Ureteritis Cystica
A 43-year-old, previously healthy woman presented to the emergency department after having a syncopal episode while showering. She denied any prodrome prior to the syncopal episode and complained only of a short course of nausea and 2 bouts of vomiting afterward.
She reported an episode of syncope approximately 9 months prior, which was very similar to the one that prompted her presentation. Also of note, she reported a 1-year history of progressively worsening painless gross hematuria. She denied passage of clots. Her menstrual cycles were normal. Her history was otherwise notable for a 10 pack-year smoking history. She had no relevant family history.
On presentation, the patient’s hemoglobin level was 3.6 g/dL. Urine macroscopy results were positive for nitrites with small amounts of leukocyte esterase, although urine culture yielded no growth.
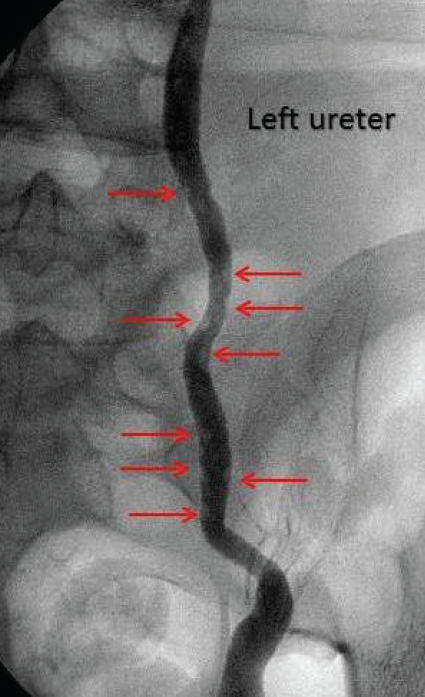
Figure 1. Multiple small lucent defects in the left ureter, indicated by red arrows.

Figure 2. Multiple small lucent defects in the right ureter, indicated by red arrows.
Diagnostic testing. Given her 1-year history of gross hematuria and severe anemia, a hematuria workup was initiated on an inpatient basis. An excretoryphase computed tomography urogram demonstrated numerous small filling defects in the bilateral ureters and urinary bladder. Given these findings, she underwent a retrograde pyelogram that confirmed the bilateral filling defects (Figures 1 and 2). A subsequent diagnostic ureteroscopy revealed multiple smooth-walled, cyst-like protrusions into the ureters bilaterally, consistent with ureteritis cystica.
Discussion. Ureteritis cystica is a rare disease with a benign course. It results from chronic, nonspecific inflammation of the urothelium1 and leads to glandular metaplasia. It has a higher predominance in women than in men and usually is unilateral, although bilateral cases have been documented.2 No specific symptoms are associated with the condition, and thus it usually is suggested incidentally by urinalysis or radiographic imaging,3 particularly during evaluation of urinary tract infections, lithiasis, and hematuria in as many as in 82%, 53%, and 52% of cases, respectively.4
Diagnosis is confirmed with the use of ureteroscopy, revealing numerous, small (< 5 mm), hemispheric filling defects in the ureter with or without involvement of the renal pelvis and bladder.5 The prognosis of ureteritis cystica is benign, with no malignant potential, and treatment is focused on eliminating the underlying disease. Given the rarity of the disease, the recurrence rate is unknown.
Outcome of the case. This patient’s underlying cause of ureteritis cystica was not clearly identified, highlighting the incidental finding of the disease. The patient received empiric treatment for a urinary tract infection with a 14-day course of ciprofloxacin, 250 mg twice a day. For her anemia, she acutely received 3 units of packed red blood cells and was placed on ferrous sulfate, 325 mg once a day. At a 2-week follow-up visit, her gross hematuria had improved significantly, and her hemoglobin level was stable. By 4 months, her hemoglobin had returned to the normal range.
In summary, ureteritis cystica is a benign disease affecting the urothelium and is usually diagnosed incidentally when addressing the underlying etiology, most frequently urinary tract infections and lithiasis. Treatment is based on addressing the suspected underlying etiology. As such, the disease has a good prognosis without increased risk for malignancy. The diagnosis should be considered in anemic patients with hematuria.
References:
- Mariño del Real J, Sevilla Zabaleta M, Cabello Padial J, Abengozar García-Moreno A, Mateos Blanco J. Cystic ureteritis: importance of chronic infection-inflammation as etiologic factor: report of a clinical case [in Spanish]. Actas Urol Esp. 2000;24(6):496-498.
- Duffin TK, Reagan JB, Hernández-Graulau JM. Ureteritis cystica with 17-year followup. J Urol. 1994;151(1):142-143.
- Rothschild JG, Wu G. Ureteritis cystica: a radiologic pathologic correlation. J Clin Imaging Sci. 2011;1(1):23.
- Padilla-Fernández B, Díaz-Alférez FJ, Herrero-Polo M, Martín-Izquierdo M, Silva-Abuín JM, Lorenzo-Gómez MF. Ureteritis cystica: important consideration in the differential diagnosis of acute renal colic. Clin Med Insights Case Rep. 2012:5:29-33.
- Poturalski MJ, Purysko AS, Herts BR. Ureteritis cystica. J Urol. 2015;193(4):1379-1380.


