Office Management of Acute Ankle Injuries: Part 1
ABSTRACT: Roughly 85% of all acute ankle injuries are sprains; most are uncomplicated and involve the lateral ligaments only. However, there are 5 fractures that must be considered in the evaluation of acute ankle injuries. Of the 5 fractures, 2 occur to the proximal portion of the fifth metatarsal and 2 occur to the distal third of the fibula. These are easily detectable by palpation before the onset of soft tissue swelling. Even after the onset of significant soft tissue swelling and generalized discomfort, discrete tenderness can usually be elicited at the fracture site. The fifth fracture occurs to the dome of the talus, which is located inside the ankle joint and is not accessible to detection by palpation.
All acute ankle injuries result in soft tissue trauma and swelling. Associated with these findings is loss of motion, which presents as stiffness, increased generalized discomfort, and an increased level of disability. The time frame between an acute ankle injury and the initial evaluation is usually sufficient for significant soft tissue swelling and the physical and functional changes to occur. This increased level of disability noted initially can lead to the assumption that the severity of the injury is greater than it is. Thus, during the history taking, it is important to obtain the level of disability at the time of the injury and shortly after. In this article, we focus on the evaluation and management of the 5 fractures that must be considered in the assessment of acute ankle injuries. We also provide a systematic guide for the examination of these injuries . In a coming issue, we will focus on the 3 significant soft tissue injuries that must be considered in the evaluation.
ACUTE ANKLE INJURIES
Roughly 85% of all acute ankle injuries are sprains,1 of which about 85% are uncomplicated, ie, involving the lateral ligaments only.2 When the examination findings are incompatible with a fracture or tendon injury (Box I), results of diagnostic studies are negative, and the primary area of tenderness is anteroinferior to the lateral malleolu over the anterior talofibular and calcaneofibula rligaments (Figure 1), the diagnosis is that of an uncomplicated lateral ankle sprain.

FRACTURES
The 5 fractures clinicians must consider are typically associated with a soft tissue injury to the ankle, most frequently an inversion injury, with the ankle in plantar flexion. In most instances, the patient can point to the fracture site as the area where he or she had the most severe pain. Each of the 5 potential fracture sites is subjected to different levels of forces during routine activities. An activity that causes minimal discomfort at one fracture site may cause greater discomfort at another fracture site, and this may result in different extents of disability for one fracture site versus another. Routinely with each of these fractures, patients are initially able to place variable amounts of weight on the ankle and often walk on it with a limp; however, with the onset of soft tissue swelling and increased generalized discomfort, their physical limitations increase.
Of the 5 fractures, 2 occur to the proximal portion of the fifth metatarsal (fractures 1 and 2) and 2 occur to the distal third of the fibula (fractures 3 and 4). These are easily detectable by palpation before the onset of soft tissue swelling. Even after the onset of significant soft tissue swelling and generalized discomfort, discrete tenderness can usually be elicited at the fracture site. The last fracture occurs to the dome of the talus (fracture 5), which is located inside the ankle joint and is not accessible to detection by palpation. In addition, because of the curvature of the talar dome, the fracture is often not seen on radiographs unless the fracture site is conveniently located precisely in the area of the talar dome that is included on the film.
1 – Avulsion Fracture of the Base of the Fifth Metatarsal
Mechanism of injury. Inversion of the ankle with the ankle typically in plantar flexion.
Symptoms typically experienced. Symptoms are compatible with those of a routine lateral ankle sprain plus a sharp pain and/or pop at the base of the fifth metatarsal.
Extent of disability. The forces transmitted across the base of the fifth metatarsal with weight bearing are minimal. Patients are typically able to walk on the injured ankle with only slight alterations in their gait as a result of the discomfort experienced.
Examination findings.
Palpation reveals tenderness at the base of the fifth metatarsal.
Radiographic findings.
Radiographs show evidence of an avulsion fragment of the base of the fifth metatarsal (Figure 2).
