Peer Reviewed
Allergic Fungal Sinusitis
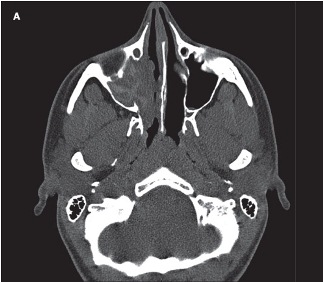 An 18-year-old woman with a history of allergic rhinitis and moderate persistent asthma presented with right-sided nasal congestion of 6 months’ duration. Her symptoms persisted despite her usual allergy medications, allergen immunotherapy, and 2 courses of antibiotics. A sinus CT scan showed complete opacification of the right maxillary sinus with increased attenuation of the mucin (A). Allergic fungal rhinosinusitis was suspected, and an otolaryngologist was contacted.
An 18-year-old woman with a history of allergic rhinitis and moderate persistent asthma presented with right-sided nasal congestion of 6 months’ duration. Her symptoms persisted despite her usual allergy medications, allergen immunotherapy, and 2 courses of antibiotics. A sinus CT scan showed complete opacification of the right maxillary sinus with increased attenuation of the mucin (A). Allergic fungal rhinosinusitis was suspected, and an otolaryngologist was contacted.
The patient underwent functional endoscopic sinus surgery (FESS), which was significant for thick mucin and nasal polyposis. Bacterial cultures of the mucin were negative; however, fungal cultures grew Curvularia (B).
Allergic fungal rhinosinusitis, first described in 1981, is the most common form of noninvasive fungal sinusitis. It should be considered in any atopic patient who presents with chronic sinusitis refractory to usual antibiotic therapy. The condition can occur at any age—although the incidence peaks in adolescence and young adulthood—and accounts for 5% to 10% of chronic sinusitis cases. Affected patients are atopic and immunocompetent and demonstrate a positive allergy skin test(s) or serum IgE to the causative mold. Hyperattenuation of the inspissated mucus is often seen on CT or MRI scans and represents accumulated heavy metals and precipitated calcium salt.
The diagnosis is based on 4 criteria1:
•Surgically obtained allergic mucin.
•Allergic mucin demonstrating fungal hyphae and/or sinus culture, positive for fungus.
•No evidence of invasive disease, necrosis, granulomas, or giant cells.
•Exclusion of other fungal sinus disorders.
The main causative organisms include the dematiaceous fungi (Bipolaris, Curvularia, and Alternaria) and less commonly Aspergillus species. The pathophysiology is still unknown, although it probably involves superantigens produced by fungi and hypertrophic sinus disease, either as a complication or risk factor for allergic fungal rhinosinusitis. The most widely accepted therapy includes surgical debridement (typically with FESS) followed by a course of oral corticosteroids for 3 to 12 months.2,3 Long-term corticosteroid therapy may produce significant adverse effects; however, patients who receive a prolonged course have fewer recurrences and require fewer repeated surgical procedures. Results of allergen-specific immunotherapy are conflicting. Because patients demonstrate type I IgE-hypersensitivity to the causative fungi, allergen immunotherapy may decrease the immunological response. However, this patient was receiving allergy injections that consisted of multiple aeroallergens, including Curvularia, for 4 years before presentation and still had a high Curvularia-specific IgE level of 28.3 kU/L. The use of topical antifungal sprays, such as amphotericin B or tobramycin, for chronic rhinosinusitis is controversial, and outcomes have not been well studied in this setting.
The most widely accepted therapy includes surgical debridement (typically with FESS) followed by a course of oral corticosteroids for 3 to 12 months.2,3 Long-term corticosteroid therapy may produce significant adverse effects; however, patients who receive a prolonged course have fewer recurrences and require fewer repeated surgical procedures. Results of allergen-specific immunotherapy are conflicting. Because patients demonstrate type I IgE-hypersensitivity to the causative fungi, allergen immunotherapy may decrease the immunological response. However, this patient was receiving allergy injections that consisted of multiple aeroallergens, including Curvularia, for 4 years before presentation and still had a high Curvularia-specific IgE level of 28.3 kU/L. The use of topical antifungal sprays, such as amphotericin B or tobramycin, for chronic rhinosinusitis is controversial, and outcomes have not been well studied in this setting.
The most discouraging aspect of allergic fungal rhinosinusitis is that despite therapy, the disease usually recurs. Thus, close follow-up by an otolaryngologist is required.
1. Schubert MS. Allergic fungal sinusitis. Clin Allergy Immunol. 2007;20:263-271.
2. Schubert MS. Allergic fungal sinusitis. Otolaryngol Clin North Am. 2004;37:301-326.
3. DeShazo RD, Chapin K, Swain RE. Fungal sinusitis. N Engl J Med. 1997;337:254-259.


