The Wheezing Infant: An Exercise in Differential Diagnosis
Author:
LaDonna Johnson, MD
Wayne State University
Citation:
Johnson L. The wheezing infant: an exercise in differential diagnosis. Consultant for Pediatricians. 2012;11(3):74-79.
ABSTRACT: The most important diagnostic tool in the evaluation of the wheezing infant is the history. After the initial assessment, further investigation is necessary to determine the underlying cause of wheeze. A sudden onset, associated fever, and the presence of other systemic symptoms suggest an infectious cause. Previous episodes of wheeze and a family or personal history of atopy are strong indicators of asthma and allergic rhinitis. The differential diagnosis of wheezing in the infant must also include rare causes of respiratory distress, such as foreign body aspiration, airway malacia, cystic fibrosis, and congenital anomalies.
Wheezing is a continuous musical whistling sound heard via chest auscultation during expiration. The sound is caused by increased, turbulent airflow through obstructed intrathoracic airways. Intrathoracic obstruction may be caused by bronchospasm, edema, or any space-occupying lesion. The assessment of wheezing in an infant requires sorting through a long list of differential diagnoses and is complicated by the difficulty in obtaining objective measurements of lung function in young children.1
Population studies show that 1 in 3 children experience at least 1 episode of wheezing before their third birthday and nearly 50% by their sixth birthday.2 In preschool-aged children and younger, most transient wheezing episodes are associated with viral infection, whereas persistent wheezing is associated with asthma later in life.3 Of children with asthma, about 25% start wheezing before 6 months of age and 75% by age 3 years.2
In medical school, I regularly heard the phrase “all that wheezes is not asthma.” Having transitioned into clinical practice, I find I must continue to be mindful of the rare, potentially overlooked causes of wheezing. This article serves as an opportunity to reassess the differential diagnostic process in the evaluation of the infant with wheeze who is brought for medical attention for the first time. I provide a diagnostic approach to help the busy pediatric practitioner quickly determine whether wheezing is self-limited, whether it may represent the beginning of a chronic respiratory disease, or—as in the case presented here—whether it may signal a potentially life-threatening condition.
CASE PRESENTATION
A 9-month-old girl, with no prior hospitalizations or surgeries, is brought for evaluation because she has not been eating well for the past day and, according to her mother, she has been “breathing funny.” The child has had no fevers. The mother has given her no medications.
Further investigation reveals a history of childhood asthma in both parents and “bronchitis” in the patient’s 3-year-old brother. There is no family history of allergic rhinitis or eczema. The infant has no cough, sick contacts, known triggers, new exposures, or personal history of allergic rhinitis or atopy. She has never been prescribed albuterol or oral corticosteroids. However, she was given 1 dose of albuterol nebulized solution via her brother’s nebulizer for congestion in the past and seemed to get better.
The infant was born at term and had an unremarkable newborn course; she was an active baby, with no developmental delays and normal growth. Results of newborn screening were negative. Her immunizations are up-to-date. She lives with her parents and brother in a house where there is occasional cigarette smoke exposure and no guns. They have a car seat and working smoke detectors.
On physical examination, the infant is fussy but consolable. Temperature is 37.6ºC (99.6ºF); heart rate, 110 beats per minute; blood pressure, 80/60 mm Hg; and respiration rate, 46 breaths per minute, with oxygen saturation of 92% on room air. The infant is noticeably tachypneic, with prolonged expiratory phase and nasal flaring but no other accessory muscle use. She has mild rhinorrhea without congestion, and expiratory wheezing with decreased aeration at the bases on lung examination.
Cardiovascular findings are normal, with regular heart rate and rhythm, no murmurs, normal perfusion, and 21 equal pulses in upper and lower extremities. The remaining physical findings are normal.
Nasal washes are negative for respiratory syncytial virus (RSV) and influenza A and B. A chest film shows some right middle lobe atelectasis versus infiltrate, consistent with small airways disease. The infant is given an intravenous bolus and admitted to the hospital.
What would you include in the differential diagnosis?
INITIAL ASSESSMENT
Parental perception of “wheeze.” One factor that may complicate the initial assessment of a wheezing infant is parental perception. In general, the sounds that parents may perceive as wheeze tend to vary widely and include many other respiratory sounds. In addition, parents who have some experience with chronic respiratory illnesses in other family members may have a lower threshold for reporting wheeze.
