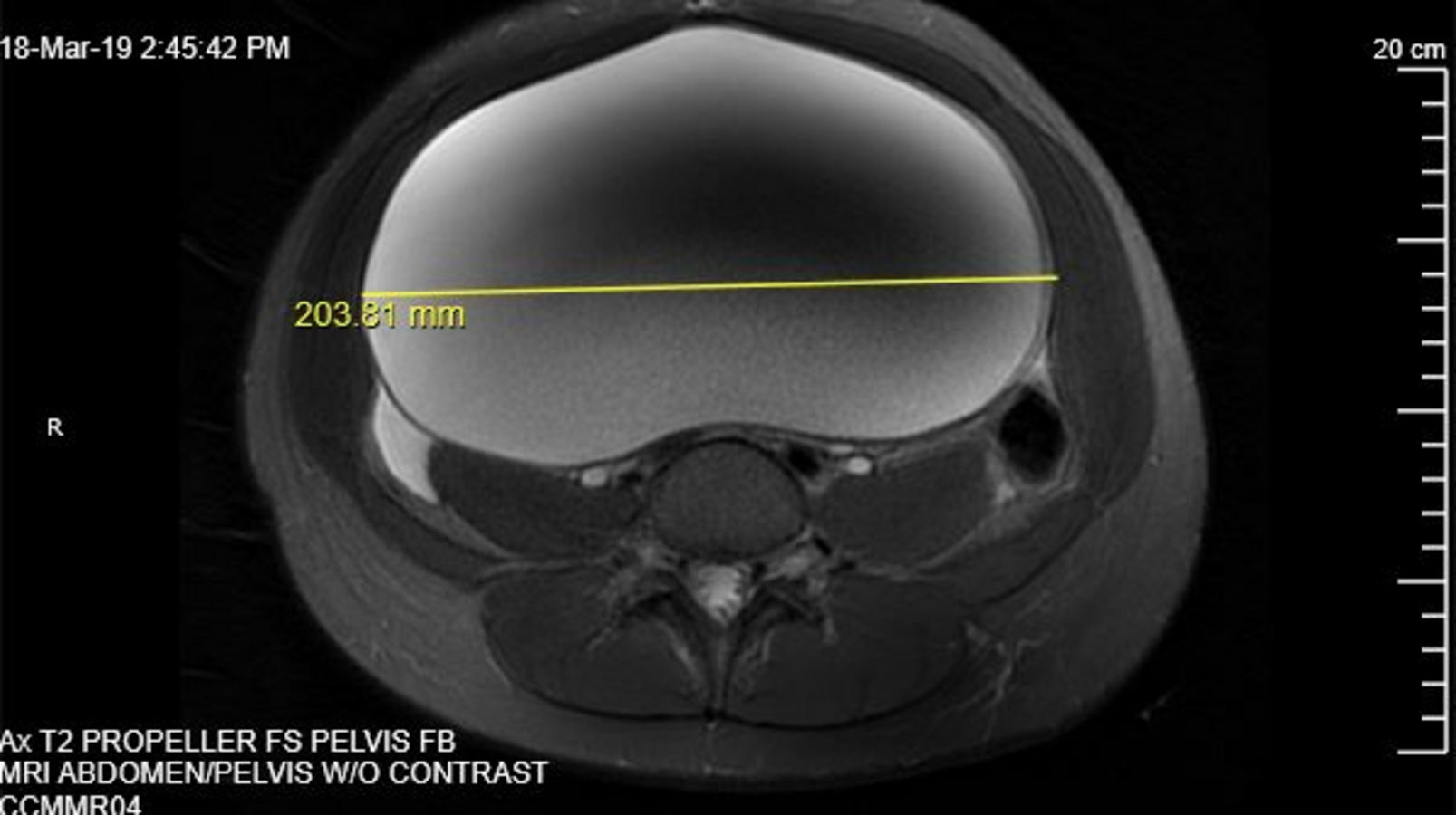
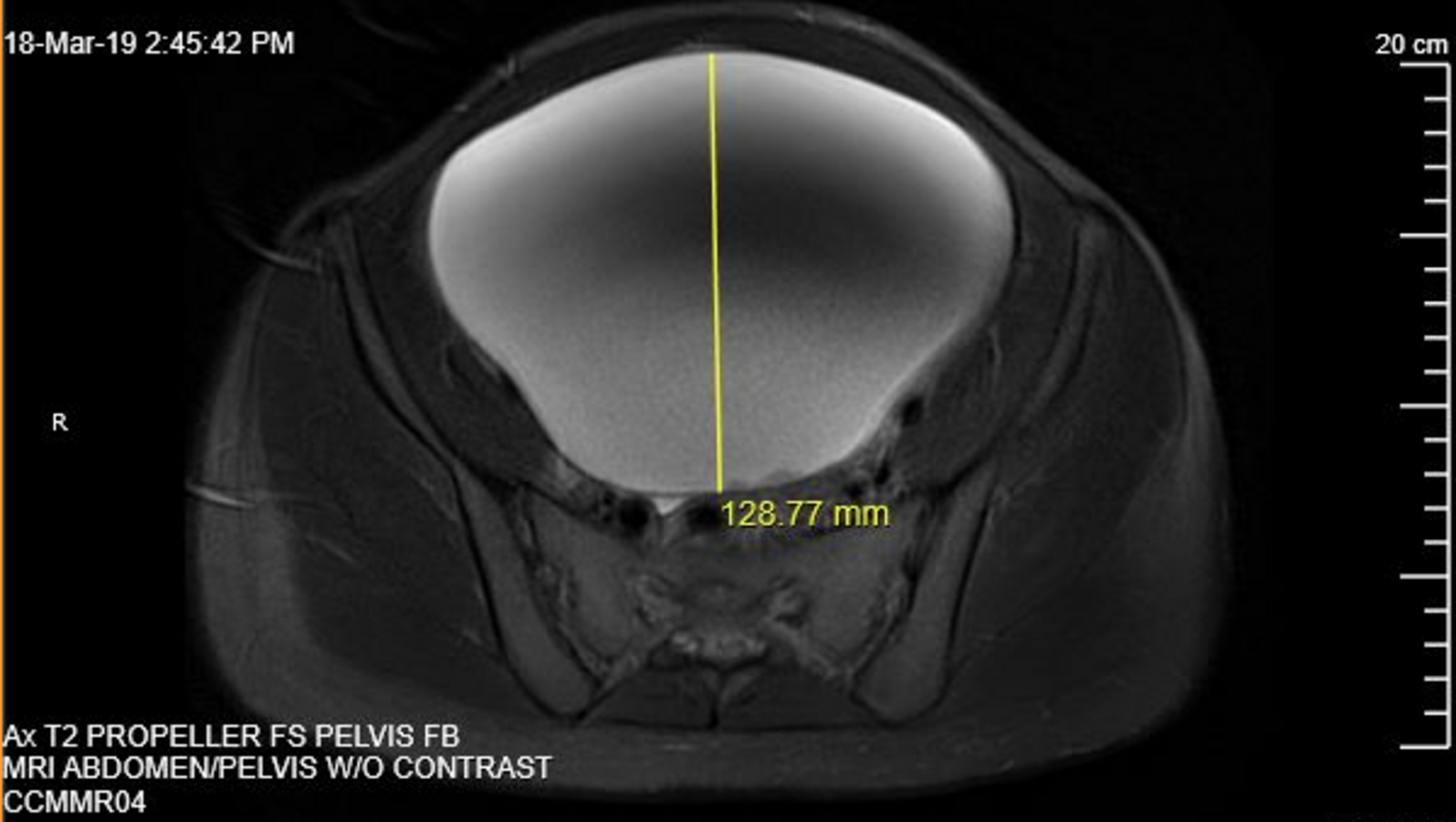
The mass appeared as a unilocular cyst with smooth contours, suggesting a benign etiology (Figures 3 and 4). No evidence of acute urinary or bowel obstruction was noted. A chest radiography scan was also conducted, results of which did not show evidence of metastatic disease. Ovary-sparing surgical excision of the cyst was conducted. The patient’s post-operative course was uneventful, and she was discharged home on post-operative day 2.


Pathology results revealed the presence of granulosa cell tumor of the left ovary. After the gynecologist consulted with an oncologist, radiologist, and pathologist, the patient also underwent a left salpingo-oophorectomy, peritoneal biopsy, and partial omentectomy, which she tolerated well. No evidence of tumors existed in the most recent pathology specimens.
