Intravenous Drug User With Hand and Forearm Pain
What’s Your Diagnosis?
Sharpen Your Diagnostic Skills
 HISTORY
HISTORY
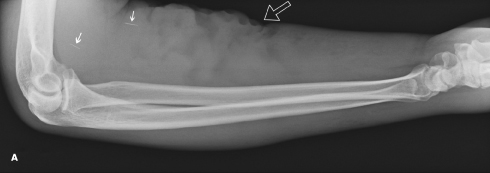
A 50-year-old man, who is right hand dominant, presents to the emergency department (ED) with swelling of the left hand and intense pain. He is an intravenous drug user with multiple prior admissions because of abscess formation in both upper extremities. A radiograph of the right forearm from a previous visit (A) shows retained needle fragments (arrows). The irregularity of the volar skin margin (open arrow) is attributable to scarring and disfigurement from a long history of intravenous drug injection. As a result of ongoing intravenous drug abuse, he has obliterated most of the veins of both upper extremities and has started injecting directly into muscles.
Two days before he presented to the ED, he injected into the dorsum of his left hand. A few hours later, the hand became swollen and very painful, and the symptoms progressively worsened. He denies fever, chills, nausea, vomiting, and lightheadedness.
PHYSICAL EXAMINATION
The patient is alert and oriented to person, time, and place. Blood pressure is 138/69 mm Hg; heart rate, 77 beats per minute; respiration rate, 18 breaths per minute; oxygen saturation, 98% on room air; and oral temperature, 35.3°C (95.5°F).
There is marked disfigurement of both upper extremities. The left hand is diffusely swollen, with associated erythema extending from the metacarpophalangeal (MCP) joints to 5 cm proximal to the wrist along the dorsum. This area is tender to palpation. Pain is also elicited with active and passive flexion and extension of the wrist, MCP joints, and proximal interphalangeal joints. There are no areas of focal fluid collection or fluctuance. Strength is 5/5 and symmetric in both hands and forearms. Sensation to light touch is preserved throughout all nerve distributions. No palpable lymphadenopathy in the left upper extremity or axilla is present. Results of the pulmonary and cardiac examinations are unremarkable.
IMAGING STUDIES
As part of the work-up, a radiograph of the left hand (B) is obtained. It shows marked soft tissue swelling, especially along the dorsum of the hand (arrow). A sonographic examination of the left forearm extensor compartment is also performed (C, D, and E).

WHAT’S YOUR DIAGNOSIS?
WHAT’S YOUR DIAGNOSIS?
ANSWER: CELLULITIS OF THE DORSAL HAND, WRIST, AND FOREARM, COMPLICATED BY ACUTE SUPPURATIVE TENOSYNOVITIS OF THE FOREARM EXTENSOR COMPARTMENT
 IMAGING RESULTS
IMAGING RESULTS
Sonography has become an important tool in musculoskeletal imaging.1,2 The spatial resolution of high-frequency ultrasound transducers exceeds that of MRI under certain conditions.3 When there is a specific clinical question, a focused sonographic examination can perform as well as MRI.4,5 Ultrasonography is easily accessible and is less expensive than MRI, does not involve ionizing radiation, and can be dynamic. Moreover, unlike MRI and CT, ultrasonography has virtually no contraindications, such as claustrophobia (MRI), contrast allergies (MRI and CT), compromised renal function (MRI and CT), and pregnancy (CT). However, its utility is limited by operator dependence and the radiologist’s experience in musculoskeletal ultrasonography.
In this case, the sonographic images were obtained using a Philips HDI 5000 with a 12-5 Hz linear transducer starting from the dorsal wrist toward the mid forearm. The images (Figures 1A, 2A, and 3A) show the fibrillary echotexture of the tendons (arrow heads), which appear bright.6 These tendons are thickened and surrounded by hypoechoic (dark) oval areas that represent fluid collections (small arrows), which may be edema and/or pus, within the tendon sheaths. Thickening of the tendons and surrounding edema and pus are common findings of tenosynovitis.7,8 Doppler imaging (Figures 1B, 2B, and 3B) shows increased color flow, consistent with hyperper-fusion, which has been shown to be associated with inflammatory changes.9 In addition, skin thickening is present (curved arrows); this is a sonographic indicator of cellulitis.

