Peer Reviewed
Uveal Melanoma
Authors:
Candice Short, DNP, FNP-C
East Tennessee State University, Johnson City, Tennessee
Ryan Short, MSN, FNP-BC
Alleghany Health Services, Sparta, North Carolina; Hugh Chatham Family Medicine, Elkin, North Carolina
Citation:
Short C, Short R. Uveal melanoma. Consultant. 2019;59(10):317-319.
Approximately 1 week after having been shot in the left eye with a foam dart from a toy gun, a 37-year-old woman presented to an optometrist due to persistent pain in the eye. The patient received a diagnosis of iritis with trace flare of the left eye and was treated with prednisolone acetate ophthalmic drops, 1%, 1 drop in the left eye 4 times daily for 1 week, then 1 drop 3 times daily for 3 days, then 1 drop twice daily for 3 days, then 1 drop daily for 3 days, and then discontinued.
The patient had a known history of a benign nevus of the right iris. During the eye examination, the optometrist, who had been following the patient’s case, noted that the nevus was brown and circumscribed with a flat anterior contour, but it appeared to have enlarged (Figure 1).
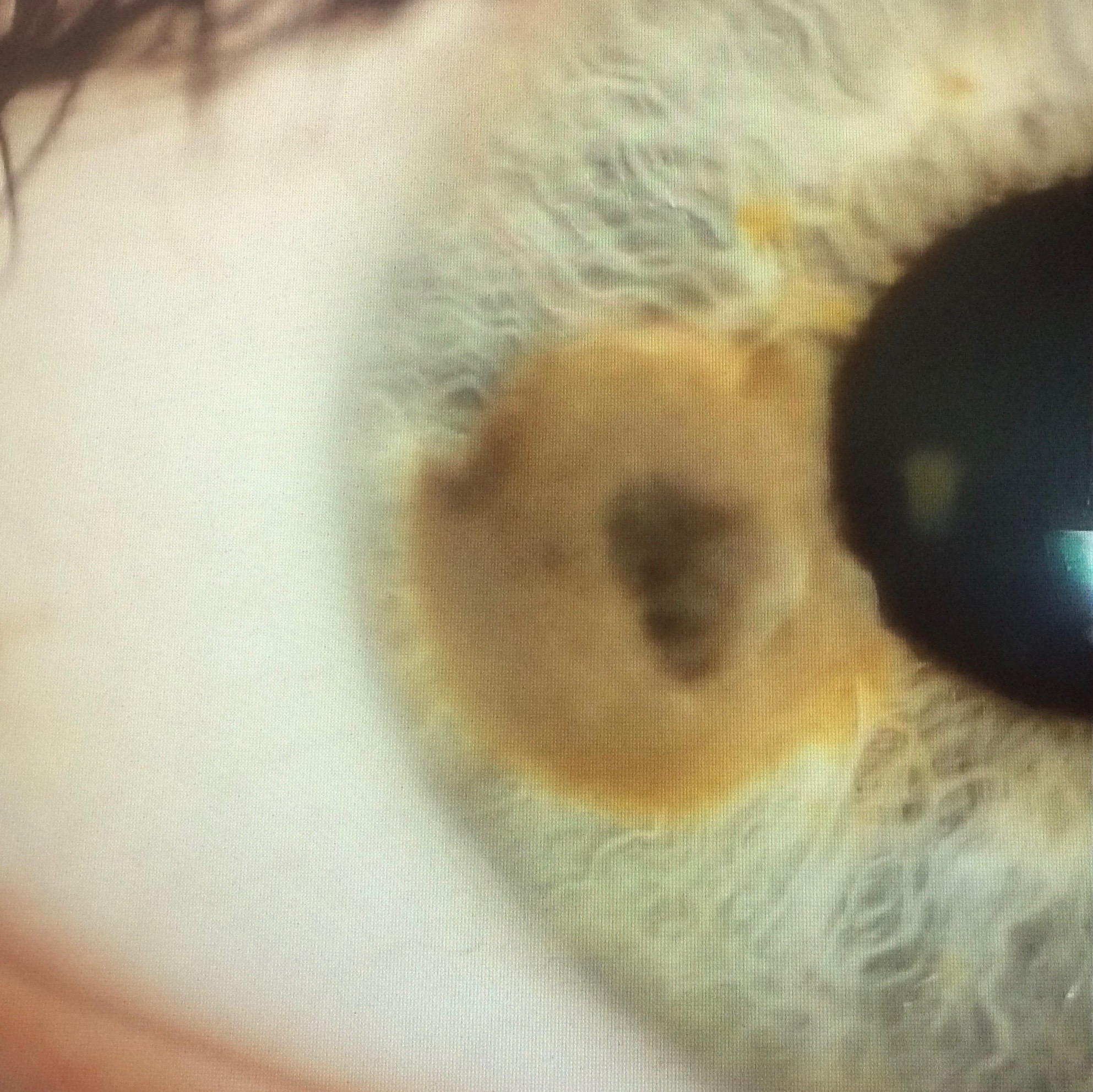
Figure 1. At presentation, the patient’s iris nevus was brown and circumscribed with a flat anterior contour.