Management. Prevent and/or eliminate soft tissue swelling with appropriate compression, elevation, and pain-free range of motion.1 Treat the fracture symptomatically. In most cases, a comfortable, yet firm, shoe is adequate. Symptomatic treatment of the fracture is followed by the patient’s participation in a comprehensive lateral ankle sprain treatment program. The discomfort at the fracture site dictates initiation of and progression in the treatment program.1

2 – Fracture of the Proximal Shaft of the Fifth Metatarsal (Jones Fracture)
Mechanism of injury. Most Jones fractures occur through preexisting stress fractures. The fracture may occur spontaneously with any activity that places stress on the foot, such as running, or in association with an acute injury, most commonly with an inversion injury of the ankle. Some patients relate a history of prior episodes of pain in the area from the stress fracture.
Symptoms typically experienced. The patient can experience an acute episode of sharp pain and/or a pop solely at the proximal shaft of the fifth metatarsal with any activity that places stress on the foot. When the fracture occurs with an inversion of the ankle, the patient can have symptoms compatible with a routine lateral ankle sprain (generalized lateral ankle discomfort) plus a sharp pain and/or pop in the proximal portion of the fifth metatarsal. Extent of disability.
The forces transmitted across the proximal shaft of the fifth metatarsal with weight bearing are greater than those transmitted across the base of the fifth metatarsal. Patients with a Jones fracture are characteristically able to place variable amounts of weight on the injured ankle but are forced to significantly alter their gait because of the discomfort at the fracture site.
Examination findings. Palpation reveals discrete tenderness at the proximal shaft of the fifth metatarsal.
Radiographic findings. Radiographs show evidence of a fracture of the proximal shaft of the fifth metatarsal, frequently through a preexisting stress fracture (which is diagnosed by callus at the fracture site) (Figure 3). Absence of the callus at the fracture site would change the diagnosis to an acute Jones fracture.

Management. Management of a Jones fracture continues to be controversial. Adding to the dilemma is the classification of Jones fractures as either “acute” or “chronic” (fracture through an existing stress fracture) based on the patient’s history and radiographic findings.
Patients with an acute Jones fracture have a history of being painfree on the lateral aspect of their foot.before the episode of acute pain, whereas those with a chronic fracture have a history of recurrent pain on the lateral aspect of their foot before the episode of acute pain. Radiographic findings in acute fractures show sharp fracture margins and no intramedullary sclerosis, whereas the findings in chronic fractures show a widened fracture line with evidence of periosteal callus compatible with a preexisting stress fracture, as shown in Figure 3. In our experience, the Jones fracture most frequently seen in athletes is the chronic or stress fracture.
Based on reported rates of nonunion of 50% to 60% with conservative management (use of non–weightbearing cast for 6 to 8 weeks) for chronic fractures, the recommended treatment for chronic fractures is open reduction and internal fixation (ORIF).3 For the acute fracture, conservative management with a non– weight-bearing cast for 6 to 8 weeks results in reported rates of nonunion of 25% to 44%.3
The recommended treatment for acute fractures is somewhat debatable. If the typical nonathlete is somewhat overweight, out of shape, and not actively involved in an exercise activity on a regular basis, this person, solely because of the extra weight and lack of physical conditioning, could have a difficult time in a non–weight-bearing cast for 6 to 8 weeks. The question is not whether conservative management should be used but rather how to select the appropriate candidates for this type of treatment.
We feel that the patient should be presented with the 2 methods of treatment (non–weight-bearing cast for 6 to 8 weeks and ORIF) and the reported success rates of each. In the discussion of conservative management, consider the patient’s occupation, commitments outside of work, weight, physical conditioning, and even weather conditions. In addition, advise patients of the consequences of prolonged immobilization (atrophy, loss of flexibility of leg muscles, decreased range of motion of the ankle) and that the time needed to regain normal size, strength, and flexibility of the muscles and normal range of motion of the ankle could be equal to or longer than the period of immobilization.
| ||
3 – Isolated Vertical Fracture of the Distal Third of the Fibula
Mechanism of injury. Inversion of the ankle with the ankle typically in plantar flexion.
