What Is This Adolescent’s Painful, Hyperkeratotic Foot Lesion?
A 17-year-old male athlete presented with a painful lesion on his right sole of approximately 6 months’ duration. Over time, the lesion had slowly increased in size and had become more painful. He recalled that he had bought a new pair of tight-fitting shoes 8 months previously. He used to be very active in sports, especially jogging and golfing. Because of the pain, he had jogged and golfed a lot less recently.
The patient was otherwise in good health. In particular, he had no history of diabetes, rheumatoid arthritis, or neurologic disease. Physical examination revealed a hyperkeratotic lesion on the right sole (Figure 1).
The lesion was exquisitely tender on standing or when direct or lateral pressure was applied to it. The rest of the physical examination findings were normal.
What’s your diagnosis?
(Answer and discussion on next page)

Figure 1. Hyperkeratotic lesion on the right sole.
Answer: Plantar Corn (Clavus)
The patient had a plantar corn (also known as plantar clavus). The lesion was treated by sharp deep paring with removal of sequential layers of keratin and the central keratin core. The pain subsided immediately after the procedure. He was advised to use a cream with a high concentration of urea on the affected area after bathing. An assessment for orthotics was scheduled.
A corn is a painful, circumscribed, hyperkeratotic lesion with a central conical core of keratin that develops in response to chronic friction or pressure.1
Epidemiology
Corns are one of the most common foot conditions seen after puberty and are especially common in elderly individuals.2 In a study of 784 community-dwelling adults aged 65 years or older, approximately 58% had corns and/or calluses.2 Corns were more commonly observed in the African American population than in the non-Hispanic white and Puerto Rican populations in that study.2 There is a slight female predominance.2
The condition is more common in those who wear poorly fitted or high-heeled shoes, those who participate in sports, and those with foot deformities (eg, hammertoe deformity, burrowing and curling of the lesser toes, bunion, exostoses, bony spur, rheumatoid arthritis), diabetes mellitus, psoriasis, and peripheral neuropathy.1,3,4
Pathogenesis
The stratum corneum thickens in response to local chronic pressure or friction to protect the irritated skin.1 It has been postulated that when subjected to stress, the stratum corneum is capable of producing growth factors and inflammatory mediators. These chemicals may increase the transit time of epidermal cells with resultant accumulation of immature cells. If the pressure or friction is focused on a localized area of the skin, the impaction of the stratum corneum can lead to the formation of a hard keratin plug—the hallmark of a corn. The corn so formed induces increasing pressure on the area, resulting in a vicious cycle.5
Histopathology
Histologic examination of a corn reveals a very dense collagen plug surrounded by marked dense, parakeratotic stratum corneum and increased collagenization of the superficial dermis.
Clinical Manifestations
Two types of corns have been described: hard corn (heloma duram) and soft corn (heloma molle).1 The former is more common than the latter. Both types of corns are very painful because they are sharp and deep.6 The size of the lesion is usually less than 1.5 cm in diameter. A hard corn typically presents as a dry, horny, dome-shaped papule with a shiny, polished surface and a hard, central conical core of hard keratin. The lesion most commonly is found over an area that is subjected to friction, trauma, or pressure, such as the dorsum of the interphalangeal joint, the dorsolateral aspect of the fifth toe, or the plantar surface beneath the metatarsal. In the latter case, it is referred to as a plantar corn, as is illustrated in the present case (Figure 1).
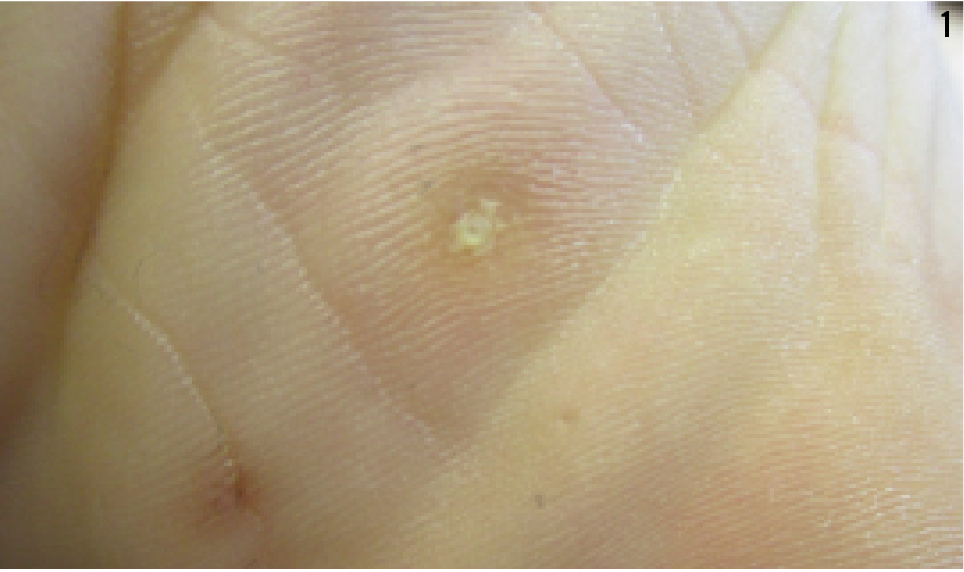
Figure 1. Plantar (hard) corn.
