Peer Reviewed
A Case of Menopause-Induced Angioedema
Abstract. Angioedema is a painless, non-pitting, localized edema that occurs within the deep layers of the skin. There are known genetic differences that influence angioedema, and the attacks have been linked to sex hormones. Angioedema can emerge, or be exacerbated, during heightened estrogen states like pregnancy or with the use of contraception. However, this case report describes multiple attacks of angioedema emerging perimenopause. Although there are few, if any, case reports related to angioedema during a period of declining estrogen, clinicians should still consider the role of hormonal changes when evaluating disease states, particularly when concluding that an illness is idiopathic in nature.
Introduction. Angioedema is a painless, non-pitting, localized edema that occurs within the deep layers of the skin, subcutaneous, mucosal, and subcutaneous tissue.1,2 It can include several areas of the body including the face, oral cavity, and extremities.1,2 Angioedema attacks can be the result of allergen exposures, acquired blood protein deficiencies, genetic disorders, or idiopathic origins.1-4 However, there are a growing number of reports3-10 regarding the role of female hormones in such attacks, particularly among studies on hereditary angioedema where high estrogen states, like pregnancy, puberty, or the use of exogenous hormones can exacerbate such attacks.3-7 However, there is less attention given to the imbalanced hormonal fluctuations during perimenopause that can also alter immune system reactions.
This case report describes multiple attacks of angioedema that emerged during the onset of perimenopause. There is no known case report in the literature discussing angioedema associated with perimenopause. This case report is a reminder of the delicate relationship between female sex hormones and immunology. Indeed, clinicians should consider the role of hormonal fluctuations when evaluating disease, particularly when suspected to be idiopathic in nature.
A 49-year-old woman with a history of hypothyroidism and allergic rhinitis presented to the emergency room with swelling of the left and lower eyelids (Figure 1). According to the patient, there was no pain or change in vision.

Figure 1. An angioedema can be seen on the left upper and lower eyelid.
Patient history. The patient noted that this was one of several episodes of angioedema that occurred within 60 minutes of food ingestion. The attacks began with the onset of perimenopause and occurred throughout the body. She reported that swellings (Figure 2) erupted in the groin, hands, feet, and neck, but most commonly in the face (Figure 3). There is no family history of persons with attacks of angioedema. However, the patient’s mother has been treated for allergic rhinitis.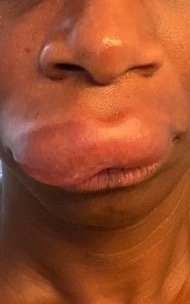
Figure 2. An angioedema of the upper lip is shown.

Figure 3. An angioedema of the lower lip is shown.
Physical examination. The left upper and lower eyelids were engorged with a non-pitting edema preventing opening of the eye. The emergency room physician noted there was no erythema, warmth, discoloration, tenderness, induration or discharge. Complete blood count and comprehensive metabolic panel were drawn, all within normal limits.
Differential diagnosis. In this case, the differential diagnoses should include ailments of infectious and allergic origin such as blepharitis, cellulitis, styes, contact dermatitis, and conjunctivitis. The patient’s physical examination and history supported the diagnosis of angioedema, acute in nature, and most likely due to food allergens.
Treatment and management. Intravenous famotidine and oral diphenhydramine 50 mg were administered during the emergency room stay. An allergist referral and prescriptions for prednisone 20 mg daily for 5 days and diphenhydramine 25 mg 3 times daily as needed were provided at discharge.
Outcome and follow-up. Skin prick test was negative during follow up with the allergist. Additional laboratory work produced normal levels of C1-inhibitor protein and function, C4, C1q, antinuclear antibody, erythrocyte sedimentation rate and thyroid function tests. The allergist reported extremely rare cases where perimenopause can decrease the threshold for allergic reactions. He recommended maintenance of a food diary as the best means of avoiding foods that could trigger the attacks. The patient’s symptoms are currently controlled with a strict diet of non-processed foods as well as lean meats, fish, fruits, and vegetables. Diphenhydramine 12.5-25 mg nightly is also used as needed.
Discussion. Angioedema—a painless, non-pitting, localized edema that occurs within the deep layers of the skin—is generally found on the face, oral cavity, and extremities.1,2 Although angioedema attacks can be the result of allergen exposures, acquired blood protein deficiencies, genetic disorders or idiopathic origins,1-4 there are a growing number of studies on the role of female hormones in such attacks due to an imbalance of hormonal fluctuations during perimenopause that can alter immune system reactions.3-10
Estrogen can trigger immunoregulatory processes that occur in response to an allergen including mast cell degranulation of histamine.4-9 Estrogen also inhibits diamine oxidase, an enzyme that degrades histamine in the gastrointestinal tract.12-13 Histamine itself also plays a role in estrogen production and maintenance.14 Consequently the two molecules develop a cycle of imbalance due to erratic estrogen surges during perimenopause.14 The accumulation of histamine can create histamine intolerance, the most likely cause of these recurrent attacks of angioedema.15,16 It should be noted that selective serotonin reuptake inhibitors, soy products, and exogenous estrogens are also recommended to reduce perimenopausal symptoms but they can worsen the histaminergic response. Hypothyroidism can also pose an increased risk for inflammatory allergic responses.17 The reduction of symptoms due to dietary changes is diagnostic for histamine intolerance.
