Peer Reviewed
Liver Enzyme Abnormalities: What to Do for the Patient
Author:
Allen L. Ginsberg, MD
George Washington University
Citation:
Ginsberg AL. Liver enzyme abnormalities: what to do for the patient. Consultant. 2002;42(3):409-416.
Abstract
High alkaline phosphatase levels generally indicate cholestatic or infiltrative disease, whereas elevated aspertate aminotransferase and alanine aminotransferase levels most likely stem from hepatocellular injury. Consider these abnormalities in the context of the clinical setting to arrive at a diagnosis. For example, a predominant alkaline phosphatase elevation in a young, asymptomatic person who is taking no medications suggests an infiltrative disease; in a feverish college student with a sore throat and cervical lyphadenopathy, infectious mononucleosis; and in a middle-aged woman with pruritus and xanthelasma, primary biliary cirrhosis. Predominant transaminase elevation in a day-care provider who suddenly complains of fever, aching, stomach upset, and jaundice suggests hepatitis A; in a young homosexual man with arthritis, nausea, anorexia, and jaundice of recent onset, it is a clue to sexually transmitted hepatitis B.
You routinely order laboratory screening panels, including serum liver enzyme measurements, for nearly every patient who has a complete physical examination or who is seen for any of a host of other complaints. If you find abnormal liver enzyme levels, your familiarity with the common causes and the settings in which they occur may enable you to avoid costly diagnostic studies or biopsy.
In this article, I present brief case histories of patients who have similar liver enzyme abnormalities but quite dissimilar clinical backgrounds. These differences can help guide you in the interpretation of laboratory findings in your own patients.
AN APPROACH TO INTERPRETING LIVER ENZYME ELEVATIONS
I find it helpful to divide patients with liver enzyme deviations into 2 categories, according to the predominant elevation: alkaline phosphatase or the transaminases—aspartate aminotransferase (AST) and alanine aminotransferase (ALT). When alkaline phosphatase elevations are the main feature, patients generally have either cholestatic disease (with bile duct injury or obstruction) or infiltrative disease— neoplastic or granulomatous (eg, sarcoidosis or tuberculosis). When transaminase elevation is the predominant abnormality, the usual cause is hepatocellular injury—typified by viral hepatitis, autoimmune hepatitis, or injury from medications or toxins (eg, halothane, acetaminophen, or poisonous mushrooms).
An alkaline phosphatase elevation can be induced by liver or bone disease. When it arises from the liver, the other liver enzymes, such as AST and ALT, are usually mildly elevated as well; it is unusual for them to be completely normal. Bone disease, however, cannot account for even mild AST or ALT elevation.
γ-Glutamyl transpeptidase (GGT) levels tend to parallel alkaline phosphatase elevations that stem from the liver. Measurement of GGT can be a useful confirmatory test, but it is an inducible enzyme. Its levels rise (in the absence of liver disease) in persons who are accustomed to drinking excessive quantities of alcohol or who take certain medications, such as phenobarbital or phenytoin.1,2 Some patients have a mixed (cholestatic and hepatocellular) injury, but most can be categorized in the above manner.
PREDOMINANT ALKALINE PHOSPHATASE ELEVATION
Let us consider the cases of 8 patients, all of whom have the same abnormal liver enzyme levels: AST, 75 U/L (normal, 5 to 35 U/L); ALT, 90 U/L (normal, 5 to 40 U/L); and alkaline phosphatase, 450 U/L (normal, less than 85 U/L). (These values are considered the norm in my laboratory.) With the exception of one, all patients have total bilirubin levels of 1.3 mg/dL (normal, up to 1.1 mg/dL). This is a typical pattern in which the alkaline phosphatase concentration is the predominant abnormality. The mild or trivial transaminase elevations strongly suggest that the increased alkaline phosphatase level is from liver rather than bone.
