Differentiating COPD Exacerbations From Other Conditions
Authors: Sarah Williams, PhD, and Takeesha Roland-Jenkins, MS, MS
As the symptoms of chronic obstructive pulmonary disease (COPD) advance into the moderate-to-severe range, the natural course of the disease becomes increasingly likely to be punctuated by acute episodes of increased respiratory symptoms known as exacerbations. Exacerbations have been shown to significantly contribute to the high morbidity and mortality rates among people diagnosed as having COPD.1
COPD is the third-leading cause of death in the United States and is responsible for more than 135,000 deaths per year.2,3 According to a 2013 self-report survey, an estimated 15.7 million (6.4%) of American adults reported having a diagnosis of COPD,4 which is characterized by airflow limitation due to alveolar and/or airway abnormalities.4,5______________________________________________________________________________________________________________________________________________________
RELATED CONTENT
Is Aspirin of Use in Patients With COPD Exacerbations?
Diagnosing Asthma and COPD Overlap Syndrome
______________________________________________________________________________________________________________________________________________________
The term COPD encompasses chronic bronchitis (bronchial tube inflammation) and emphysema (air sac destruction), although most patients with COPD often have both bronchitis and emphysema. COPD has a variety of etiologies, such as an α₁-antitrypsin deficiency, abnormal lung growth and development, cigarette smoking, or exposure to air pollution.
COPD is often missed or underdiagnosed because early symptoms (cough, phlegm, wheezing, shortness of breath with activity, fatigue) are mild or even nonexistent, fluctuate daily, and are relatively common to many other illnesses. However, the condition can progress and worsen until symptoms are severe enough to interfere with the individual’s functioning.4,6
One cardinal symptom of COPD is recurrent and progressive dyspnea.1 Cough with sputum production is present in only about 30% of patients, while others have wheezing and/or chest tightness.4,5 These symptoms regularly precede the progression of airflow restriction, but misdiagnosis and underdiagnosis continue to be a prominent problem in COPD management,7,8 as does the management of exacerbations during the disease course.
Exacerbations of COPD
Historically, there has been wide variation within the literature regarding the definition of a COPD exacerbation,9 although the recent Global Initiative for Chronic Obstructive Lung Disease (GOLD)5 found consensus, defining COPD exacerbations as an acute worsening of respiratory symptoms beyond typical daily variations, leading to a medication change or additional therapy.5
Exacerbations of COPD typically present as an acute, sustained episode demarcated by a significant change in the patient’s baseline symptoms of cough (frequency and severity), sputum (increase in volume or character changes), or dyspnea (frequency).9 Currently, there are no clinically applicable biomarkers capable of predicting COPD exacerbations;10 however, blood eosinophil counts have shown some promise as an informative marker.11
The annual COPD exacerbation rates have been shown to vary from as low as 0.5 to as high as 3.5 exacerbations per patient.12 Exacerbation frequency tends to increase with disease severity, and the median time of recovery is about 1 week.10
A main risk factor for COPD exacerbations is a history of prior exacerbations, regardless of COPD severity. Less certain risk factors are gastroesophageal reflux disease (GERD)13, 14 and secondary pulmonary hypertension.15, 16 A risk model of 11 variables, which included the number of exacerbations in the preceding year, height, age, forced expiratory volume in 1 second and other comorbid conditions, was capable of significantly predicting 2 or more COPD exacerbations.17 Triggers for exacerbations include respiratory infections (responsible for 70% of COPD exacerbations, predominantly viral and/or bacterial in origin), while the remaining 30% are due to environmental pollutants, pulmonary embolism, or some other unknown cause.5,18-21
Evaluating COPD Exacerbations
COPD exacerbations can be deadly.10 Thus, when a patient has a “flare up” and complains of worsening breathlessness, increased cough and sputum production, extreme fatigue, and perhaps some mental confusion, the clinician must determine whether this is really an exacerbation of the underlying COPD, or the manifestation of some other potentially serious clinical event, such as a bacterial or viral infection, or possibly a vascular condition or cardiac event.