A soft corn is described as such because of its macerated appearance secondary to absorption of moisture from inadequate drainage of perspiration (Figure 2). The lesion is boggy and appears white and rubbery. A soft corn generally is found in interdigital areas, especially between the fourth and fifth toe.

Figure 2. Soft corn.
Diagnosis
The diagnosis is mainly a clinical one based on the characteristic clinical appearance. The diagnosis can be aided by dermoscopy, which typically shows a translucent central core known as a nucleus.7 Referral to a dermatologist or podiatrist sometimes is required for diagnostic clarification.
Differential Diagnosis
A corn should be differentiated from a callus. Although the two conditions share more or less the same etiologies, their clinical presentations are different. A corn is a narrow-based, sharply defined, and deep lesion that often presents as a dome-shaped papule with a central core.6 Paring of a corn yields a translucent, compressed, whitish yellow core at the center.
On the other hand, a callus is a broad-based, superficial lesion with poorly demarcated borders. Paring of a callus reveals layers of yellowish keratin without a central core. While a corn often causes significant discomfort and pain, a callus (unless fissured) usually results in no pain.4 A corn usually is less than 1.5 cm in diameter, in contrast to a callus, which can be of any size. A corn and callus also can be present in the same lesion, and paring down the callus can reveal an underlying focal corn.
Other differential diagnoses include a plantar wart, a digital mucous cyst, and a dermatofibroma. Typically, plantar warts present as multiple, firm, rough papules that coalesce into a mosaic plaque, disrupting normal dermatoglyphics. Tiny black dots may be visible at the surface of the wart. These black dots represent thrombosed, dilated capillaries. Trimming the surface keratin makes the capillaries more prominent. The tiny black dots at the surface of the lesion are pathognomonic of plantar warts.
A digital mucous cyst is a benign, cystic lesion of the digit that typically is located near the distal interphalangeal joints or near the proximal nail folds.8 Two types of digital mucous cysts have been described. The myxomatous (superficial) type presumably arises de novo from the metabolic derangement of dermal fibroblasts that leads to excess production of hyaluronic acid. The ganglionic (deep) type results from leakage of fluid from the distal interphalangeal joint. There may be coexisting osteoarthritis and osteophytes in the joint. Characteristically, a digital mucous cyst presents as an asymptomatic, slow-growing, solitary, circumscribed, semitranslucent, flesh-colored, compressible, dome-shaped, cystic papulonodule measuring 1 to 10 mm in diameter on the digit.8
Typically, a dermatofibroma presents as an asymptomatic red or reddish brown firm nodule. The lesion is attached to the skin but not to the underlying structure. Although a dermatofibroma can develop anywhere in the body, the lesion most commonly is found on the limb. The size varies from a few millimeters to 2 cm. Pinching of the lesion results in dimpling of the lesion (dimple sign or Fitzpatrick sign).
Complications
A plantar corn can cause foot pain that and may restrict ambulatory activities. The condition can be incapacitating, especially for those individuals who have to stand or bear weight for long hours. In the population with diabetes, a plantar corn is highly predictive of subsequent plantar ulceration. A soft corn, on the other hand, is prone to secondary bacterial or fungal infection, especially in those individuals with diabetes mellitus or immunosuppression.
Prognosis and Management
Corns tend to recur unless the underlying cause is removed.
The importance of wearing properly fitted footwear and the use of appropriate orthotics cannot be overemphasized. Paring of the corn and sharp debridement of the central keratin core using a chisel or No. 15 blade will provide prompt relief to the area.1,5
Alexander K. C. Leung, MD, is a clinical professor of pediatrics at the University of Calgary and a pediatric consultant at the Alberta Children’s Hospital in Calgary, Alberta, Canada.
Benjamin Barankin, MD, is a dermatologist and the medical director and founder of the Toronto Dermatology Centre in Toronto, Ontario, Canada.
References
- Freeman DB. Corns and calluses resulting from mechanical hyperkeratosis. Am Fam Physician. 2002;65(11):2277-2280.
- Dunn JE, Link CL, Felson DT, Crincoli MG, Keysor JJ, McKinlay JB. Prevalence of foot and ankle conditions in a multiethnic community sample of older adults. Am J Epidemiol. 2004;159(5):491-498.
- Gillet HG. Interdigital clavus: predisposition is the key factor of soft corns. Clin Orthop Relat Res. 1979;(142):103-109.
- Leung AKC, Barankin B. What is causing this man’s foot lesion? Consultant. 2015;55(8):633-634.
- Lee WJ, Lee SM, Won CH, et al. Efficacy of intralesional bleomycin for the treatment of plantar hard corns. Int J Dermatol. 2014;53(12):e572-e577.
- Güngör Ş, Bahçetepe N, Topal İ. Removal of corns by punch incision: a retrospective analysis of 15 patients. Indian J Dermatol Venereol Leprol. 2014;80(1):41-43.
- Bae JM, Kang H, Kim HO, Park YM. Differential diagnosis of plantar wart from corn, callus and healed wart with the aid of dermoscopy. Br J Dermatol. 2009;160(1):220-222.
- Leung AKC, Barankin B. Digital mucous cyst. Aperito J Dermatol. 2015;2(1):108.