The woman’s last documented eye examination, approximately 2 years prior, stated that she had mild elevation of the nevus. Mild elevation of the nevus had been first documented more than 20 years prior. Upon further questioning, the patient recalled that several friends had commented recently about the enlarged size of the brown spot in her right eye. The patient reported no other visual changes or concerns at that time.
Physical examination. On visual examination, the patient was suspected to have more than minimal elevation of the lesion. She was immediately referred to an ophthalmologist, who agreed that the lesion’s size was concerning and referred her to an ocular oncologist. The ocular oncologist ordered transverse ocular ultrasonography. The patient was found to have a significant elevation of 1.65 mm of the lesion in her right iris.
Based on the results of the clinical examination, the patient received a diagnosis of a uveal melanoma arising from the iris. Pathology tests are not required for a definitive diagnosis of a uveal melanoma; clinical diagnostic accuracy was found to exceed 99% in the Collaborative Ocular Melanoma Study for eyes surgically enucleated.1 Nevertheless, the patient expressed a desire to have a biopsy to determine staging and metastasis risk. The biopsy was completed during treatment with the plaque brachytherapy.
Discussion. Uveal melanoma is a malignancy in the uveal tract of the eye. Uveal melanoma typically arises from the choroidal melanocytes (85%-90% of cases) but can arise from the iris (3%-5%) or the ciliary body (5%-8%).2 The reported incidence of primary uveal melanoma is 5.2 cases per million per year in the United States.3 Representing the most common primary intraocular malignancy, uveal melanoma makes up 5% of all recorded melanomas in the United States.4 The average age of persons diagnosed with uveal melanoma is 41 years.3
Risk factors for uveal melanoma include fair skin, light eyes, an inability to tan, dysplastic nevus syndrome, and BAP1 mutation.5-7 The role of ultraviolet radiation is unclear in the development of uveal melanoma, unlike with cutaneous melanoma.7
The most common symptom associated with uveal melanoma is blurred vision, followed by photopsia, floaters, loss of visual fields, visible lesion, pain, and metamorphopsia.8 Often a patient presents with no symptoms, and discovery is made incidentally.8
The diagnosis is made by distinguishing symptomatology, patient history, and clinical evaluation.9 Other tests may be performed to confirm the diagnosis, including ocular ultrasonography, fundus fluorescein angiography, indocyanine green angiography, optical coherence tomography, fundus autofluorescence, ultrasound biomicroscopy, and biopsy.9
This malignancy is typically diagnosed early based on clinical presentation and progression of the disease; however, the consequences of treatment can often lead to significant visual disturbances.2 Metastatic progression is common, leading to a poor prognosis.2 Metastasis risk has been associated with tumor size.9 It is estimated that up to 50% of patients with uveal melanoma eventually will have metastatic disease, with the liver being the leading site, followed by lung, skin, and bone, respectively.10 The reported 5-year survival rate is 69%, and the 15-year survival rate is 55%.11 In some cases, a biopsy may be performed to determine staging of the lesion and look for metastatic markers such as BAP1 and PRAME.
Differential diagnosis. Several other lesions may mimic a uveal melanoma, including primary iris cysts, iris nevus, essential iris atrophy, foreign body, peripheral anterior synechia, and secondary metastasis.2 If the diagnosis is uncertain, ultrasound biomicroscopy of the anterior segment is recommended to measure lesion thickness.12 Tissue confirmation is not required to make a definitive diagnosis; however, if questions arise regarding the diagnosis, an intraocular biopsy using fine-needle aspiration or incisional biopsy may be performed.13
Treatment. In some minor cases, the lesion is monitored for growth and change.14 Surgical excision may be performed in lesions with documented enlargement to preserve visual acuity.15 Our patient was treated with plaque brachytherapy, which is the most widely used treatment.14 A gold plaque was sewn onto the patient’s iris for 5 days and then removed (Figures 2 and 3). A few new treatment options are in various stages of approval by the Food and Drug Administration. One such treatment is light-activated AU-011, which is virus-like drug for the treatment of primary uveal melanoma.14 Another investigational treatment, tebentafusp, is proving effective in clinical trials at increasing survival rates in metastatic uveal melanoma.16

Figure 2. Plaque brachytherapy treatment of the patient, during which a gold plaque was sewn onto the iris.

Figure 3. The patient’s eye 6 days after removal of the gold plaque.
