Weight Loss in an Older Adult with Diabetes
An 80-year-old woman with a past medical history of type 2 diabetes mellitus, asthma, and recurrent urinary tract infections presented to our clinic complaining of decreased appetite and weight loss. The patient lost 17 lb over the past 6 months. She also reported a poor appetite and nausea. She denied history of rectal bleeding and melena. A 2011 colonoscopy had previously revealed an adenomatous polyp.
Physical examination. The patient was in no distress and had no oral lesions. There was no abdominal tenderness or palpable masses.
Laboratory tests. An evaluation revealed hemoglobin 10 g/dL, hematocrit 33%, and mean corpuscular volume of 65 fL. Her white blood cell count was 7.4 mmol/L and platelets were 399 x 109/L. Urinalysis showed red blood cells, trace blood, and a few bacteria. The urine culture showed no growth. Her hemoglobin A1c count was at 6.5%.
Subsequent laboratory test results revealed an iron serum level of 22 mg/dL, total iron-building capacity 218 g/dL, ferritin 697.8 ng/mL, thyroid-stimulating hormone (TSH) 2.22 nIU/L, vitamin B12 311 pg/mL, and a folate level of 4.8 ng/mL.
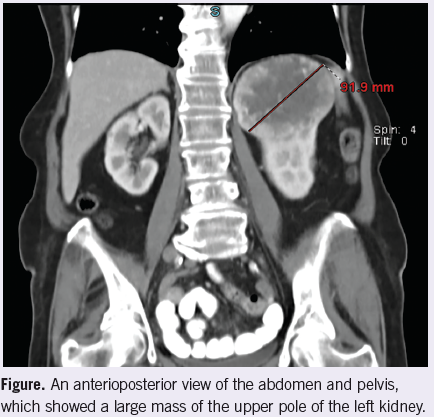
Radiology. A CT scan of the abdomen and pelvis showed a mass in the upper pole of the left kidney (Figure).
Discussion. Weight loss is common in older adults. It occurs in 15% to 20% of older patients. It is associated with functional decline, frailty, and increased mortality.1-3 Clinicians should review weight trends at every office visit. Although it is not abnormal for the patient’s weight to steadily decline with age, the acceptable rate of weight loss is approximately 0.1 kg to 0.2 kg per year.4 Clinically, significant weight loss in the older adult is defined as a decrease of ≥5% of usual body weight over a 6- to 12-month period.4 If the healthcare provider observes such weight loss, further investigation is warranted.
It is difficult to determine the cause of weight loss in older patients who have multiple medical and psychosocial challenges. Malignancy, chronic disease, depression, cognitive impairment, poor oral health, low income, and medication side effects are a few of the common reasons older adults lose weight.
There are no guidelines available to assist clinicians in the workup of these complex patients. Evaluation usually consists of a through history, physical examination, and laboratory tests, including a complete blood count, comprehensive metabolic panel, urinalysis, sedimentation rate, and TSH.
The clinician’s knowledge of the patient and family is also useful in determining whether or not further studies are appropriate. In the above patient, her physician did not suspect depression or cognitive impairment. Her chronic medical problems were well-controlled. The patient had 2 daughters—both nurses—who provided close observation and care to the patient. In light of the patient’s history of adenomatous polyps, anemia, and microscopic hematuria, colonic or genitourinary malignancy were high in the differential. Therefore, a CT scan of the abdomen and pelvis seemed to be the best, first imaging test to pursue.
Outcome of the case. The patient was referred to urology for evaluation, and underwent hand assisted laparoscopic nephrectomy of her left kidney. Pathology revealed clear cell renal cell carcinoma confined to the capsule. The patient had an uneventful postoperatively course. One month later, the patient was doing very well and had gained 7 lb.
References:
1.Gaddey HL, Holder K. Unintentional weight loss in older adults.
Am Fam Physician. 2014;89(9):718-722.
2.Stajkovic S, Aitken EM, Holroyd-Leduc J. Unintentional weight loss in older adults. CMAJ. 2011;183(4):443-449.
3.Robertson RG, Montagnini M. Geriatric failure to thrive. Am Fam Physician. 2004; 70(2): 343-350.
4.Smith KL, Greenwood C, Payette H, et al. An approach to the nonpharmacologic and pharmacologic management of unintentional weight loss among older adults. Geriatrics Aging. 2007;10(2):91-98.