Symptoms typically experienced. Patients have symptoms compatible with a routine lateral ankle sprain plus a sharp pain of the distal third of the fibula.
Extent of disability. Although the forces placed on the leg with weight bearing are directly transmitted to the tibia, the tibia transfers a portion (about one-sixth) of this weight to the fibula through the interosseous membrane. Thus, patients with an isolated vertical fracture of the distal third of the fibula are able to walk or limp on the involved lower extremity but have a varying amount of discomfort at the fracture site. The amount of discomfort is directly related to the amount of weight placed on the involved lower extremity.
Examination findings. Palpation reveals diffuse tenderness of the distal third of the fibula.
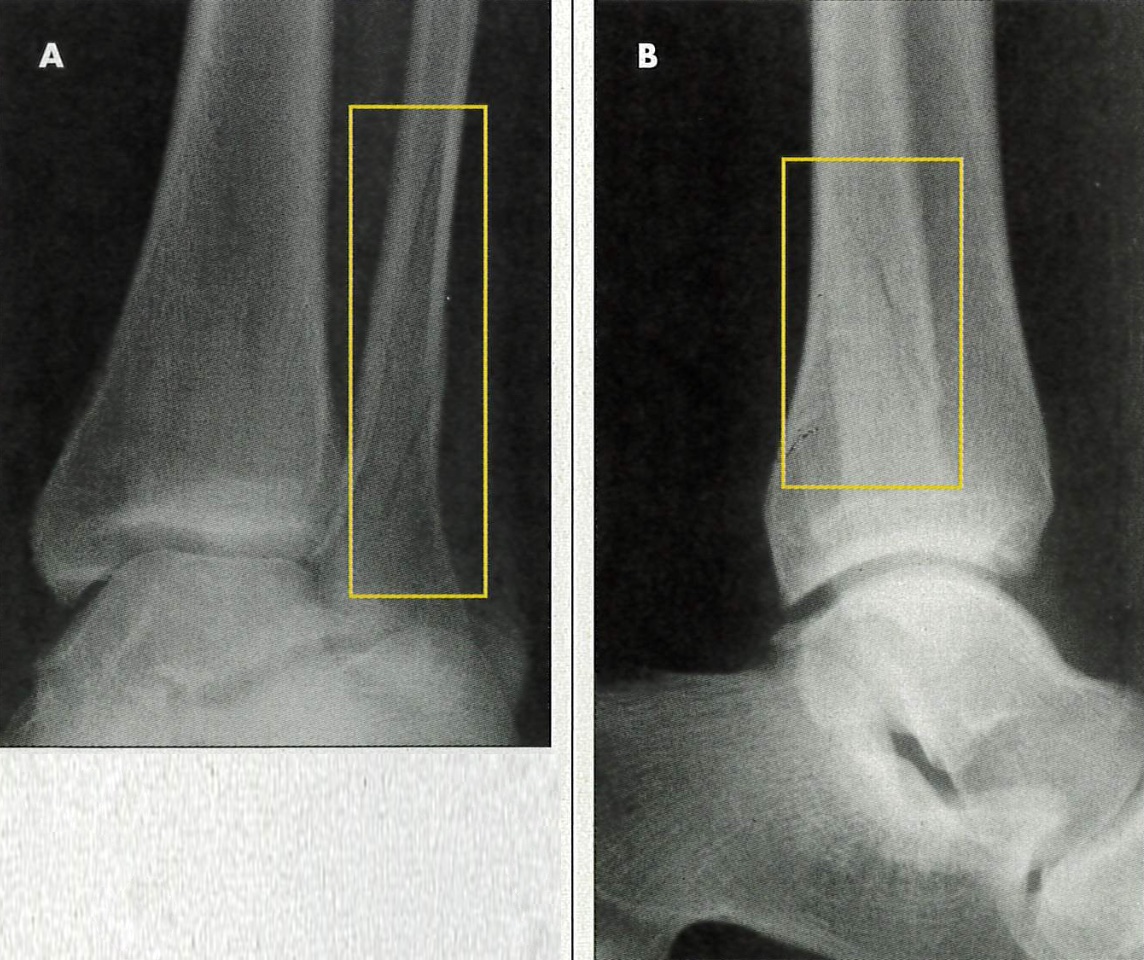
Radiographic findings. Radiographs show evidence of a vertical fracture of the distal third of the fibula; it is not uncommon for the fracture to be evident on the mortise and lateral views only (Figure 4).
