Peer Reviewed
A Rare Case of Congenital Radioulnar Synostosis
A 6-year-old girl was brought to our clinic by her parents with the inability to supinate both upper extremities. Her mother had noticed that the patient could not retain powdered substances in her palms from an early age. The mother had compared the patient’s arm movements to her biological brother’s and observed the differences.
The mother denied any trauma to the area, family history of similar problems, or skeletal abnormalities. The patient denied pain at the elbow.
Physical examination. The patient was generally healthy, except she could only supinate her forearms past 60° actively and passively. A compensatory movement of her shoulder region with passive supination was observed. Full range of motion was present in other directions.
Some mild tenderness was noted upon deep palpation of the lateral elbow. The patient also had clinodactyly of the fifth phalange bilaterally. No other skeletal abnormalities were noted. A 3-view radiography scan of the elbow was conducted, results of which showed bilateral radioulnar synostosis (Figures 1-4). No wrist abnormalities were identified.

Figure 1. A radiology scan of the patient’s upper left extremity, lateral view.

Figure 2. A radiology scan of the patient’s upper left extremity, medial view.

Figure 3. A radiology scan of the patient’s upper right extremity, lateral view.

Figure 4. A radiology scan of the patient’s upper right extremity, medial view.
Discussion. Congenital radioulnar synostosis is rare, with only about 350 cases identified worldwide.1 The average age at diagnosis is about 6 years, which is typically the age when children start attending school and having more physical activity demands.2 In 60% of cases, congenital radioulnar synostosis occurs bilaterally, and 9% are familial cases.3 It is also believed to be related to an abnormality of chromosome X, but cases related to an abnormal chromosome Y have also been reported.3 There appears to be no difference in incidence between boys and girls, but some authors have described a male predominance.4-7
At about 4 weeks gestation, the upper extremity emerges from an unsegmented body wall. Initially, the ulnar and radius share a common perichondrium, which must be separated in a short time.8 Congenital radioulnar synostosis occurs when there is failure of segmentation of the adjacent radius and ulna at the seventh week of development. Typically, patients will accommodate and learn to live with the condition. However, because of compensatory strain at the shoulder, elbow, and wrist joint, patients may have pain at compensating joints. Congenital radioulnar synostosis has been associated with musculoskeletal (ie, polydactyly, syndactyly, joint laxity), gastrointestinal, renal, cardiac, hematologic, and neurological disorders.2,9 Our patient presented with only one other isolated abnormality, clinodactyly.
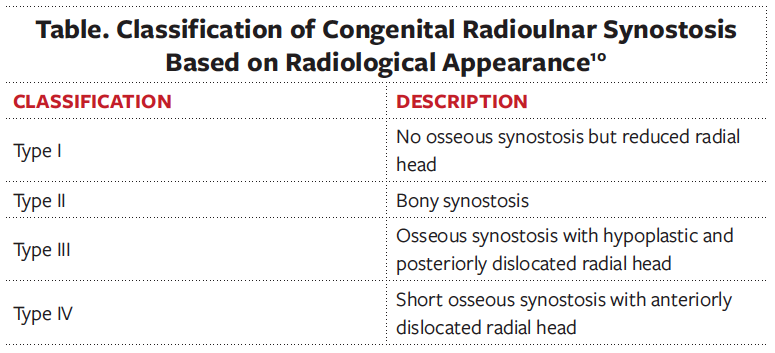
CRUS has been described based on radiological classifications, the anatomical location of synostosis, and how it influences functionality. The most common radiological classification of CRUS, described by Cleary and Omer, is based on the appearance of the synostosis and reduction of the radial head (Table).6,10 Type I occurs with no osseous synostosis but a reduced radial head. Type II occurs with bony synostosis. Type III occurs with osseous synostosis with a hypoplastic and posteriorly dislocated radial head. Type IV occurs with short osseous synostosis with an anteriorly dislocated radial head. The radiological findings in our patient depicts a type II congenital radioulnar synostosis (Figure 1). Another description was explained by Wilkie, for which type I shows a connection between the radius and ulna occurs at the medullary canal; with type II, the fusion occurs distal to the proximal radial epiphysis and the radial head is dislocated anteriorly or posteriorly.4 A third description, which pertains to just the proximal radioulnar synostosis has also been portrayed.11 In type I, there is an absence of the radial head followed by complete radioulnar synostosis. In type II, the proximal part of the radial head is present but often deformed, and fusion occurs at the neck of the ulna. In type III, the head of the radius is always deformed and subluxed with synostosis occurring at the proximal area of the interosseous bones.
