What Is This Skin Eruption?
Authors:
Yi Chun Lai, MD, MPH; Usha Alapati, MD; and Viktoryia Kazlouskaya, MD, PhD
Citation:
The Dermatologist. 2018;26(3):47-50.
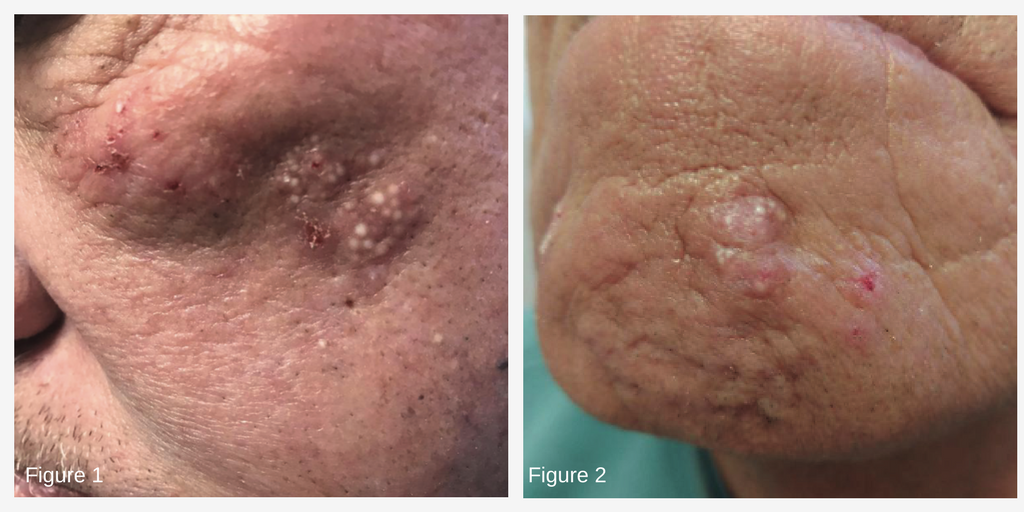
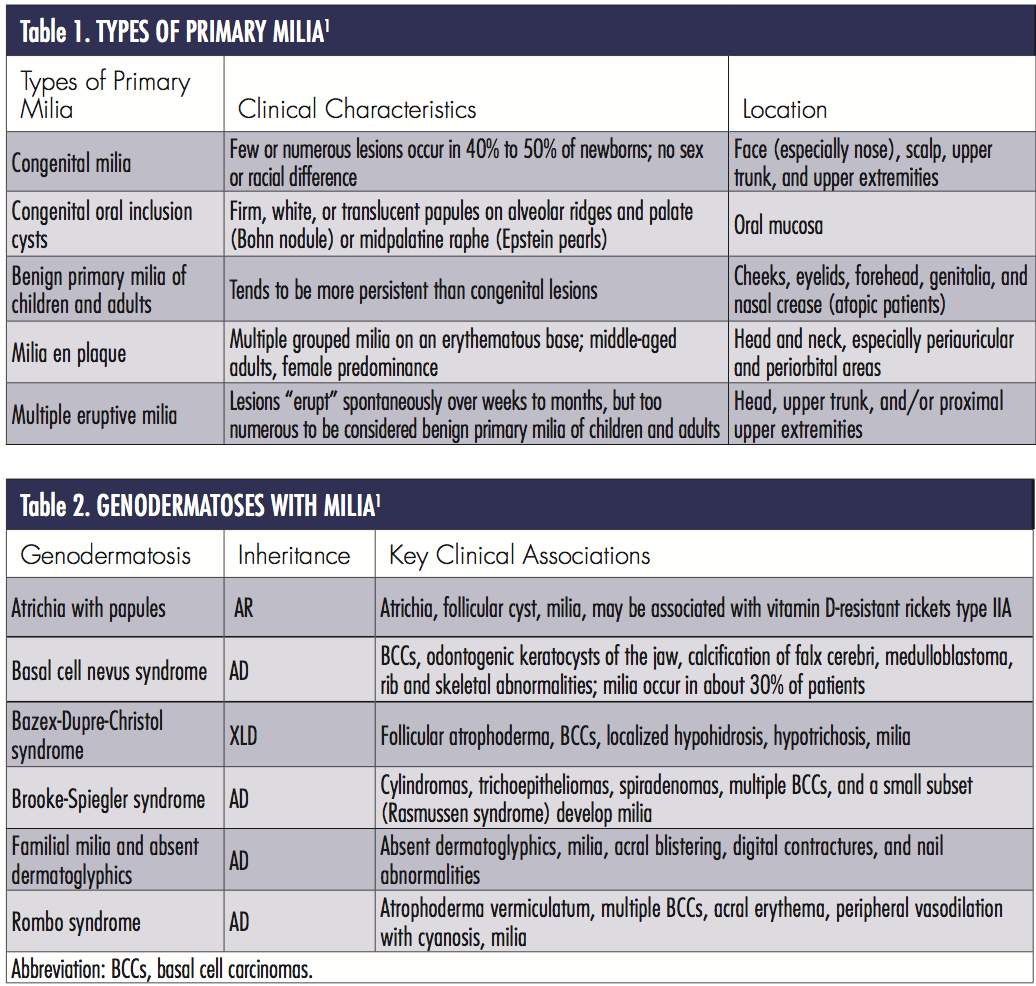
Two patients presented with unusual skin eruptions. In case 1, a 68-year-old white man presented with plaques on the bilateral cheeks of several months’ duration. The plaques were asymptomatic, however, the patient said he picked at the lesions. Otherwise, the patient was healthy and had a noncontributory past medical history (Figure 1). In case 2, an 81-year-old white man with a history of biopsy-proven prurigo nodularis presented with 2 plaques on the chin. He said he picked at the area frequently and later noticed some white spots on the old lesion. Otherwise, the patient denied pruritus, pain, or any other symptoms (Figure 2). His past medical history was noncontributory.
What is your diagnosis?

A milium is a small (1-2 mm), superficial keratin-filled cyst that presents as a white, dome-shaped papule.1 Milia may arise spontaneously without an underlying disorder or secondary to trauma, a medication, or another skin condition. Milia en plaque (MEP) is a rare variant of primary milia characterized by numerous grouped milia on an edematous, erythematous base. Since the term MEP was coined, no more than 50 to 60 cases have been reported in the literature.2
Clinical Presentation
MEP is an uncommon benign condition that presents as multiple, tiny, white papules situated within an erythematous plaque. MEP is typically asymptomatic. It preferentially involves the head and neck area, including nose, forehead, cheeks, scalp, periauricular, periorbital, submandibular, and supraclavicular regions1,3-8 (Figures 1 and 2).