Because this liver enzyme pattern is inconsistent with primary hepatocellular injury, such as that typically seen in viral hepatitis, it would be a waste of money to order hepatitis serologic tests. Nevertheless, you must consider a differential diagnosis that includes a wide range of cholestatic and infiltrative disorders (Table).

Case 1: Young, Asymptomatic Woman
Not every patient, of course, requires extensive evaluation with invasive radiologic studies or liver biopsy. Consider first the clinical setting in which the abnormalities occur. Information garnered from the history and physical examination will enable you to focus on the likely diagnosis, and only one or two confirmatory tests may be required.
During the course of a routine physical examination, a 30-year-old African American woman is found to have the following liver enzyme levels: AST, 75 U/L; ALT, 90 U/L; alkaline phosphatase, 450 U/L. Her serum bilirubin level is 1.3 mg/dL. She is asymptomatic and is taking no medications.
An infiltrative disorder, such as sarcoidosis, rarely causes symptoms, yet it often produces this enzyme pattern. In this setting, obtain a chest film. The finding of bilateral hilar adenopathy might suffice to diagnose sarcoidosis (which occurs 10 times more frequently in black persons). Some physicians might also look for an elevation in serum angiotensin-converting enzyme. If still in doubt, they might perform a liver biopsy; in the case of sarcoidosis, this would almost certainly show noncaseating granulomas (Figure).
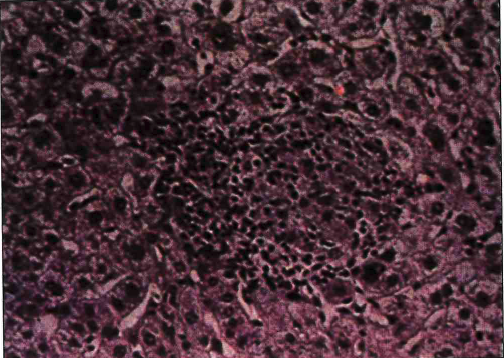
Figure. This photomicrograph shows noncaseating hepatic granulomas in a patient with sarcoidosis.
If the chest film shows no abnormalities, consider the possibility of the earliest stage of primary biliary cirrhosis— a rare disorder found more often in middle-aged women (see Case 5). Abnormal liver enzyme concentrations (predominantly an increase in alkaline phosphatase) in a young woman who is asymptomatic is now a common presentation for primary binary cirrhosis. A positive test for antimitochondrial antibodies would strongly support this diagnosis.
Case 2: Ill, Feverish College Student
A 20-year-old college student is feverish and has a sore throat and cervical lymphadenopathy. Serum levels include AST, 75 U/L; ALT, 90 U/L; alkaline phosphatase, 450 U/L; and bilirubin, 1.3 mg/dL.
In this setting, the diagnosis is almost certainly mononucleosis or a re- lated viral disease, such as cytomegalovirus (CMV) infection. You may find that her spleen is palpable, and you should expect to see atypical lymphocytes on a peripheral smear. A spot test for mononucleosis or an Epstein-Barr virus titer should be diagnostic.
Mononucleosis commonly produces this liver enzyme pattern. The characteristic predominant alkaline phosphatase elevation is presumed to be caused by sinusoidal infiltration with atypical lymphocytes.3 No additional studies should be necessary.
Case 3: Woman With Acute Abdominal Pain
A 40-year-old woman seen in the emergency department has had severe right upper quadrant pain for the past 3 hours. Her blood studies reveal AST, 75 U/L; ALT, 90 U/L; alkaline phosphatase, 450 U/L; and bilirubin, 1.3 mg/dL.
Numbers 1, 2, and 3 on your differential diagnosis should be cholelithiasis, which should be confirmed with an ultrasonogram. If no gallstones are visualized (small stones may be missed on the ultrasonogram or CT scan), but this patient continues to have similar attacks, cholecystectomy— with operative cholangiogram or preoperative endoscopic retrograde cholangiopancreatography (ERCP)— will still be necessary.