When the disease is mild, conservative therapy via physiotherapy, occupational therapy, activity modification, and ergonomic working environment are beneficial.12 Functionality will improve, but range of motion may remain unchanged.13 Derotational osteotomy could be conducted in patients with severe or debilitating disease but often has poor outcomes, primarily because of a poorly developed supporting structure, risk of compartment syndrome, and recurrence of synostosis.13
Patient outcome. Our patient was referred for physical therapy. The patient’s mother was educated regarding the anomaly and was advised to return if improvement was not made.
Conclusion. Congenital radioulnar synostosis can present as an isolated anomaly that can easily be missed. It can be treated conservatively if no functional impairment presents. However, with less than 60° of impairment in pronation, there may be significant impairment, which may require surgical correction. One also needs to be aware of comorbidities that may be present.
AFFILIATION:
Texas Tech University Health Sciences Center, Lubbock, Texas
CITATION:
Okotcha E, Goldfinger M, Bell T, Griffin A. A rare case of congenital radioulnar synostosis. Consultant. 2022;62(6);e14-e16. doi:10.25270/con.2021.11.00004
Received May 16, 2021. Accepted June 16, 2021. Published online November 15, 2021.
DISCLOSURES:
The authors report no relevant financial relationships.
CORRESPONDENCE:
Efe Okotcha, MD, Texas Tech University Health Sciences Center, 1400 South Coulter Street, Amarillo, TX 79106 (Efe.okotcha@gmail.com)
1. Tsai J. Congenital radioulnar synostosis. Radiol Case Rep. 2017;12(3):552-554. https://doi.org/10.1016/j.radcr.2017.03.011
2. Alagbe OA, Oyekale OI, Adeniyi TO. A case report of congenital bilateral proximal radioulnar synostosis in a 22-month-old child. West Afr J Radiol. 2019:26(1):50. doi:10.4103/wajr.wajr_57_17
3. Siemianowicz A, Wawrzynek W, Besler K. Congenital radioulnar synostosis - case report. Pol J Radiol. 2010;75(4):51-54. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3389900/
4. Jia Y, Geng C, Song Z, Lv S, Dai B. Congenital unilateral proximal radioulnar synostosis: a surgical case report. Medicine (Baltimore). 2020;99(16):e19782. https://doi.org/10.1097/md.0000000000019782
5. Prokopovich EV, Konev MA, Afonichev KA, et al. Congenital radioulnar synostosis: symptom complex and surgical treatment. Pediatr Traumatol Orthop Reconstr Surg. 2016;4(3):16-25. https://doi.org/10.17816/PTORS4316-25
6. Hosni S, Hanine D, El Alami SZF, Madhi T. Congenital radio-ulnar synostosis (about 7 cases). J Med Case Rep. 2018:6(18):763-768. doi:10.21276/sjmcr.2018.6.10.9
7. Fakoor M. Radioulnar synostosis in a father and his 5-year-old daughter. Pak J Med Sci. 2006:22(2):191-193. https://pjms.com.pk/issues/aprjun06/article/casereport1.html
8. Iyoko IK, Iyoko II, Essien MA, Henshaw JE. Congenital proximal radioulnar synostosis-a case report. Radiol Case Rep. 2020;15(8):1313-1316. https://doi.org/10.1016/j.radcr.2020.05.070
9. Qari, RM, Aljaouni SK. Congenital bilateral radioulnar synostosis with acute lymphoblastic leukemia: a case report. J Appl Hematol. 2016:8(1):37-38. doi:10.4103/joah.joah_49_16
10. Cleary JE, Omer GE Jr. Congenital proximal radio-ulnar synostosis. Natural history and functional assessment. J Bone Joint Surg Am. 1985;67(4):539-545. https://journals.lww.com/jbjsjournal/Abstract/1985/67040/Congenital_proximal_radio_ulnar_synostosis_.6.aspx
11. Martínez Estupiñan CLM, Martínez Aparicio L, Martínez Aparicio L, Morales Piñéiro S. Congenital radioulnar synostosis. Clin Med Health Res J. 2021;1(1):26-28. http://cmhrj.com/index.php/cmhrj/article/view/14
12. Kepenek-Varol B, Hoşbay Z. Is short-term hand therapy effective in a child with congenital radioulnar synostosis? A case report. J Hand Ther. 2020;33(3):435-442. https://doi.org/10.1016/j.jht.2019.03.009
13. Pei X, Han J. Efficacy and feasibility of proximal radioulnar derotational osteotomy and internal fixation for the treatment of congenital radioulnar synostosis. J Orthop Surg Res. 2019;14(1):81. https://doi.org/10.1186/s13018-019-1130-0