One study found that lung function in children with parentally reported wheeze was identical to that in children with no wheeze, and lung function in children with physician-confirmed wheeze was significantly poorer than that in the children with parentally reported wheeze and those with no wheeze.4 Thus, parents may have an inaccurate understanding of what the medical term “wheeze” means. Nevertheless, it is in the clinician’s best interest not to discount parental reports of current or past episodes of wheeze in a child, address parents’ concerns, and provide reassurance when appropriate.
Airway physiology. When taking functional differences into consideration, the airway is broken into 3 physiological segments: intrathoracic intrapulmonary, intrathoracic extrapulmonary, and extrathoracic extrapulmonary. The important distinction between each airway segment relates to how obstruction in that area differs in presentation.
Children naturally have smaller, more compliant airways and supporting structures, thus any narrowing of the airways can be significant, especially in the presence of disease. Under normal conditions, during inspiration, the intrathoracic airways tend to expand, because negative extraluminal pressure is greater than intraluminal pressure, and the extrathoracic airways, being exposed only to negative intraluminal pressure, tend to contract. The opposite process occurs with expiration.5 Thus, in a patient with extrathoracic obstruction, airway narrowing is more pronounced during inspiration. Likewise, in a patient with intrathoracic obstruction, airway narrowing worsens during expiration.
Is it wheeze or stridor? Wheeze is generally caused by intrathoracic obstruction, whereas stridor usually results from extrathoracic obstruction. Although the term “inspiratory wheeze” is sometimes used, any such sound heard on inspiration is technically considered stridor. Making this distinction affects the differential, intervention, and subsequent management.
Stridor in the infant and young child is more often associated with viral croup, bacterial tracheitis, epiglottitis, retropharyngeal or peritonsillar abscess, and laryngeal abnormality. Foreign body aspiration may present as wheeze or stridor depending on the location of the aspirated object. Laryngeal and tracheal foreign bodies may manifest as cough and stridor or voice change, whereas cough, dyspnea, and unilateral wheeze or decreased air movement suggest a bronchial foreign body.6
Tachypnea in relation to wheezing. According to the WHO, tachypnea in children aged 2 to 12 months is greater than 50 breaths per minute.7 By this definition, the 9-month-old girl in the case is not tachypneic. What was appreciated as tachypnea was probably increased work of breathing.
Respiration rate is influenced by the relationship between air flow and pressure gradients. At any point during the respiratory cycle, air flow stops when the gradient has been dissipated. Tachypnea refers to the speed at which gradient dissipation occurs. When there is obstruction or increased compliance of airways, as in asthma and emphysema, it takes longer for the pressure equilibration to occur. This results in a prolonged expiratory phase. When there is decreased compliance of airways, as in pneumonia and pulmonary edema, the lung cannot expand as well and it takes less time for pressure equilibration to occur. This results in tachypnea.
EVALUATION AND DIFFERENTIAL DIAGNOSIS
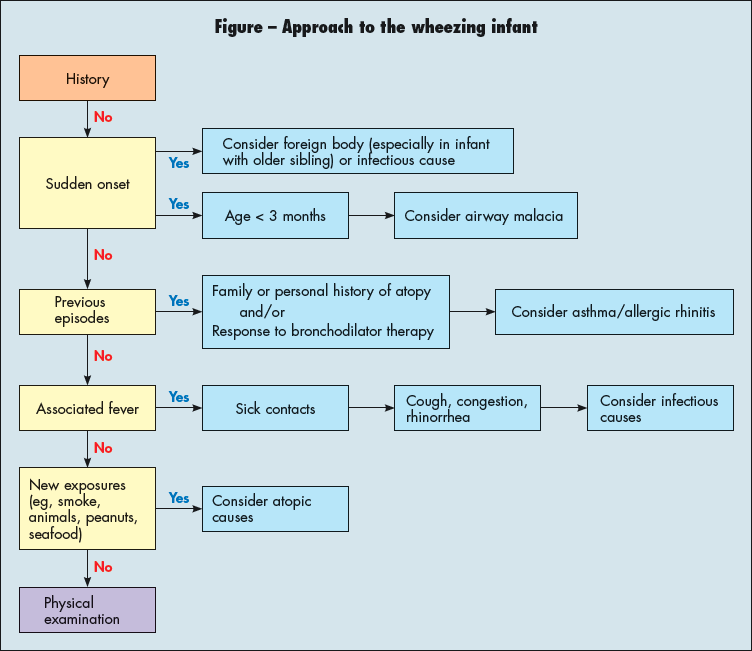
The most important diagnostic tool in the evaluation of the wheezing infant is the history. After the initial assessment, further investigation is necessary to determine the underlying cause of wheeze (Figure). The focus of the evaluation is on whether wheeze is associated with infection, allergy, or asthma or a combination of these conditions. A sudden onset, associated fever, and the presence of other systemic symptoms suggest an infectious cause. Previous episodes of wheeze and a family or personal history of atopy are strong indicators of asthma and allergic rhinitis. Wheeze triggered by exposure (eg, to animal dander, peanuts, or seafood ) suggests atopic causes.