The goal of the clinician should be to confirm the diagnosis of COPD and to identify, if possible, the cause of the exacerbation; assess severity; and evaluate the contribution, if any, of comorbidities.13-16,18-21 The initial evaluation should include a physical and mental status examination, pulse oximetry, historical baseline functioning (arterial blood gas measurements, chest radiographs, spirometry findings) and a (Continued on next page)
detailed time-based report of current and past symptoms, including dyspnea reports at rest and with activity, sputum characteristics (amount, presence of blood or purulence), and ability to participate in activities of daily living.21 Individuals requiring emergency care or those with moderate-to-severe exacerbations may also require chest radiographs, laboratory tests, and arterial blood gas analysis.
Differentiating a COPD exacerbation from other serious clinical events can be challenging. According to James Donohue, MD, who is with the University of North Carolina Department of Medicine in Pulmonary Diseases and Critical Care Medicine, “Patients with COPD have multiple comorbidities, and this symptom complex can be seen in congestive heart failure, pulmonary edema, acute pulmonary embolus, pneumonia, pneumothorax, cardiovascular illness such as myocardial infarction, aortic dissection, and pericardial effusion.” Dr. Donohue advises that a careful history and physical examination, chest radiograph, evaluation of sputum, complete blood count with differential, and electrocardiogram are necessary. He also suggests considering obtaining a computed tomography angiogram of the lungs for pulmonary embolus, if indicated.
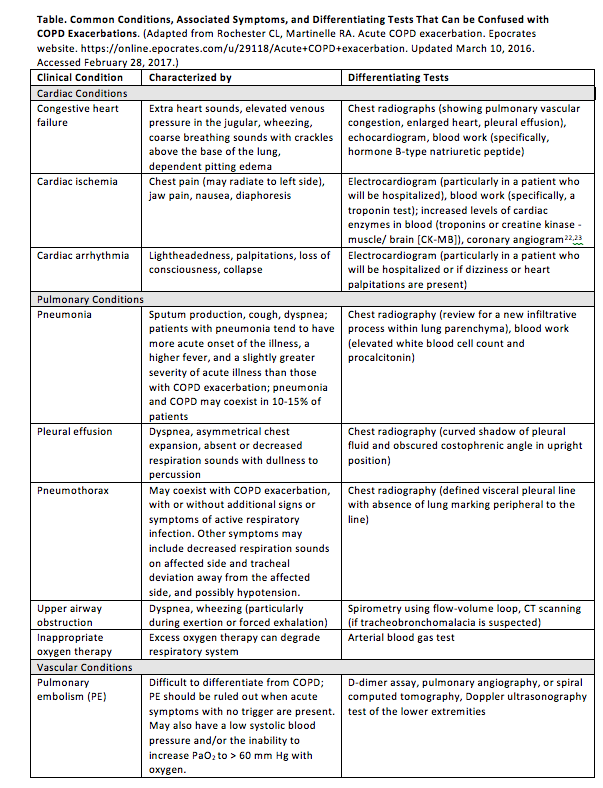
See Table for methods to differentially diagnose COPD exacerbations by body system from other common and potentially serious clinical conditions.
Conclusion
Patients with COPD, and particularly those with exacerbations, may present with complex comorbidities. If patients are experiencing an acute increase in symptoms beyond the normal daily variations associated with their COPD, and this leads to a change in medications, they may be having an exacerbation. After the severity and cause of the exacerbation are identified, the clinician should proceed with a differential diagnosis and determine whether comorbidities are a contributing or a predominant factor. Long-term management of COPD exacerbations should focus on managing risk factors like smoking cessation and pulmonary rehabilitation, as well as encouraging compliance with medications and enforcing vaccinations against respiratory infections.
Sarah Williams, PhD, and Takeesha Roland Jenkins, MS, MS, are medical writers at HE Institute, located in Ponte Vedra Beach, Florida.