Lesions can be unilateral or bilateral.1 A linear MEP following Blaschko lines has also been described.9 MEP mostly arises in healthy individuals, though it has been found to be associated with pseudoxanthoma elasticum, discoid lupus erythematosus, lichen planus, systemic amyloidosis, trauma, and renal transplantation.10-17 Certain medications, specifically cyclosporine, may be involved in the development of MEP.16,17 Additionally, a case of MEP co-existing with cutis laxa was described in a patient who was taking penicillamine for more than 50 years.18 Dermoscopy is helpful in diagnosing early, inconspicuous milia (Figure 3).
Epidemiology
While MEP is classically described as an entity that primarily affects middle-aged adults with a slight female predominance, a few pediatric cases4 and 2 congenital cases7,19 have also been reported. The average duration between lesion onset and diagnosis is 9 months.20There is no known ethnic/racial, geographical, or genetic predisposition.20
Differential Diagnosis
The main differential diagnoses of MEP include, but are not limited to, nevus comedonicus, Favre-Racouchot syndrome, follicular mucinosis, trichoadenoma, steatocystoma multiplex, folliculotropic mycosis fungoides, as well as acne, especially chloracne and iododerma.1Acne and nevus comedonicus can be distinguished clinically by papules with a central dark, hyperkeratotic plug. Favre-Racouchot syndrome is differentiated by multiple large comedones on a background of actinic damage. Steatocystoma multiplex is characterized by small semitranslucent cysts that may drain oily, yellow fluids. Other entities can be distinguished from MEP by characteristic histopathological features.