Infectious causes. Viral bronchiolitis often affects children during the first 2 years of life. Symptoms on presentation typically include cough, tachypnea, increased work of breathing, and wheezing. Nasal congestion, rhinorrhea, and fever often precede the onset of respiratory symptoms by 1 to 2 days. The virus is present in the nasal secretions of infected children and is spread via cough, sneeze, or on hands that have been in contact with infected noses or eyes.
Commonly diagnosed viruses include RSV, parainfluenza virus, adenovirus, influenza virus, rhinovirus, and metapneumovirus. These may be detected in airway secretions via rapid antigen testing, immunoglobulin assays, or polymerase chain reaction.8
Of 12 randomized control trials that evaluated the efficacy of bronchodilators in infants with bronchiolitis, 9 showed that this therapy had no effect.9 However, of 5 randomized trials that evaluated nebulized adrenaline in bronchiolitis, all showed that this treatment yielded significant clinical improvement.9 There is some evidence to support the use of leukotriene receptor antagonists, specially montelukast, in bronchiolitis.10
Bronchopneumonia may be caused by a virus or bacteria. It affects the pulmonary parenchyma and can be acquired in the community or in health care settings. Infected children can present with fever, chills, cough, tachypnea, increased work of breathing, wheezing, chest pain, and sometimes with lower lobe pneumonias and abdominal pain.
The diagnosis and treatment of community-acquired pneumonia have been extensively outlined in the 2011 guidelines, which contain 92 recommendations. In terms of selecting antibiotic therapy, for uncomplicated pneumonia, the preferred treatment in the inpatient setting is ampicillin and in the outpatient setting is amoxicillin.11
Asthma. Asthma is the most common chronic disease in childhood and is a frequent cause of wheezing in children younger than 3 years. Young children with asthma often have a personal and family history of wheezing, eczema, and/or allergic rhinitis. Certain environmental exposures can lead to the development and exacerbation of asthma. The triggers most strongly associated with asthma are house dust mites, environmental tobacco smoke, cockroaches, rodents, cat dander, fungi, rhinovirus infections, and higher levels of ozone.12
Diagnosis of asthma in infants and young children requires:
- Use medical history and physical examination to determine that symptoms of recurrent episodes of airflow obstruction are present.
- Use of spirometry in all patients at least 5 years of age to determine that airway obstruction is at least partially reversible.
- Consideration of alternative causes of airway obstruction.1
Treatment of asthma focuses on:
- Reducing impairment (ie, prevent chronic symptoms, require infrequent use of short-acting ß2-agonist, and maintain normal lung function and activity levels).
- Reducing risk (ie, prevent exacerbations, loss of lung function, and reduced lung growth; minimize the need for emergency care or hospitalization; and ensure child has minimal to no adverse effects of therapy.1
In my hospital, an infant with a prior history of wheeze (1 episode or more) is treated with albuterol. The albuterol treatments are spaced according to the response and weaned as tolerated; oral corticosteroids are added if necessary. For any child with a prior history of wheeze, the family is asked to keep a “trigger journal,” which would help inform the child’s primary care provider in the event of future exacerbations.
Allergy-associated wheeze. In children with wheeze and a history of atopy or allergic rhinitis, the risk of developing asthma is increased. These children may initially be classified as having either bronchiolitis or asthma. However, they would still have to meet the diagnostic criteria for either condition.
A differential diagnosis of wheezing in the infant must also include rare conditions that may cause respiratory distress (Table).13 Some of the following conditions may be ruled out on the basis of the clinical presentation alone. Others may require further diagnostic testing.