TENOSYNOVITIS: A BRIEF OVERVIEW
Tenosynovitis is a nonspecific inflammatory condition that affects the synovial lining of the tendon sheath and in many cases the tendon itself. The classic presentation is pain and swelling along the affected tendon. This is mirrored on physical examination by localized swelling, pain on palpation, and pain with active and passive range of motion of the affected tendons. In the wrist, tenosynovitis is more common in the extensor compartment.10 It can occur as a result of inflammatory arthritis, crystalline tendinopathy (calcific tenosynovitis or gout), deposition diseases (amyloidosis), and infectious tenosynovitis.11 Also, posttraumatic tenosynovitis may occur from a single traumatic event or from an overuse syndrome.12
Infectious tenosynovitis can be further categorized as pyogenic or nonpyogenic. In this case, the patient had cellulitis of the left hand complicated by pyogenic tenosynovitis. Pyogenic or acute suppurative tenosynovitis is often caused by a penetrating
injury, but may be hematogenous in origin.13 If the clinical diagnosis is uncertain, aspiration of tendon sheath fluid can be performed under sterile conditions with sonographic guidance. If a focal fluid collection suggestive of an abscess is detected at sonography, it must be drained surgically.13 The most common infecting organism is Staphylococcus aureus.13 Other infectious complications can coexist with pyogenic tenosynovitis, such cellulitis (as in this case), abscess formation, and tendon injury or rupture. Treatment of acute pyogenic tenosynovitis should be promptly initiated to avoid propagation of infection, spread of infection to the deep fascial spaces, and/or functional disability. Treatment consists of immediate antibiotic administration. If there is no clinical improvement within 12 to 24 hours, surgical evaluation and irrigation should be considered.14
If the clinical diagnosis is uncertain, aspiration of tendon sheath fluid can be performed under sterile conditions with sonographic guidance. If a focal fluid collection suggestive of an abscess is detected at sonography, it must be drained surgically.13 The most common infecting organism is Staphylococcus aureus.13 Other infectious complications can coexist with pyogenic tenosynovitis, such cellulitis (as in this case), abscess formation, and tendon injury or rupture. Treatment of acute pyogenic tenosynovitis should be promptly initiated to avoid propagation of infection, spread of infection to the deep fascial spaces, and/or functional disability. Treatment consists of immediate antibiotic administration. If there is no clinical improvement within 12 to 24 hours, surgical evaluation and irrigation should be considered.14
OUTCOME OF THIS CASE
This patient received a diagnosis of cellulitis of the wrist and hand, complicated by pyogenic tenosynovitis of the wrist extensor compartments. The plastic surgeon who evaluated him in the ED determined that he would not benefit from surgical management or aspiration. Intravenous vancomycin was started in the ED. Cultures from the draining arm abscess grew methicillin-sensitive S aureus (MSSA), resistant only to penicillin. Results of a complete blood cell count and basic metabolic panel were within reference range.
After the patient was admitted, infectious disease and general surgery consultants evaluated him. Once they had obtained the results of the sonographic study of the wrist, the consultants opted for continuing medical management. The patient’s symptoms started to improve on the second day of admission and resolved by the fifth day. He was discharged home on a regimen of oral dicloxacillin and was advised to follow up in 5 days in the urgent care clinic. Unfortunately, the patient was lost to follow-up. ■
References:
1. Jacobson JA. Musculoskeletal sonography and MR imaging. A role for both imaging methods. Radiol Clin North Am. 1999;37:713-735.
3. Erickson SJ. High-resolution imaging of the musculoskeletal system. Radiology. 1997;205:593-618.
4. Jacobson JA. Ultrasound in sports medicine. Radiol Clin North Am. 2002;40:363-386.
5. Sofka CM. Ultrasound in sports medicine. Semin Musculoskeletal Radiol. 2004;8:17-27.
6. Martinoli C, Derchi LE, Pastorino C, Bertolotti M, Silvestri E. Analysis of echotexture of tendons with ultrasound. Radiology. 1993;186:839-843.
7. Jeffrey RB Jr, Laing FC, Schechter WP, Markison RE, Barton RM. Acute suppurative tenosynovitis of the hand: diagnosis with US. Radiology. 1987;162:741-742.
8. Evans KD, Farooki S. Sonographic evaluation of extensor tenosynovitis. J Diagnostic Medical Sonography. 2001;17:275-279.
9. Newman JS, Adler RS, Bude RO, Rubin JM. Detection of soft-tissue hyperemia: value of power Doppler sonography. AJR Am J Roentgenol.1994;163:385-389.
10. Evans KD, Farooki S: Sonographic evaluation of extensor tenosynovitis. J Diagnostic Medical Sonography. 2001;17:275-279.
11. Teefey SA, Middleton WD, Boyer MI. Sonography of the hand and wrist. In: Seminars in Ultrasound, CT, and MRI. St. Louis, MO: WB Saunders; 2000;21(3):192-204.
12. Curtis D. Radiography of soft tissue in trauma to the hand and wrist. In: Gilula L, Yin Y, eds. Imaging of the Wrist and Hand. Philadelphia, PA: WB Saunders; 1996:159-167.
13. Neviaser RJ: Acute infections. In: Green DP, ed. Green’s Operative Hand Surgery. 4th ed. Philadelphia, PA: Churchill Livingstone; 1999:1033-1047.
14. Clark DC. Common acute hand infections. Am Fam Phys. 2003;68:2167-2176.