Pathogenesis and Histology
The pathogenesis of MEP remains elusive and most cases are idiopathic. Boehm and colleagues11 proposed that damage to adnexal structures from underlying diseases results in the formation of milia. MEP after cryotherapy has been described, supporting the theory of trauma-induced milia.21 Kouba and colleagues12 suggest that alteration in the infundibulum of a hair follicle, which causes impaired keratinization and outlet obstruction, plays a role in de novo MEP. Ghosh and Sangal7 postulate that intrauterine alteration in the infundibular portion and subsequent migration of the dysfunctional tissue contributes to the Blaschkoid pattern seen in congenital MEP. Based on histopathological features, Terui and colleagues suggest that MEP may represent a hamartoma, similar to a tumor of follicular infundibulum and trichoadenoma.22
Histopathology of MEP typically demonstrates multiple keratin-filled epidermoid cysts at various levels of the dermis accompanied by variable mixed lymphocytic infiltrates.22Branched epithelial proliferations budding from the epidermis were described by some authors.2,3,5,6,22-26 Keratin-filled cysts surrounding by mononuclear infiltrates were sometimes seen in those epithelial proliferations.22
Treatment

Although MEP is a benign condition, treatment is warranted if it causes a significant cosmetic disfigurement. Standard treatment for MEP has not been established, but the condition can be treated with either medical or surgical modalities, including topical/oral retinoids, minocycline, photodynamic therapy, simple extraction, cryotherapy, ablative laser therapy, dermabrasion, electrodesiccation, or excision, with variable successes depending on the depth of the lesions.2,20,27-32 Simple extraction and topical tretinoin are generally effective for superficial lesions. Rarely, spontaneous resolution may occur. It should be noted, however, that recurrence is not uncommon. 5
Our Patients
Biopsy was performed on both of our patients and the diagnosis of MEP was confirmed (Figures 4-7). The first patient preferred topical treatment with tretionin 0.1% cream and reported clinical improvement in 1 month. Extraction of milia was performed on the second patient with a satisfactory cosmetic outcome. Given the history of manipulation, trauma most likely contributed to the development of MEP in both of our patients.
Conclusion
To the best of our knowledge, this is the first reported case of MEP associated with prurigo nodularis. In addition, it occurred on the mental region, a location that has yet been reported in the literature. It is important for clinicians to be able to recognize MEP, a rare variant of primary milia (other types are listed in Tables 1 and 2), and its association with other skin conditions. Clinicians should also provide patients with reassurance as well as education on avoiding excessive manipulation of the lesion.
Dr Lai is with the department of dermatology at SUNY Downstate Medical Center in Brooklyn, NY.
Dr Alapati is with the department of dermatology at the Veterans Hospital in Brooklyn, NY.
Dr Kazlouskaya is with the department of dermatology at SUNY Downstate Medical Center in Brooklyn, NY.
Disclosure: The authors report no relevant financial relationships.
References
1. Berk DR, Bayliss SJ. Milia: a review and classification. J Am Acad Dermatol. 2008;59(6):1050-1063.
2. Ishiura N, Komine M, Kadono T, Kikuchi K, Tamaki K. A case of milia en plaque successfully treated with oral etretinate. Br J Dermatol. 2007;157(6):1287-1289.
3. Alsaleh QA, Nanda A, Sharaf A, Al-Sabah H. Milia en plaque: a new site. Int J Dermatol. 2000;39(8):614-615.
4. Nambudiri VE, Habib N, Arndt KA, Kane KS. Milia en plaque of the nose: report of a case and successful treatment with topical tretinoin. Pediatrics. 2014;133(5):e1373-1376.
5. Fujita H, Iguchi M, Kenmochi Y, Fukunaga Y, Asahina A. Milia en plaque on the forehead. J Dermatol. 2008;35(1):39-41.
6. Cota C, Sinagra J, Donati P, Amantea A. Milia en plaque: three new pediatric cases. Pediatr Dermatol. 2009;26(6):717-720.
7. Ghosh S, Sangal S. Congenital milia en plaque on scalp. Indian J Dermatol. 2015;60(1):105.
8. Dogra S, Kanwar AJ. Milia en plaque. J Eur Acad Dermatol Venereol. 2005;19(2):263-264.
9. Lee SH, Kim SC. Linear milia en plaque on the central face: an acquired skin rash following Blaschko’s lines? J Dermatol. 2012;39(11):936-937.