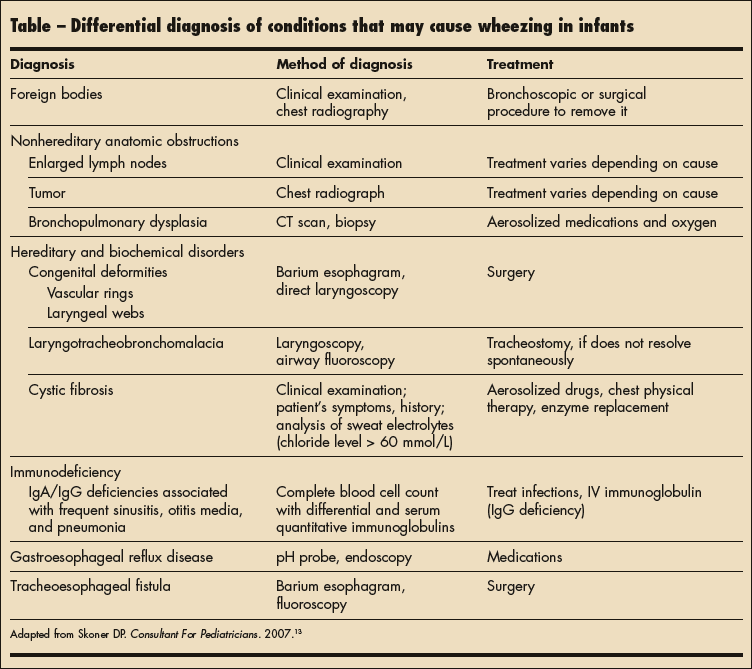
Foreign body. In young, mobile children with sudden onset of wheezing, foreign body aspiration is always a consideration. It should also be in the differential for infants with sudden onset of wheezing who have older siblings, especially siblings who are toddlers. The history may include a witnessed choking episode or period of unattended play.
The diagnosis of foreign body relies greatly on history. In terms of studies, radiographs may reveal a foreign body if it is radio-opaque. Chest radiograph may also show asymmetric air-trapping. Bronchoscopy can be used to both visualize and remove a foreign body from the airway.
Airway malacia. Laryngotrachobronchomalacia is caused by flaccidity of the supporting cartilage in the larynx, trachea, or bronchus. This causes airway narrowing, which leads to turbulent air flow manifested as wheezing or stridor depending on the location of the malacia. As stated above, in general, intrathoracic obstruction leads to expiratory wheeze and extrathoracic obstruction leads to inspiratory stridor. In children with malacia, wheezing becomes apparent within the first 3 months of life. The condition usually improves with age and worsens during respiratory infections.
Chest films in affected infants are usually normal, with bronchoscopy or laryngoscopy being the best way to make a definitive diagnosis.
Cystic fibrosis. Cystic fibrosis is the most common autosomal recessive fatal disease affecting white persons, with a frequency of 1 in every 2000 to 3000 live births. The disorder is caused by a mutation in the CFTR (cystic fibrosis transmembrane conductance regulator) protein and leads to increased thick secretions in the affected organs. As a result, children with cystic fibrosis have difficulty in clearing respiratory secretions and experience multiple respiratory tract infections.
Patients may present with multisystem involvement, including poor growth, constipation, persistent respiratory tract infections, biliary disease, nephrolithiasis, and signs of pancreatic insufficiency. Of the 1000 new cases diagnosed in 2001, more than 40% of them presented with respiratory symptoms.14
Diagnosis is based on clinical criteria and confirmed with biomedical testing. The majority of new cases of cystic fibrosis are diagnosed in childhood, and it is one of the diseases on state newborn screening tests.
Vascular ring. Vascular ring is an anatomical anomaly in which an abnormal relationship between the aortic arch and the trachea and/or esophagus results in compression and respiratory or GI symptoms. Vascular rings can be classified as either complete or incomplete. A complete vascular ring encircles both structures and an incomplete vascular ring affects only 1 of the 2 structures.
Patients typically present by 1 year of age with respiratory symptoms, specifically stridor, caused by tracheal compression. The initial study is usually a chest film to investigate underlying causes of repiratory symptoms and assess anatomy. Diagnostic studies for vascular ring may include barium swallow, CT, MRI, and bronchoscopy.
Other potential causes of respiratory distress and wheezing include tumors, bronchopulmonary dyspasia, laryngeal webs, gastroesophageal reflux disease, and tracheoesophageal fistula.
CASE CONCLUSION
Working through the differential. The physical examination findings and review of airway anatomy point to possible intrathoracic obstruction. The differential diagnosis includes the following conditions:
- Viral bronchiolitis. The diagnosis on admission is viral bronchiolitis. The infant is in the right age group for viral bronchiolitis, and her symptoms evolved within the appropriate time frame. Although she has no cough, she does have rhinorrhea and expiratory wheeze.