Management. Because a fracture of the distal third of the fibula can occur in association with an ankle injury that requires surgical intervention (an injury not isolated to the distal fibula), immobilization and referral to an orthopedic specialist for appropriate management is warranted. An isolated fracture of the distal third of the fibula is generally immobilized for 3 to 6 weeks. Immobilization of an acute ankle injury for even 3 weeks can result in significant atrophy and loss of flexibility of the calf muscles, along with decreased motion of the ankle. Once the fracture has healed, the patient must participate in a comprehensive lateral ankle sprain treatment program to regain normal size, strength, and flexibility of the muscles as well as normal ankle range of motion.1
4 – Epiphyseal Growth Plate Fracture
Mechanism of injury. Inversion of the ankle with the ankle typically in plantar flexion.
Symptoms typically experienced. Patients have symptoms compatible with a routine lateral ankle sprain plus a sharp pain at the growth plate.
Extent of disability. The extent of disability is directly associated with the severity of injury to the growth plate. The patient is characteristically able to walk or limp on the injured ankle with varying amounts of increased pain at the fracture site.
Examination findings. Palpation reveals discrete tenderness of the lateral malleolus at the site of the growth plate, about 1 inch proximal to the distal tip of malleolus.
Radiographic findings. The growth plate will be evident. Typically, no changes are noted on the initial radiographs, although, in some cases, changes compatible with those seen with a Salter-Harris fracture (types I through IV) may be evident.
Management. Some primary care practitioners may feel comfortable managing Salter-Harris type I fractures (fractures limited to distal fibular epiphysis) with immobilization in a short-leg walking cast or CAM walker for 3 to 4 weeks. However, if there is any concern regarding the extent of injury to the growth plate, referral to an orthopedic specialist is warranted. Once the fracture has healed, the patient must participate in a comprehensive lateral ankle sprain treatment program to regain normal size, strength, and flexibility of the muscles as well as normal ankle range of motion.1
5 – Talar Dome Fracture
Mechanism of injury. Characteristically, inversion of the ankle with the ankle in plantar flexion.
Symptoms typically experienced. Patients have symptoms compatible with a routine lateral ankle sprain. Infrequently, patients may state that they felt something happen “inside their ankle.”
Extent of disability. Various areas of the talar dome are tasked with bearing the majority of forces transmitted across the ankle joint with weight-bearing activities. Thus, the extent of disability is directly related to the amount of force normally placed on the fracture site. The patient is generally able to walk or limp on the injured ankle with the amount of discomfort related to the fracture site.
Examination findings. Because the talar dome cannot be directly palpated, the findings are those typically seen with a routine lateral ankle sprain—generalized discomfort of the ankle with increased intensity of the lateral aspect.
Radiographic findings. Fractures of the talar dome primarily occur on either the posterolateral or anteromedial aspect of the talar dome. Often the fracture is not visible on radiographs because of the curvature of the talar dome and because the area of the talar dome where the fracture occurs is usually not included on routine radiographs of the ankle. When the fracture is evident on radiographs, changes are located on either the lateral or medial aspect of the talar dome (Figure 5).