Perimenopause is an inevitable period in a woman’s life and the effects of hormonal imbalance require more attention. The alterations to the body’s homeostasis should not be dismissed as a few uncomfortable symptoms only to be discussed with a gynecologist. These hormonal fluctuations are affecting other organ systems and a few additional questions within the patient-provider dialogue could decrease misdiagnosis, lower the rates of idiopathic disease, and provide more insight into the role of hormones in a woman’s life cycle.
- Misra L, Khurmi N, Trentman T. Angioedema: classification, management and emerging therapies for the perioperative physician. Indian J Anaesth. 2016;60(8):534-554. doi: 10.4103/0019-5049.187776
- Bernstien J, Moellman J. Emerging concepts in the diagnosis and treatment of patients with undifferentiated angioedema. Int J Emerg Med. 2012;5(1):39. doi: 10.1186/1865-1380-5-39.
- Banerji A, Riedl M. Managing the female patient with hereditary angioedema. Women’s Health. 2016;12(3):351-361 doi:10.2217/whe.16.6
- Mcglinchey P, Mccluskey D. Hereditary angioedema precipitated by estrogen replacement therapy in a menopausal woman. Am J Med Sci. 2000;320(3):212-213. doi: 10.1097/00000441-200009000-00014.
- Bernstien J, Bouillet L, Caballero T, Staevska M. Hormonal effects on urticaria and angioedema conditions. J Allergy Clin Immunol. 2021;9(6): 2209-2219. doi:10.1016/j.jaip.2021.04.021
- Hentges F, Hilger C, Kohnen M, Gilson G. Angioedema and estrogen-dependent angioedema with activation of the contact system. J Allergy Clin Immunol. 2009;123(1):262-264. doi:10.1016/j.jaci.2008.10.056
- Bouillet L. Hereditary angioedema in women. Allergy Asthma Clin Immunol. 2010;6(1):17. doi:10.1186/1710-1492-6-17
- Taneja V. Sex hormones determine immune response. Front Immunol. 2018;9:1931. doi:10.3389/fimmu.2018.01931
- Bonds RS, Midoro-Horiuti T. Estrogen effects in allergy and asthma. Curr Opin Allergy Clin Immunol. 2013;13(1):92-99. doi:10.1097/ACI.0b013e32835a6dd6
- Fan Z, Che H, Yang S, Chen C. Estrogen and estrogen receptor signaling promotes allergic immune responses: Effects on immune cells, cytokines, and inflammatory factors involved in allergy. Allergol Immunopathol (Madr). 2019;47(5):506-512. doi:10.1016/j.aller.2019.03.001
- Seeman M. Developing effective strategies for women with schizophrenia. Psychiatric Times. 2023;40:33-34.
- Schnedi W, Schenk M., Lackner S, Enko D, et al. Diamine oxidase supplementation improves symptoms in patients with histamine intolerance. Food Science Biotechnology. 2019;28(6):1779-1784. doi: 10.1007/s10068-019-00627-3
- Szelag A, Lad A, Trocha M. Histamine receptors in the female reproductive system. Part 1. Role of mast cells and histamine in the reproductive system. Ginekologia Polska. 2002;73(7):627-635.
- Fogel W. Diamine oxidase (DAO) and female sex hormones. Agents Actions. 1986;18(1-2):44-45. doi: 10.1007/BF01987978
- Hrubisko M, Danis R, Huorka M. Histamine Intolerance-the more we know the less we know. A review. Nutrients. 2021;12(7) 2228. doi:10.3390/nu13072228
- Baste, O, Perez S, Nogues M. Histamine Intolerance: the current state of the Art. Biomolecules: 2020;10(8):1181. doi:10.3390/biom10081181
- Perez S, Baste O, Nogues M, et al. Low histamine diets: is the exclusion of foods justified by their histamine content. Nutrients. 2021;13(5):1395. doi: 10.3390/nu13051395
AUTHOR:
Tobechukwu A. Clouden, MD, MPH1
AFFILIATIONS:
1Medical Director, Riverview Medical Center Adult Outpatient Behavioral Health, Shrewsbury, NJ
CITATION:
Clouden TA. A case of menopause-induced angioedema. Consultant. Published online October 1, 2024. doi:10.25270/con.2024.10.000002
Received January 22, 2024. Accepted July 17, 2024
DISCLOSURES:
The authors report no relevant financial relationships
ACKNOWLEDGEMENTS:
None.
CORRESPONDENCE:
Tobechukwu A. Clouden, MD, MPH, Riverview Medical Center Adult Outpatient Behavioral Health 661 Shrewsbury Avenue, Shrewsbury, NJ 07702 (tobechukwu.clouden@hmhn.org)


