Type 2 diabetes mellitus is becoming an increasing problem among children and adolescents.1,2 Type 1 diabetes mellitus is caused by deficiency of insulin secretion from pancreatic beta-cell damage. Type 1A is characterized by autoimmune destruction of pancreatic beta cells; type 1B refers to insulin-dependent diabetes not of immune cause. Type 2 diabetes occurs most often in adults and is associated with insulin resistance and a relative insufficiency of insulin.
In the past, 2% to 3% children with diabetes were thought to have type 2 disease.3 However, an increasing number of cases are being seen in pediatric clinics and in the general population. This increase in frequency is linked to the increase in childhood obesity. A study in 2000 from Ohio showed that 33% of African American and Caucasian children aged 10 to 19 years with diabetes had type 2 disease.4 It has been estimated that 4.1 per 1000 American children aged 12 to 19 years have diabetes and that 30% of these children have type 2 diabetes.5
Type 2 diabetes in children is associated with obesity, family history of type 2 diabetes, female sex, and ethnic background.4 In Canada, various aboriginal communities have been studied. One study found a high prevalence of childhood obesity that resulted in an increased risk of diabetes or impaired fasting glucose.6 Among the risk factors described, childhood obesity is the only one that can be altered and therefore should be the target for prevention strategies.
The early onset of type 2 diabetes is a serious health concern for children, since a significant portion of their life will be spent controlling this disease. Complications of diabetes are common; poor glycemic control of long duration can lead to significant morbidity, including macrovascular (peripheral vascular disease, coronary artery disease, and stroke) and microvascular (retinopathy, neuropathy, and nephropathy) complications.7 Obesity in itself can also lead to macrovascular complications and hypertension.
The new challenge to physicians is to prevent these problems from occurring through aggressive management of childhood obesity. Here we provide guidelines on detecting type 2 diabetes and on close monitoring of children with the disease.
Diagnosis of Type 2 Diabetes in Children

Detection of type 2 diabetes and close monitoring of children at risk is key to preventing complications.8 The Canadian Diabetes Association has defined a fasting plasma glucose level of 7 mmol/L or more as diabetes, 6.1 to 6.9 mmol/L as impaired fasting glucose, and between 4 and 6 mmol/L as normal. These are the same criteria currently in use for the adult population.9
It has been recommended that the fasting (no food for at least 8 hours) plasma glucose be used for the initial screening test. The test is fast, easy to perform, inexpensive, and more convenient than the oral glucose tolerance test.

75-g oral glucose tolerance test may be necessary when clinical suspicion is high but the fasting plasma glucose level is normal. With the oral glucose tolerance test, a 2-hour blood glucose value of 11.1 mmol/L or higher is considered a positive result for diabetes, 7.8 to 11 mmol/L is impaired glucose tolerance, and less than 7.8 mmol/L is normal. In the absence of significant symptoms and unequivocal metabolic decompensation, a confirmatory laboratory glucose test (either a fasting plasma glucose, casual plasma glucose or oral glucose tolerance test) must be done on a separate day.9

Children, like adults, may be asymptomatic for a long period before presenting with signs or symptoms of hyperglycemia in type 2 diabetes. Although diabetic ketoacidosis is commonly seen in type 1 diabetes, children with type 2 diabetes may present with diabetic ketoacidosis.10
Children should be screened for type 2 diabetes if they have a family history of type 2 diabetes, are from a high-risk ethnic group, are obese, or have polycystic ovary syndrome. Important historical and physical examination findings and laboratory investigations are shown in Tables 1, 2, and 3.
PREVENTION AND TREATMENT OF TYPE 2 DIABETES
In children with type 2 diabetes, treatment is best accomplished through the combined efforts of a multidisciplinary team.11 Ideally, patients should have access to dietitians, nurse educators, psychologists, social workers, and physicians. Type 2 diabetes has a significant impact on the entire family, and support should be offered if needed. Lifestyle modifications should involve all family members so that everyone can benefit from healthy eating habits and exercise.

Table 4 outlines available treatment options. The most appropriate and cost-effective treatment is decreased caloric intake and increased physical activity. In fact, strategies aimed at healthy lifestyle habits for children are the best way to prevent type 2 diabetes. Improved insulin sensitivity can be gained from weight loss, exercise, and maintaining an ideal body weight.12
Some studies have shown that metformin( is an effective treatment for adolescents with type 2 diabetes.13,14 A recent survey found that pediatric endocrinologists in the United States and Canada treat 44% of children who have type 2 diabetes with oral hypoglycemic agents. Among these children, 71% received metformin, 46% sulfonylureas, 9% thiazolidinediones, and 4% meglitinide.15 Unfortunately, many oral hypoglycemic agents used in adults with type 2 diabetes have not been licensed for use in the pediatric population. Until the safety and efficacy of these drugs is established, they cannot be recommended for routine clinical use.
There is a lot of experience with subcutaneous insulin injections in type 1 diabetes. Recently, such injections have been used in the early treatment of type 2 diabetes to decrease glucose toxicity and achieve target blood glucose levels.16 If appropriate lifestyle modification cannot be achieved and blood glucose targets are not maintained, it is reasonable to consider a short course of insulin therapy or metformin.
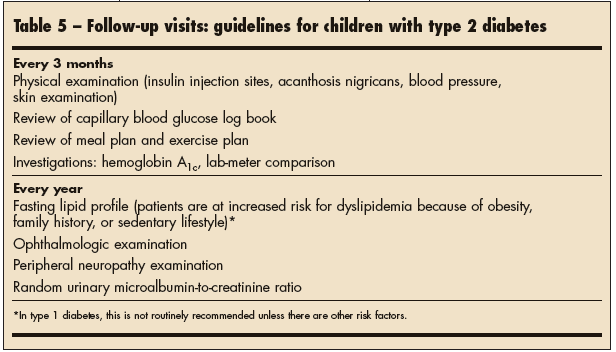
Follow-up for pediatric patients with type 2 diabetes should involve the family and a multidisciplinary team (Table 5). Children often feel well and do not see the benefits of rigorous blood glucose monitoring or dietary restrictions and exercise. The long-term risks of type 2 diabetes and the benefits of treatment are often not tangible to children. This can lead to frustration and poor compliance with treatment plans. Ongoing education and support is therefore essential in managing type 2 diabetes.
A unique situation faced by pediatric patients with type 2 diabetes is the transition to adult services. Issues that may arise include less frequent follow-up, different expectations of the patient, and compliance problems as the adolescent assumes sole care of his or her diabetes.
Are We Meeting The Challenge?
As the prevalence of childhood obesity increases in North America, we can expect the incidence of insulin resistance and type 2 diabetes to increase as well. Early detection of type 2 diabetes is difficult because children are often asymptomatic. Few medical options are available for pediatric patients with type 2 diabetes; the optimal therapy focuses on diet and exercise.
Management of diabetes involves changes in daily lifestyle that need to be consistent in the long term. However, health care professionals often face many barriers when treating children with diabetes.17 As noted, children may feel well and do not see any immediate benefits from treatment. Families may have socioeconomic constraints or cultural differences that can make it difficult to implement healthy lifestyles. Positive role models need to be in place to encourage children to exercise and eat healthy foods. Widespread societal adjustments must be made, including increased activity in school, changed accessibility to healthy food choices, different infrastructures to favor physical activity, safe outdoor play areas for children, and changes in advertising trends.18
In attempting to stop the development of type 2 diabetes and its complications, physicians need to focus on preventing obesity in all children--not just children in seemingly high-risk populations. The real challenge will be in overcoming barriers to implementing strategies for healthy lifestyles in our communities so that all children will benefit.