Management. When a fracture is evident on initial radiographs, immobilization and referral to an orthopedic specialist is warranted. Fragments of this fracture can become loose in the joint. Loose bodies in the joint can lead to episodes of sharp pain inside the ankle accompanied by a feeling that something is in the way. Because the fracture is generally not evident on radiographs, a talar dome fracture becomes the working diagnosis when the patient is slow to progress during or after a comprehensive lateral ankle sprain treatment program. For instance, if the patient has persistent pain inside the ankle with or without loose-body sensations during the program or after he returns to functional activities and follow- up radiographs are negative, the working diagnosis is a talar dome fracture and referral to an orthopedic specialist for further evaluation with a bone scan or MRI is warranted.
It is important to be able to distinguish a talar dome fracture from osteochondritis dissecans, in which a portion of the talar dome loses its blood supply (Figure 6). This type of avascular necrosis usually occurs during adolescence. The resulting bony lesion may remain asymptomatic and heal uneventfully with the return of adequate blood supply to the area, or it may present with symptoms compatible with a talar dome fracture (pain inside the ankle with or without loose-body sensations). The symptoms may develop insidiously or with any acute injury to the ankle.
Like talar dome fractures, osteochondral injury of the talus may not be evident on initial radiographs. When the lesion is evident, immobilization and orthopedic referral is appropriate. When the lesion is not evident on initial or followup radiographs, the symptoms and the age of the patient dictate whether an orthopedic referral for further evaluation with bone scan or MRI is warranted.

SIGNIFICANT SOFT TISSUE ANKLE INJURIES
Of all the soft tissue ankle injuries, 3 types are considered significant because of the long-term physical limitations that can result, especially when the injuries are not identified and treated appropriately initially. These injuries involve the following anatomical areas and corresponding soft tissue structures:
•Lateral aspect of the ankle: the retinacular sheath of the peroneal tendons— responsible for retaining the peroneal tendons posterior to the lateral malleoli.
•Posterior aspect of ankle: the Achilles tendon—the tendon of the gastrocnemius and soleus muscles.
•Medial aspect of the ankle: the tendon of the tibialis posterior muscle— which is located posterior to the medial malleoli and runs a course inferior and anterior to the medial malleolus to its insertion onto the navicular bone.
Because of the potential for long-term disability after injury to each of these structures, their examination during the acute ankle injury evaluation must be emphasized. By the time the patient with a significant soft tissue ankle injury is evaluated in the office, the findings on examination are usually not as discrete to the area of injury as they are when the ankle is examined immediately after the injury. However, even if soft tissue swelling prevents a definitive diagnosis by examination alone, a history that reveals the typical mechanism of injury, symptoms experienced, and level of disability at the time of the injury is usually enough to warrant early orthopedic referral.
1 – Peroneal Tendon Dislocation
Mechanism of injury. Dislocation of the peroneal tendons occurs only when the stress placed on the peroneal tendon retinacular sheath is sufficient enough to cause it to either rupture or avulse from the posterolateral aspect of the lateral malleolus. When the ankle is forced into dorsiflexion with or without inversion during an acute ankle injury, the integrity of the retinacular sheath—the ability to retain the peroneal tendons posterior to the malleoli—is challenged. If the stress is sufficient, the peroneal tendons can dislocate anteriorly. When the ankle is taken out of dorsiflexion, the peroneal tendons spontaneously reduce to their normal location posterior to the lateral malleoli.
The mechanism of a typical uncomplicated lateral ankle sprain—inversion with the ankle in plantar flexion—does not cause the peroneal tendons to place stress on their retinacular sheath.
Symptoms typically experienced. Patients commonly say that they felt something quickly slip or pop forward over the bone on their outer ankle and then quickly slip or pop back.
Extent of disability. The disability is typically significant. Patients frequently hobble on the ball of their foot to keep the ankle in plantar flexion (this prevents them from feeling that the peroneal tendons may redislocate). Some patients may be able to walk or limp on the foot but have persistent, often intense, pain at the site of the injured retinacular sheath.
