Wolff-Parkinson-White Syndrome
Authors:
Ronda Lunn, MPH
JAS Medical Management, Miramar, Florida
Syed A. A. Rizvi, PhD, MBA, and Sultan S. Ahmed, MD
Nova Southeastern University, Fort Lauderdale, Florida
Ayman M. Saleh, PhD
King Saud bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia
Mian Hasan, MD
Vanguard Medical Group, Fort Lauderdale, Florida
Frantz Sainvil, PhD, MD, ScD
University of Science, Arts and Technology, Montserrat, British West Indies
Jasmin Ahmed, MD
Larkin Community Hospital, South Miami, Florida
Citation:
Lunn R, Rizvi SAA, Ahmed SS, Saleh AM, Hasan M, Sainvil F, Ahmed J. Wolff-parkinson-white syndrome. Consultant. 2017;57(11):675-677.
A 37-year-old woman presented to the office with intermittent dizziness, palpitations, and multiple syncopal episodes occasionally accompanied by numbness of the left arm. She had been experiencing these episodes for approximately 7 years.
She had been seen previously in an emergency department (ED) for a syncopal episode. Findings of a computed tomography (CT) scan of the brain done at that time were negative, and she performed the Valsalva maneuver in the ED without any effect. She recovered in the ED without any further intervention.
History and physical examination. The patient had no history of substernal chest pain, diaphoresis, or dyspnea. She denied a history of tobacco use or any substance abuse.
Her blood pressure was 120/78 mm Hg, her pulse rate was 75 beats/min, and her respiratory rate was 16 breaths/min at presentation. Her height was 167.6 cm and her weight was 76.2 kg, with a body mass index of 27.1 kg/m2. She had regular heart rate and rhythm. The apical impulse had a normal location and character, and S1 and S2 were normal. No murmurs, gallops, or rubs were detected. The patient had no carotid artery bruit. Her orthostatic blood pressure was normal, as were neurologic examination findings.
Diagnostic tests. Laboratory test results were as follows: total cholesterol, 167 mg/dL; high-density lipoprotein cholesterol, 38 mg/dL; low-density lipoprotein cholesterol, 104 mg/dL; triglycerides, 126 mg/dL; sodium, 138 mEq/L; potassium, 4.2 mEq/L; chloride, 103 mEq/L; carbon dioxide, 18 mEq/L; calcium, 8.8 mg/dL; thyrotropin, 0.43 mIU/L; and glycated hemoglobin, 5.9%.
Electrocardiography (ECG) results showed a very short PR interval (< 120 ms), QRS prolongation (> 120 ms), and a delta wave (Figure 1), indicating Wolff-Parkinson-White (WPW) syndrome. Echocardiography findings showed normal left ventricular size and function. Mild mitral and tricuspid valve regurgitation was detected, but it was not clinically significant. Results of a nuclear stress test with single-photon emission CT showed no wall motion abnormality and an ejection fraction of 70%. The impression was that there was no evidence of stress-induced ischemia. Results of lower-extremity venous Doppler ultrasonography were normal, with no evidence of deep-vein thrombosis.

Figure 1: ECG recorded at presentation showing a very short PR interval (< 120 ms), QRS prolongation (> 120 ms), and a delta wave, the hallmark features of Wolff-Parkinson-White syndrome.
Discussion >>
Discussion. WPW syndrome is one of the preexcitation disorders and is characterized by an alternative electrical pathway between the atria and the ventricles, bypassing the atrioventricular node and causing preexcitation of the ventricles. In 1930, Louis Wolff, John Parkinson, and Paul D. White described the cases of 11 young healthy persons with a bundle branch block pattern on ECG, with shorter PR intervals, wide QRS complexes, and paroxysms of tachycardia.1 In 1942, Wood and colleagues reported the first histologic evidence of accessory connections discovered during the autopsy of a 16-year-old patient with paroxysmal tachycardia.2 It was not until 1970 when electrophysiology studies provided concrete evidence that the alternative electrical pathway is the source of preexcitation syndrome.3
This accessory pathway is present at birth. It can be a result of genetic mutation and also is associated with the Ebstein anomaly, but in most cases, the cause is unknown. WPW syndrome is more prevalent in males than in females,4 and it affects 0.13% to 0.25% of the population.5,6 It can cause tachycardia, chest pain, dyspnea, palpitations, dizziness, and syncope, although some patients remain asymptomatic. Symptoms can emerge at any age, but onset typically occurs between 11 and 50 years.7 In approximately 25% of WPW cases, symptoms resolve without treatment; however, atrial fibrillation can develop in approximately 10% to 30% of cases.