Patient outcome. She continues to be monitored by the oncologist and has no evidence of residual or recurrent disease based on follow-up tumor markers and repeat MRI scans and has no evidence of lung metastases on repeat chest radiography. She denies new pain, nausea, vomiting, constipation, diarrhea, or changes in appetite or weight and has no issues with urination or stooling. Her menses have resumed and are now regular.
On follow-up one year later, she has returned to school and participates in cheerleading. Her school uniform now fits correctly.
Discussion. The differential diagnosis for acute-on-chronic abdominal pain in this adolescent girl was broad. The patient had no signs or symptoms to suggest acute surgical cause for pain, given the absence of fever, vomiting, bloody diarrhea, lack of bowel sounds, rebound tenderness, or voluntary guarding. Constipation, hernia, and infectious causes of pain, including gastroenteritis and urinary tract infection, were considered. Other gynecologic problems including pelvic inflammatory disease, ovarian cysts, ovarian torsion, and ovarian masses were also included in our differential.
Ovarian masses are unusual findings in adolescent girls, with the majority of masses presenting as physiologic cysts or benign lesions. Although rare, this diagnosis should be considered for adolescent girls with abdominal pain and a palpable mass, as approximately 10% of ovarian masses are malignant.1-4 Early recognition of an ovarian mass is important because of the increased risk for torsion when the mass is larger than 5 cm. Similarly, prompt identification can improve outcomes for malignant lesions. Classification of the mass based on tumor markers and imaging is, therefore, critical to ensure the appropriate management for treatment and fertility preservation.1-4
The presentation of abdominal pain and a palpable mass in adolescent girls should elicit a comprehensive workup for a broad differential diagnosis given the possibility for malignancy. Abdominal ultrasound should be the primary imaging modality utilized to evaluate and characterize the size, location, origin, and consistency (ie, solid or cystic) of a mass because of its accessibility and lack of ionizing radiation. Doppler flow should also be conducted to understand the blood supply to the mass.
Laboratory studies vary with clinical features of the mass and might include the following tumor markers: lactate dehydrogenase, carcinoembryonic antigen, α -fetoprotein, β-hCG, inhibin B, and cancer antigen-125. However, negative tumor markers do not eliminate the risk of malignancy and should be interpreted in conjunction with imaging. A pregnancy test should also be administered to determine pregnancy status and rule out an ectopic pregnancy. Treatment for ovarian masses typically requires surgical excision of the lesion, with the goal of ovarian preservation if possible. If malignancy is suspected based on the aforementioned imaging and laboratory assessment, adequate staging of the mass is necessary to improve prognosis.1-4
Conclusions. Although uncommon, ovarian masses should remain on the differential for abdominal pain in adolescent girls to decrease the risk of torsion and improve outcomes associated with malignancy. Ultrasonography scanning is the preferred method of initial imaging for a suspected ovarian mass given its availability and safety but can be augmented with MRI for better categorization of the mass, while chest radiography scanning is important to determine presence of metastatic disease. Laboratory assessment is also useful to guide management. However, laboratory findings and imaging should supplement a thorough physical examination. Conflicting findings should trigger a reassessment and expansion of the existing differential diagnosis.
1. Zhang M, Jiang W, Li G, Xu C. Ovarian masses in children and adolescents - an analysis of 521 clinical cases. J Pediatr Adolesc Gynecol. 2014;27(3):e73-e77. https://doi.org/10.1016/j.jpag.2013.07.007
2. Strickland J, Laufer MR. Adnexal masses. In: Emans SJ, Laufer MR, DiVasta A, eds. Emans, Laufer, Goldstein's Pediatric and Adolescent Gynecology. 7th ed. Wolters Kluwer, 2019;529-547.
3. Mahajan P, Weldon CB, Frazier AL, Laufer MR. Gynecologic cancers in children and adolescents. In: Emans SJ, Laufer MR, DiVasta A, eds. Emans, Laufer, Goldstein's Pediatric and Adolescent Gynecology. 7th ed. Wolters Kluwer, 2019;556-574.
4. Heo SH, Kim JW, Shin SS, et al. Review of ovarian tumors in children and adolescents: radiologic-pathologic correlation. Radiographics. 2014;34(7):2039-2055. https://doi.org/10.1148/rg.347130144