Examination findings. Because the peroneal tendons spontaneously reduce when the foot is out of the forced dorsiflexed position, distinct tenderness is limited to the area posterolateral to the lateral malleoli (where the peroneal tendon retinacular sheath is located). Patients may also have generalized pain of the peroneal tendons. The generalized tenderness of peroneal tendon dislocation differs from that of a typical lateral ankle sprain in that it more closely follows the course of the tendons posterior to the lateral malleoli. With an uncomplicated lateral ankle sprain, there is no pain over the peroneal tendons or sheath.
Radiographic findings. In most cases, radiographs are unremarkable; however, a small avulsion fracture of the posterior lateral malleolus may infrequently occur. This fragment is seen on the anterior views of the ankle only and confirms the diagnosis.
Management. Immobilization and referral to an orthopedic specialist is warranted when the diagnosis is either strongly suspected or confirmed by the history and examination. Definitive treatment (usually operative) by the orthopedic specialist is necessary to regain the integrity of the retinacular sheath. Unless the integrity of the sheath is regained, painful dislocations of the peroneal tendons can recur and severely limit the patient’s activity.
2 – Achilles Tendon Rupture
Mechanism of injury. Achilles tendon rupture may result from an acute episode of ballistic stress that is placed on the tendon during a physical activity, such as basketball, or from sudden, unexpected dorsiflexion of the ankle that occurs with a seemingly benign action, such as stepping off an unseen curb. Although usually considered an injury of the younger athlete, Achilles tendon rupture is common in both athletic and nonathletic persons 35 years and older.
Symptoms typically experienced. Patients usually feel a sharp pain and/or pop in the back of the ankle at the time of the rupture.
Extent of disability. The extent of disability is significant, although the pain following the acute painful rupture may be minimal. The patient can usually walk or limp on the injured ankle but walks flatfooted with the foot externally rotated to eliminate the toe-off phase of the gait, which requires an intact Achilles tendon complex.
Examination findings. Achilles tendon ruptures occur 21⁄2 to 3 inches above the tendon’s insertion into the calcaneus. If there is no soft tissue swelling, a defect in the tendon may be visible and/or palpable in this area. This defect is associated with discrete tenderness. Although the presence of soft tissue swelling may obscure this defect, discrete tenderness will still be noted in this area of the Achilles tendon—21⁄2 to 3 inches above the tendon’s insertion into the calcaneus.
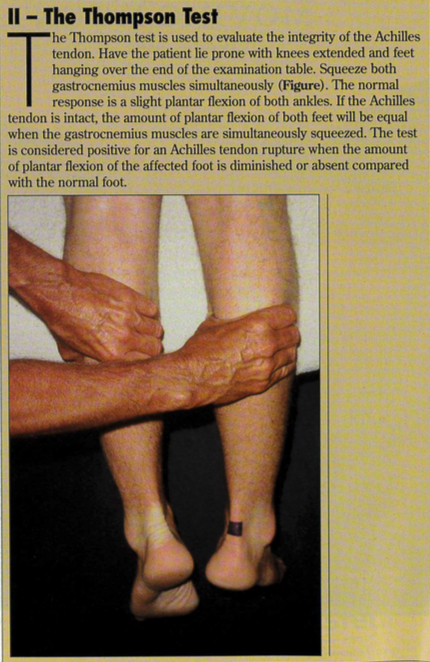
The Thompson test can be used to evaluate the integrity of the Achilles tendon. With the patient lying prone with knees extended and feet hanging over the end of the examination table, the examiner squeezes the gastrocnemius muscles. The normal response is a slight plantar flexion of both ankles. The test is considered positive for an Achilles tendon rupture when the amount of plantar flexion of the affected foot is diminished or absent compared with the normal foot.
Radiographic findings. No radiographic findings are associated with this injury.
Management. Immobilization and an orthopedic referral are warranted when the diagnosis is either strongly suspected or confirmed by the history and examination. For a successful outcome, definitive treatment, typically surgical repair, should be done within 5 to 10 days of the injury.