A trial of nebulized albuterol is ordered, even though it is understood that this treatment may not help. The infant’s work of breathing improves with this therapy; however, wheezing and air exchange are unaffected.
- Bronchopneumonia. Although the infant does have some symptoms associated with bronchopneumonia, namely increased work of breathing and wheeze, she is afebrile and without cough. Bronchopneumonia cannot be ruled out at this point. The patient’s chest radiograph is reviewed for peribronchial cuffing, streaking, and patchy atelectasis and is found to be negative for these findings. The more common clinical signs of pneumonia include fever, tachypnea, and hypoxia.
- Asthma. The infant’s strong family history and previous response to bronchodilator therapy suggest the possibility of an asthma diagnosis in her future. Because this is her first presentation with wheeze, it is too early to diagnose asthma.
- Foreign body aspiration. The infant has been crawling for several weeks and has a 3-year-old brother. The mother reports no history of choking or any known aspiration. Foreign body is still a consideration, especially in light of the chest film findings, showing right middle lobe infiltrate.
- Airway malacia. Malacia is unlikely to be the cause of wheezing in this infant because she is 9 months old, and this is the first physician documentation of wheeze.
- Cystic fibrosis. This patient is at higher risk for cystic fibrosis because she is white. However, she has had at most only 2 respiratory infections, according to her parents. Newborn screening for cystic fibrosis was negative. Her growth has been normal. This diagnosis may be considered in the event her condition does not improve.
- Vascular ring. A vascular ring is considered because of the wheezing, decreased oral intake, and the infant's age. However, the chest film findings point toward another cause.
Patient outcome. Following the trial of bronchodilator therapy, inhaled epinephrine was attempted without improvement. The infant was then fitted with a high-flow nasal cannula for oxygen therapy; however, the wheezing persisted. The pediatric pulmonary medicine team was consulted, and the patient underwent bronchoscopy the next day. During the procedure, a peanut was found in the right main bronchus and removed. She recovered well and was discharged home in stable condition.
REFERENCES:
- National Asthma Education and Prevention Program Expert Panel Report 3. Guidelines for the diagnosis and management of asthma. Summary Report 2007. NIH; National Heart, Lung, and Blood Institute. October 2007. Publication 08-5846.
- Brand PL, Baraldi E, Bisgaard H, et al. Definition, assessment and treatment of wheezing disorders in preschool children: an evidence-based approach. Eur Respir J. 2008;32:1096-1110.
- Liu AH. Natural history of allergic diseases and asthma. In: Leung DY, Sampson HA, Raif S, et al, eds. Pediatric Allergy: Principles and Practice. St Louis: Mosby; 2003.
- Lowe L, Murray CS, Martin L, et al. Reported versus confirmed wheeze and lung function in early life. Arch Dis Child. 2004;89:540-543.
- Clark J. Wheezing child. Clin Pediatr (Phila). 2008;47:191-198.
- Mace SE, Olaru C, Effron D. Stridor in the neonate and young child: evaluation and treatment of underlying causes. Consultant For Pediatricians. 2011;10:379-386.
- World Health Organization. The management of acute respiratory infections in children. Practical guidelines for outpatient care. Geneva: World Health Organization; 1995.
- Hall CB, Lieberthal AS. Viral testing and isolation of patients with bronchiolitis. Pediatrics. 2007;120: 893-894.
- Schindler M. Do bronchodilators have an effect on bronchiolitis? Crit Care. 2002;6:111-112.
- Fitzgerald DA, Mellis CM. Leukotriene receptor antagonists in virus-induced wheezing: evidence to date. Treat Respir Med. 2006;5:407-417.
- Bradley JS, Byington CL, Shah SS, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53:e25-e76.
- Takaro TK, Krieger JW, Song L. Effect of environmental interventions to reduce exposure to asthma triggers in homes of low-income children in Seattle. J Expo Anal Environ Epidemiol. 2004;14: S133-S143.
- Skoner DP. Wheeze in preschool children: therapeutic challenges with controller medications. Consultant For Pediatricians. 2007;6:205-214.
- Cystic Fibrosis Foundation Patient Registry. 2001 Annual data report to the center directors. Bethesda, MD: Cystic Fibrosis Foundation; 2002.
Dr Johnson is clinical assistant professor of pediatrics at Wayne State University and the Children’s Hospital of Michigan in Detroit. She is also a fellow of the American Academy of Pediatrics.