1. Evensen AE. Management of COPD Exacerbations. Am Fam Physician. 2010;81(5):607-613.
2. Saraiva C, Abreu T, Neves D, Rodrigues F. Mortality predictive factors in subjects with COPD after a pulmonary rehabilitation program: a 3-year study. Respir Care. 2016;61(9):1179-1185.
3. National Heart, Lung, and Blood Institute. What is COPD? http://www.nhlbi.nih.gov/health/educational/copd/what-is-copd/index.htmhttp://www.nhlbi.nih.gov/health/educational/copd/what-is-copd/index.htm. Accessed February 24, 2017.
4. Wheaton AG, Cunningham TJ, Ford ES, Janet B. Croft JB.. Employment and activity limitations among adults with chronic obstructive pulmonary disease – United States, 2013. MMWR. 2015;64(11):290-295.
5. GOLD 2017 Global Strategy for the Diagnosis, Management and Prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease website. http://goldcopd.org/gold-2017-global-strategy-diagnosis-management-prevention-copd. Accessed February 17, 2017.
6. Vos T, Flaxman AD, Naghavi M et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163-2196.
7. Guarascio AJ, Ray SM, Finch CK, Self TH. The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinicoecon Outcomes Res. 2013;5:235-245.
8. Soriano JB, Zielinski J, Price D. Screening for and early detection of chronic obstructive pulmonary disease. Lancet. 2009;374(9691):721-732.
9. Ali NK. Evidence-based approach to acute exacerbations of chronic obstructive pulmonary disease. Hosp Phys. 2009;38:9-16.
10. Donaldson GC, Wedzicha JA. COPD exacerbations – 1: Epidemiology. Thorax. 2006;61(2):164-168.
11. Pavord ID, Lettis S, Locantore N, Pascoe S, Jones PW, Wedzicha JA, Barnes NC. Blood eosinophils and inhaled corticosteroid/long-acting β-2 agonist efficacy in COPD. Thorax. 2016;71(2):118-125.
12. Seemungal TA, Hurst JR, Wedzicha JA. Exacerbation rate, health status and mortality in COPD–a review of potential interventions. Int J Chron Obstruct Pulmon Dis. 2009;4(1):203-223.
13. Kim J, Lee JH, Kim Y, et al. Association between chronic obstructive pulmonary disease and gastroesophageal reflux disease: a national cross-sectional cohort study. BMC Pulm Med. 2013;13:51.
14. Hurst JR, Vestbo J, Anzueto A, et al. Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Investigators. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128-1138.
15. Wells JM, Washko GR, Han MK, et al. Pulmonary arterial enlargement and acute exacerbations of COPD. N Engl J Med. 2012;367(10):913-921.
16. Shujaat A, Bajwa AA, Cury JD. Pulmonary Hypertension Secondary to COPD. Pulm Med. 2012;2012:203952.
17. Kerkhof M, Freeman D, Jones R, Chisholm A, Price DB. Predicting frequent COPD exacerbations using primary care data. International journal of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;10:2439-2450.
18. Barnes PJ. Chronic obstructive pulmonary disease. N Engl J Med. 2000;343(4):269-280.
19. Sapey E, Stockley RA. COPD exacerbations. 2: aetiology. Thorax. 2006;61(3):250-258.
20. Gan WQ, FitzGerald JM, Carlsten C, Sadatsafavi M, Brauer M. Associations of ambient air pollution with chronic obstructive pulmonary disease hospitalization and mortality. Am J Respir Crit Care Med. 2013;187(7):721-727.
21. Rochester CL, Martinelle RA. Acute COPD exacerbation. Epocrates website. 2016; https://online.epocrates.com/u/29118/Acute+COPD+exacerbation. Updated March 10, 2016. Accessed February 28, 2017.
22. Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014. 130(25):e344-e426.
23. Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016. 37(3):267-315.