3 – Tibialis Posterior Tendon Rupture
Mechanism of injury. A rupture of the tibialis posterior tendon is the end result of attritional changes from chronic tendon inflammation. The rupture most commonly occurs with a seemingly benign activity. For unknown reasons, this injury occurs primarily in women 45 years and older.
Symptoms typically experienced. The discomfort the patient feels at the time of the rupture is minimal. In some cases, this discomfort is so minimal that loss of arch support is the patient’s chief complaint.
Extent of disability. The extent of disability is significant. Patients are able to walk or limp on the injured ankle; however, they have an altered gait as a result of the functional loss of the contributions of the tibialis posterior muscle to the sophisticated motions of the ankle with ambulation.
Examination findings. Patients may have discrete tenderness with or without swelling over the area posterior and inferior to the medial malleolus. The tibialis posterior muscle, which is primarily responsible for inversion of the foot, is also an accessory plantar flexor of the foot and is one of the key structures that help maintain the foot arch. When the tibialis posterior tendon ruptures, the patient’s ability to actively invert the plantar flexed foot and hold the foot in inversion against manual resistance is greatly diminished on the affected side. With the patient standing, loss of the longitudinal arch of the involved foot compared with the noninvolved foot is commonly detected.
Radiographic findings. No radiographic findings are associated with this injury.
Management. Immobilization and orthopedic referral are warranted when the diagnosis is either strongly suspected or confirmed by the history and examination. Because of tendon attrition and chronic inflammation, surgical repair of tibialis posterior tendon rupture is usually difficult, and the results of both nonsurgical treatment and surgery are either very poor or poor in most cases. Thus, the ideal management is prevention of recurrence.
Preventive treatment includes rest, anti-inflammatory medication, calf stretching exercises,4 and sometimes immobilization—if all other conservative measures fail to resolve tendon tenderness. If the patient has pes planus, the use of an over-the-counter semi-rigid arch support (orthotic) may be beneficial. Advise patients to refrain from all activities until they have no swelling or discomfort in the area and have achieved adequate flexibility of the calf muscles. Patients should be educated about the attritional changes that occur when the inflammation is not appropriately treated before their return to activities and how these changes compromise the effectiveness of treatment.
Other tibialis posterior tendon injuries. Avulsion fractures of the tendon’s insertion site onto the navicular bone and ruptures of the extreme distal portion of the tendon have both been reported in younger athletes with a previously healthy ankle. Both of these injuries are described as infrequent; however, health care providers should be aware of them.
The mechanism of injury is resisted inversion or forced eversion of the ankle. Patients feel a sharp pain and/or pop in the area of the navicular on the superior midportion of the arch at the time of the injury. The extent of the disability is significant. Patients are forced to hobble or limp dramatically because of the pain.
The examination reveals discrete pain over the area of the navicular and decreased ability to invert the plantar flexed foot and to resist manual eversion of the plantar flexed foot.
Treatment is immobilization and early orthopedic referral for surgical intervention. The surgical outcome is excellent if these injuries are recognized early.
1. Garrick JG, Heinz Schelkun P. Managing ankle sprains: keys to preserving motion and strength. Phys Sportsmed. 1997;25:56-68.
2. Broström L. Sprained ankles, I: anatomic lesions in recent sprains. Acta Chir Scand. 1964;128: 483-495.
3. Mologne TS, Lundeen JM, Clapper MF, O’Brien TJ. Early screw fixation versus casting in the treatment of acute Jones fractures. Am J Sports Med. 2005;33:970-975.
4. Aronen JG, Garrick JG. Sports-induced inflammation in the lower extremities. Hosp Pract (Minneap). 1999;34:51-67.
5. Stiell IG, Greenberg GH, McKnight RD, et al. A study to develop clinical decision rules for the use of radiology in acute ankle injuries. Ann Emerg Med. 1992;21:384-390.
6. Stiell IG, Greenberg GH, McKnight RD, et al. Decision rules for the use of radiology in acute ankle injuries. Refinement and prospective validation. JAMA. 1993;269:1127-1132.