Case 4: HIV-positivity, Low-grade Fever, Weight Loss
A 30-year-old man who is HIVpositive has had a low-grade fever and weight loss for several weeks. His liver enzyme studies are as follows: AST, 75 U/L; ALT, 90 U/L; alkaline phosphatase, 450 U/L. His serum bilirubin level is 1.3 mg/dL.
Until it is proved otherwise, abnormal liver enzyme levels in an HIVpositive patient are consicaused by an opportunistic infection (eg, tuberculosis, candidiasis, CMV infection), which may involve the liver. A drug reaction must also be considered.
Moreover, HIV-positive patients are susceptible to bile duct infection caused by Microsporidia, Cryptosporidium, or CMV.4,5 Obtain a CT scan to search for focal lesions in the liver and bile duct dilation. A liver biopsy may be necessary to identify the pathogen.
Case 5: Middle-aged Woman With Pruritus and Xanthelasma
A 40-year-old woman complains of pruritus, and you note that she has xanthelasma. Her serum values include AST, 75 U/L; ALT, 90 U/L; alkaline phosphatase, 450 U/L; and bilirubin, 1.3 mg/dL.
This is the classic presentation of primary biliary cirrhosis. As previously mentioned, this almost always affects middle-aged women. You would expect this patient to test strongly positive for antimitochondrial antibody. If this antibody is absent, have her bile ducts evaluated by means of ERCP or percutaneous transhepatic cholangiography. Patients with primary biliary cirrhosis benefit from therapy with ursodeoxycholic acid.6
Case 6: Enlarged, Nodular Liver and Anemia in Older Man
A 60-year-old man complains of decreased energy. His liver is large, hard, and nodular. His hematocrit is 29%; mean corpuscular volume, 60 fL; stool test, positive for occult blood. The patient’s liver enzyme levels are AST, 75 U/L; ALT, 90 U/L; alkaline phosphatase, 450 U/L. His serum bilirubin level is 1.3 mg/dL.
These findings immediately suggest colon cancer with metastasis to the liver. Cancer in the cecum and right side of the colon commonly presents with occult blood in the stools and iron deficiency anemia. This patient’s liver enzyme pattern is typical of metastatic infiltration of the hepatic parenchyma. The diagnosis can be confirmed with colonoscopy.
Case 7: Young Man With Ulcerative Colitis
A 30-year-old man with ulcerative colitis in remission is receiving sulfasalazine( maintenance therapy. His serum values include AST, 75 U/L; ALT, 90 U/L; alkaline phosphatase, 450 U/L; and bilirubin, 1.3 mg/dL.
This is a textbook case of sclerosing cholangitis. Although it is seen in association with ulcerative colitis, this condition does not correlate with the activity or extent of colitis. The diagnosis can be confirmed with ERCP.
Case 8: Elderly Woman With Jaundice
Painless jaundice develops in a 70-year-old woman. She had a sinus infection a month earlier, for which she was given amoxicillin-clavulanate. Her liver enzyme values are AST, 75 U/L; ALT, 90 U/L; and alkaline phosphatase, 450 U/L. Her serum bilirubin level is 6 mg/dL.
When you find clinical and laboratory evidence of cholestasis in an elderly patient, you must consider malignancy as well as drug-induced cholestasis. Painless jaundice associated with this liver enzyme profile constitutes a classic presentation of cancer of the head of the pancreas.
Remember, however, that medications (typically phenothiazines) may also produce this clinical and laboratory picture. Amoxicillin-clavulanate occasionally causes intrahepatic cholestasis, which may appear even after the drug is discontinued.7 Obtain an ultrasonogram or CT scan of the liver and pancreas to exclude tumor in the head of the pancreas and/or bile duct dila- tion. If there is any doubt, ERCP may be necessary.