Treatment of WPW is based on risk stratification to assess whether individuals are at risk of sudden cardiac death (SCD). Risk stratification is assessed via various methods and includes a history of syncope or heart rate variability and the use of signal-averaged ECG, QT dispersion measurement, baroreflex sensitivity testing, and programmed electrical stimulation.8
Vagal maneuvers to break arrhythmias are mainstay of noninvasive management. Direct-current cardioversion is used in symptomatic tachycardia. WPW is commonly treated with radiofrequency catheter ablation therapy, which has an 85% to 95% success rate of eliminating the abnormal pathway.6 Other treatment options include antiarrhythmic medications. Asymptomatic patients may require only observation.9
Outcome of the case. Our patient was experiencing multiple episodes of syncope and serious arrhythmias, which indicated a high risk of SCD.10 She underwent radiofrequency catheter ablation therapy by a cardiac electrophysiologist. An ECG repeated 8 days after the ablation procedure showed normal sinus rhythm with a normal axis. The delta wave was no longer present (Figure 2). The patient reported having no further episodes of syncope and arrhythmia.
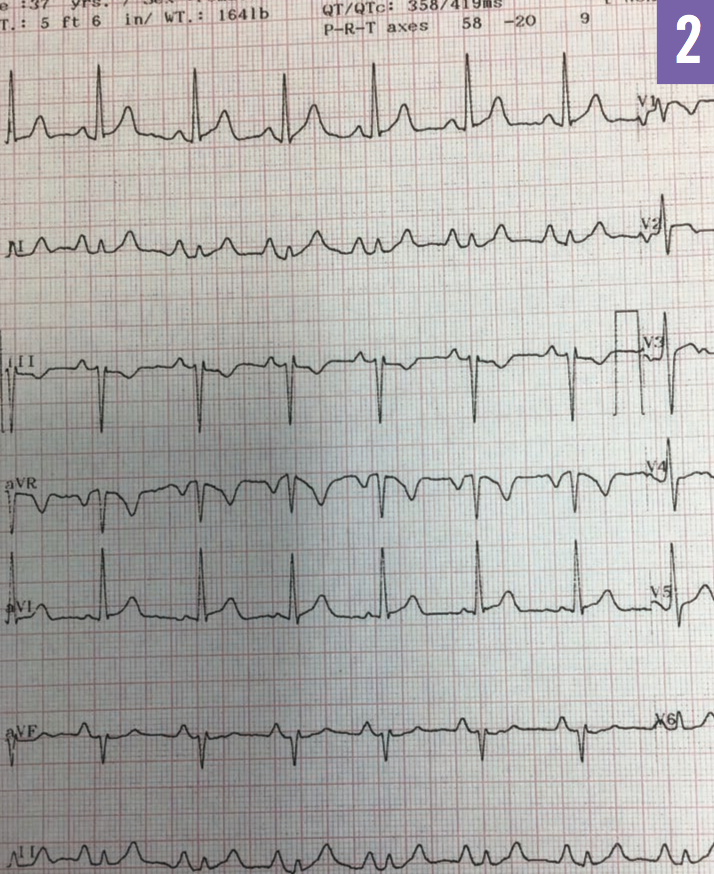
Figure 2: ECG recorded 8 days after radiofrequency catheter ablation therapy showing normal sinus rhythm with no delta wave present.
References:
- Wolff L, Parkinson J, White PD. Bundle-branch block with short P-R interval in healthy young people prone to paroxysmal tachycardia. Am Heart J. 1930;5(6):685-704.
- Wood FC, Wolferth CC, Geckeler GD. Histologic demonstration of accessory muscular connections between auricle and ventricle in a case of short P-R interval and prolonged QRS complex. Am Heart J. 1943;25(4):454-462.
- Hanon S, Shapiro M, Schweitzer P. Early history of the pre-excitation syndrome. Europace. 2005;7(1):28-33.
- Villareal RP, Woodruff AL, Massumi A. Gender and cardiac arrhythmias. Tex Heart Inst J. 2001;28(4):265-275.
- Prenni PG. Caring for the student with Wolff-Parkinson-White syndrome. J Sch Nurs. 2009;25(5):327-332.
- Bengali R, Wellens HJ, Jiang Y. Perioperative management of the Wolff-Parkinson-White syndrome. J Cardiothorac Vasc Anesth. 2014;28(5):1375-1386.
- Almendral J, Castellanos E, Ortiz M. Paroxysmal supraventricular tachycardias and preexcitation syndromes. Rev Esp Cardiol. 2012;65(5):456-469.
- Shekha K, Ghosh J, Thekkoott D, Greenberg Y. Risk stratification for sudden cardiac death in patients with non-ischemic dilated cardiomyopathy. Indian Pacing Electrophysiol J. 2005;5(2):122-138.
- Jetley P, Chatterjee R, Bafna U, Jetley NK. WPW syndrome: intricacies of anesthetic management in cesarean delivery. J Cardiol Clin Res. 2016;4(1):1052.
- Obeyesekere M, Gula LJ, Skanes AC, Leong-Sit P, Klein GJ. Risk of sudden death in Wolff-Parkinson-White syndrome: how high is the risk? Circulation. 2012;125(5):659-660.