Upon removal of the plaque, the patient was discharged with instructions to apply atropine sulfate drops, 1%, 1 drop every morning for 4 weeks, and tobramycin and dexamethasone ophthalmic ointment 4 times daily for 1 week, then 3 times daily for 1 week, then twice daily for 1 week, then once daily for 1 week. Combination drops and ointments are prescribed to reduce inflammation and prevent postoperative infection. There is no gold standard treatment for uveal melanoma.15 Treatment is standardized to the patient. Other treatment modalities include enucleation, laser therapy, and other forms of radiation.2
Outcome of the case. The patient was evaluated at 5 weeks postoperatively and was found to have visual acuity of 20/20. The patient’s only complaint was some vision cloudiness, erythema, and mild ptosis 3 months posttreatment (Figure 4).

Figure 4. The patient’s eye approximately 3 months posttreatment.
At a 5-month follow-up visit, the lesion had decreased in size from 1.65 mm to 1.28 mm, which represented a significant reduction in the tumor size. The patient is expected to fully recover. She will require biannual computed tomography scans of the chest and abdomen for at least 5 years to monitor for metastasis. Because she tested negative for BAP1 and PRAME markers, the estimated risk of metastasis is less than 1%. Potential negative outcomes reported by the ocular oncologist for the patient included development of a cataract, metastasis, and vision loss from radiation retinopathy due to the radiation exposure.
References:
- Accuracy of diagnosis of choroidal melanomas in the Collaborative Ocular Melanoma Study: COMS Report No. Arch Ophthalmol. 1990;108(9):1268-1273.
- Krantz BA, Dave N, Komatsubara KM, Marr BP, Carvajal RD. Uveal melanoma: epidemiology, etiology, and treatment of primary disease. Clin Ophthalmol. 2017;11:279-289.
- Aronow ME, Topham AK, Singh AD. Uveal melanoma: 5-year update on incidence, treatment, and survival (SEER 1973-2013). Ocul Oncol Pathol. 2018;4(3):145-151.
- Francis JH, Shoushtari AN, Baker CA, Abramson DH. Uveal melanoma: diagnosis, prognosis and current treatments for primary and metastatic disease. Melanoma Lett. 2016;34(3):1- https://www.skincancer.org/publications/the-melanoma-letter/fall-2016-vol-34-no-3/uveal-melanoma. Accessed August 9, 2019.
- Ocular melanoma. National Organization for Rare Disorders. https://rarediseases.org/rare-diseases/ocular-melanoma/. Published 2018. Accessed August 9, 2019.
- Harbour JW, Onken MD, Roberson EDO, et al. Frequent mutation of BAP1 in metastasizing uveal melanomas. Science. 2010;330(6009):1410-1413.
- Weis E, Shah CP, Lajous M, Shields JA, Shields CL. The association between host susceptibility factors and uveal melanoma: a meta-analysis. Arch Ophthalmol. 2006;124(1):54-60.
- Damato EM, Damato BE. Detection and time to treatment of uveal melanoma in the United Kingdom: an evaluation of 2384 patients. Ophthalmology. 2012;119(8):1582-1589.
- Tarlan B, Kıratlı H. Uveal melanoma: current trends in diagnosis and management. Turk J Ophthalmol. 2016;46(3):123-137.
- Rietschel P, Panageas KS, Hanlon C, Patel A, Abramson DH, Chapman PB. Variates of survival in metastatic uveal melanoma. J Clin Oncol. 2005;23(31):8076-8080.
- Kujala E, Mäkitie T, Kivelä T. Very long-term prognosis of patients with malignant uveal melanoma. Invest Ophthalmol Vis Sci. 2003;44(11):4651-4659.
- Henderson E, Margo CE. Iris melanoma. Arch Pathol Lab Med. 2008;132(2):268-272.
- Shields CL, Manquez ME, Ehya H, Mashayekhi A, Danzig CJ, Shields JA. Fine-needle aspiration biopsy of iris tumors in 100 consecutive cases: technique and complications. Ophthalmology. 2006;113(11):2080-2086.
- Kaliki S, Shields CL. Uveal melanoma: relatively rare but deadly cancer. Eye (Lond). 2017;31(2):241-257.
- Conway RM, Chua WC-T, Qureshi C, Billson FA. Primary iris melanoma: diagnostic features and outcome of conservative surgical treatment. Br J Ophthalmol. 2001;85(7):848-854.
- Connelly S. Novel immunotherapy tebentafusp granted fast track designation for metastatic uveal melanoma. Targeted Oncology. https://www.targetedonc.com/news/novel-immunotherapy-tebentafusp-granted-fast-track-designation-for-metastatic-uveal-melanoma. Published April 11, 2019. Accessed August 9, 2019.