PREDOMINANT TRANSAMINASE ELEVATION
AST and ALT elevations can be marked or mild. Very high levels usually indicate acute hepatocellular necrosis, as seen in viral- or drug-induced hepatic injury. Extremely high levels (5000 to 10,000 U/L or higher) suggest an overdose of acetaminophen.8 As you will see in the following 4 cases, the laboratory data and the clinical history often point to the correct diagnosis.
Case 9: Sudden Illness in Day-care Teacher
A 30-year old teacher in a day-care center abruptly becomes feverish, with a temperature of 38.9ºC (102ºF); she suffers headache and myalgias, followed by nausea and anorexia. The fever subsides after 48 hours and she feels better, but then she notices that her urine is dark and her scleras are yellow. Her liver enzyme levels are AST, 1200 U/L; ALT, 1500 U/L; and alkaline phosphatase, 150 U/L. Her serum bilirubin concentration is 5 mg/dL.
This is a truly representative case of hepatitis A, epidemics of which have been reported in day-care centers. In contrast to other forms of viral hepatitis, hepatitis A typically presents with the sudden onset of a flu-like illness featuring headache, fever, and myalgias. The appropriate confirmatory test is IgM antibody to hepatitis A, an acute phase reactant. Other hepatitis serologic tests would be superfluous.
Case 10: Arthritis, Nausea, and Anorexia in Homosexual Man
A 30-year-old man describes the recent occurrence of arthritis in his fingers and knees and a rash on his legs. Over the following 2 weeks, he experiences an insidious onset of nausea and anorexia. The patient then notes that his urine is dark and the whites of his eyes are yellow. His serum values include AST, 1200 U/L; ALT, 1500 U/L; alkaline phosphatase, 150 U/L; and bilirubin, 5 mg/dL.
Here we see a typical case of hepatitis B, which may be sexually transmitted and is frequently encountered among male homosexuals. Extraintestinal manifestations, such as arthritis and vasculitis, are common in the late incubation period. The diagnosis is confirmed by detection of the hepatitis B surface antigen.
Case 11: Arthralgias and Amenorrhea in Young Woman
A 30-year-old woman complains of arthralgias and amenorrhea. Her liver enzyme pattern includes AST, 200 U/L; ALT, 200 U/L; and alkaline phosphatase, 120 U/L. Her serum bilirubin concentration is 1.2 mg/dL.
The cause of such moderate transaminase evaluation should be identified if possible, whether or not the patient has symptoms. The abnormality is usually chronic. Document these abnormal transaminase levels if they persist for more than 3 months.
In this patient, the diagnosis is autoimmune chronic hepatitis, which generally occurs in young women and commonly presents with arthralgias and/or amenorrhea. Hyperglobulinemia is common, and hypersplenism may be present. Tests for fluorescent antinuclear antibodies and smooth muscle antibodies are likely to be positive. Corticosteroid therapy, often combined with azathioprine(, may be lifesaving.9 The differential diagnosis includes chronic hepatitis C, drug-induced liver injury, and such hereditary metabolic disorders as Wilson disease, hemochromatosis, and α1-antitrypsin deficiency.
Case 12: Alcohol-induced Liver Injury
A 35-year-old bartender undergoes routine blood studies. Values include AST, 150 U/L; ALT, 60 U/L; alkaline phosphatase, 85 U/L; and GGT, 300 U/L (normal, 5 to 40 U/L).
Although the patient denies drinking heavily, alcohol-induced liver injury is the obvious diagnosis. In most patients thus affected, the ALT value is normal or only minimally elevated. The AST level is usually more than twice that of the ALT, but it is below 300 U/L in over 95% of cases.10,11 The GGT elevation is induced by alcohol and is invariably marked. These liver enzyme values suffice for the diagnosis; it is unnecessary to order a liver biopsy or any other tests.
REFERENCES
- Whitfield JB, Moss DW, Neale G, et al. Changes in plasma γ-glutamyl transpeptidase activity associated with alterations in drug metabolism in man. Br Med J. 1973;1:316-318.