10. Cho SH, Cho BK, Kim CW. Milia en plaque associated with pseudoxanthoma elasticum. J Cutan Pathol. 1997;24(1):61-63.
11. Boehm I, Schupp G, Bauer R. Milia en plaque arising in discoid lupus erythematosus. Br J Dermatol. 1997;137(4):649-651.
12. Kouba DJ, Owens NM, Mimouni D, Klein W, Nousari CH. Milia en plaque: a novel manifestation of chronic cutaneous lupus erythematosus. Br J Dermatol. 2003;149(2):424-426.
13. de Wet J, Jordaan HF, Visser WI. Bilateral malar milia en plaque as primary presentation of discoid lupus erythematosus. JAAD Case Rep. 2017;3(2):106-109.
14. Losada-Campa A, De La Torre-Fraga C, Cruces-Prado M. Milia en plaque. Br J Dermatol. 1996;134(5):970-972.
15. Dickison P, Howard V, Wylie B, Smith SD. Localized axillary milia en plaque: a rare cutaneous case presentation of systemic amyloidosis. Clin Exp Dermatol. 2016;41(7):764-767.
16. Carrington PR, Nelson-Adesokan P, Smoller BR. Plaque-like erythema with milia: a noninfectious dermal mucinosis mimicking cryptococcal cellulitis in a renal transplant recipient. J Am Acad Dermatol. 1998;39(2 Pt 2):334-337.
17. Dogra S, Kaur I, Handa S. Milia en plaque in a renal transplant patient: a rare presentation. Int J Dermatol. 2002;41(12):897-898.
18. Vajdi T, Lee WW, Paravar T. Penicillamine-associated cutis laxa and milia en plaque - case report and review of cutaneous changes associated with penicillamine. Dermatol Online J. 2016;22(5).
19. Wang AR, Bercovitch L. Congenital milia en plaque. Pediatr Dermatol. 2016;33(4):e258-e259.
20. Stefanidou MP, Panayotides JG, Tosca AD. Milia en plaque: a case report and review of the literature. Dermatol Surg. 2002;28(3):291-295.
21. Beutler BD, Cohen PR. Cryotherapy-induced milia en plaque: case report and literature review. Dermatol Online J. 2014;21(2).
22. Terui H, Hashimoto A, Yamasaki K, Aiba S. Milia en plaque as a distinct follicular hamartoma with cystic trichoepitheliomatous features. Am J Dermatopathol.2016;38(3):212-217.
23. Hubler WR Jr, Rudolph AH, Kelleher RM. Milia en plaque. Cutis. 1978;22(1):67-70.
24. Stork J. Retroauricular bilateral milia en plaque. Dermatology. 1995;191(3):260-261.
25. Combemale P, Faisant M, Dupin M. Milia en plaque in the supraclavicular area. Dermatology. 1995;191(3):262-263.
26. Samlaska CP, Benson PM. Milia en plaque. J Am Acad Dermatol. 1989;21(2 Pt 2):311-313.
27. Leverkus M, Rose C, Bröcker EB, Goebeler M. Follicular cutaneous T‑cell lymphoma: beneficial effect of isotretinoin for persisting cysts and comedones. Br J Dermatol.2005;152(1):193-194.
28. Noto G, Dawber R. Milia en plaque: treatment with open spray cryosurgery. Acta Derm Venereol. 2001;81(5):370-371.
29. Sandhu K, Gupta S, Handa S. CO2 laser therapy for milia en plaque. J Dermatol Treat. 2003;14(4):253-255.
30. van Lynden‑van Nes AM, der Kinderen DJ. Milia en plaque successfully treated by dermabrasion. Dermatol Surg. 2005;31(10):1359-1362.
31. Al-Mutairi N, Joshi A. Bilateral extensive periorbital milia en plaque treated with electrodesiccation. J Cutan Med Surg. 2006;10(4):193-196.
32. Lee KY, Oh SW, Kim SC. A case of milia en plaque treated with modified rhomboid transposition flap. Korean J Dermatol. 2007;45:1227-1229.