- Davidson DC, McIntosh WB, Ford JA. Assessment of plasma γ-glutamyl transpeptidase activity and urinary D-glucaric acid excretion as indices of enzyme induction. Clin Sci Mol Med. 1974;47:279-283.
- Shuster F, Ognibene AI. Dissociation of serum bilirubin and alkaline phosphate in infectious mononucleosis. JAMA. 1969;209:267-268.
- Cello JP. Acquired immunodeficiency syndrome cholangiopathy: spectrum of disease. Am J Med. 1989;86:539-546.
- Beaugerie L, Teilhoc MF, Deluol AM, et al. Cholangiopathy associated with Microsporidia infection of the common bile duct mucosa in the patient with HIV infection. Ann Intern Med. 1992;117:401-402.
- Poupon RE, Poupon R, Balkau B, et al. Ursodiol for the long-term treatment of primary biliary cirrhosis. N Engl J Med. 1994;330:342-347.
- Reddy KR, Brilliant P, Schiff EF, et al. Amoxicillin/clauvulnic acid potassium-associated cholestasis. Gastroenterology. 1989;96:1135-1141.
- Zimmerman HJ. Hepatotoxicity. New York: Appleton-Century-Crofts; 1978:288.
- Johnson PJ, McFarlane IG, Williams R. Azathioprine for long-term maintenance of remission in autoimmune hepatitis. N Engl J Med. 1995;333:958-963.
- Bradus S, Korn RJ, Chomet B, Zimmerman HJ. Hepatic function and serum enzyme levels in association with fatty metamorphosis in the liver. Am J Med Sci. 1963;246:69-75.
- Zimmerman HJ, Seef LB. Enzymes in hepatic disease. In: Coodley EL, ed. Diagnostic Enzymology. Philadelphia: Lea & Febiger; 1970:1-38.
1. Whitfield JB, Moss DW, Neale G, et al. Changes in plasma y-glutamyl transpeptidase activity associated with alterations in drug metabolism in man. Br Med J. 1973;1:316-318.
2. Davidson DC, McIntosh WB, Ford JA. Assessment of plasma y-glutamyl transpeptidase activity and urinary D-glucaric acid excretion as indices of enzyme induction. Clin Sci Mol Med. 1974;47: 279-283.
3. Shuster F, Ognibene AI. Dissociation of serum bilirubin and alkaline phosphatase in infectious mononucleosis. JAMA. 1969;209:267-268.
4. Cello JP. Acquired immunodeficiency syndrome cholangiopathy: spectrum of disease. Am J Med. 1989;86:539-546.
5. Beaugerie L, Teilhoc MF, Deluol AM, et al. Cholangiopathy associated with Microsporidia infection of the common bile duct mucosa in the patient with HIV infection. Ann Intern Med. 1992;117:401-402.
6. Poupon RE, Poupon R, Balkau B, et al. Ursodiol for the long-term treatment of primary biliary cirrhosis. N Engl J Med. 1994;330:342-347.
7. Reddy KR, Brilliant P, Schiff EF, et al. Amoxicillin/ clavulanic acid potassium-associated cholestasis. Gastroenterology. 1989;96:1135-1141.
8. Zimmerman HJ. Hepatotoxicity. New York: Appleton- Century-Crofts; 1978:288.
9. Johnson PJ, McFarlane IG, Williams R. Azathioprine for long-term maintenance of remission in autoimmune hepatitis. N Engl J Med. 1995;333:958-963.
10. Bradus S, Korn RJ, Chomet B, Zimmerman HJ. Hepatic function and serum enzyme levels in association with fatty metamorphosis of the liver. Am J Med Sci. 1963;246:69-75.
11. Zimmerman HJ, Seeff LB. Enzymes in hepatic disease. In: Coodley EL, ed. Diagnostic Enzymology. Philadelphia: Lea & Febiger; 1970:1-38.


