Peer Reviewed
Pruritus in Children: What’s Itching?
Authors:
Alexander K. C. Leung, MD
University of Calgary
WM. Lane M. Robson, MD
Childrens Clinic
Citation:
Leung AKC, Robson WMLM. Pruritus in children: what’s itching? Consultant for Pediatricians. 2008;7(5):193-202.
ABSTRACT
In children, most causes of itching are the result of skin disease, not underlying systemic illness. The most common dermatological causes of pruritus are atopic and contact dermatitis, urticaria, miliaria rubra, infections, insect bites or infestations, xerosis, and aquagenic pruritus. A careful history and physical examination usually reveal the diagnosis.
Pruritus—the most common dermatological complaint—is usually the result of a primary skin disease, but it can be a manifestation of a systemic illness.1 The cause can usually be determined via a good history and physical examination: laboratory investigations are generally not necessary. The underlying cause should be treated whenever possible.
The word pruritus is derived from the Latin prurire, which means “to itch.” Defined as an unpleasant sensation that provokes the desire to scratch,2 pruritus is the most common symptom in dermatology and one of the most challenging problems in clinical practice. Pruritus can interfere with sleep and concentration, and it can be socially embarrassing. Severe itching can be physically incapacitating.
In children, skin disease (rather than systemic illness) is the most common cause of itching. Here we will review the most common dermatological causes of dermatitis, which account for more than 90% of lesions that itch in childhood (Table 1).

PATHOPHYSIOLOGY
The itch sensation is the result of activation of a network of free nerve endings that are situated at the dermal-epidermal junction.3 Itch receptors are activated by mediators that include histamine, kinins, interleukins, proteases, neuropeptides, and prostaglandins.3,4
The itch impulses travel along unmyelinated C fibers, which enter the ipsilateral dorsal horn of the spinal cord.4 The nerve fibers synapse, cross the midline, ascend in the anterolateral spinothalamic tract to the thalamus, and then pass through the internal capsule to the sensory cortex.5 The perception of itch can be modified by psychological factors such as stress, anxiety, excitation, or distraction. Centrally acting mediators,
such as endorphins and serotonin, can participate in the pathogenesis of generalized pruritus.5 Scratching leads to the development of inflammatory mediators, which can aggravate the pruritus and reinforce scratching.
DERMATOLOGICAL CAUSES OF PRURITUS
Atopic dermatitis. This inflammatory skin disorder is characterized by pruritus, erythema, oozing, crusting, scaling, and sometimes lichenification (Figure 1).6 In infants, the cheeks and extensor areas of the arms and legs are typically affected. Involvement of flexural areas usually appears later.

Figure 1. In atopic dermatitis (or atopic eczema), protracted scratching leads to post-inflammatory dyschromia and palpable thickening of affected skin (lichenification). (Courtesy of Ted Rosen, MD.)
Atopic dermatitis affects approximately 3% to 5% of children in North America.7 About 70% of patients have a family history of atopy. Allergic rhinitis or asthma is significantly more likely to develop in children with atopic dermatitis.6
Contact dermatitis. Primary irritant contact dermatitis and allergic contact dermatitis are the 2 types. Primary irritant contact dermatitis is a non-allergic reaction to prolonged or repetitive contact with chemical irritants that are present in such vehicles as saliva, citrus juice, soap, bubble bath, detergent, urine, and feces. Allergic contact dermatitis is a T-cell mediated type IV hypersensitivity reaction. The skin lesion is limited to the site of exposure to the offending allergen. Common allergens include metals, such as nickel (Figure 2); topical medications, such as neomycin and diphenhydramine; and plants, such as poison ivy, oak, and sumac.

Figure 2. This teenaged girl has nickel contact dermatitis. She was given several pieces of jewelry for her birthday and had been wearing a necklace, earrings, and bracelets. She presented with a rash that involved her wrist, ears, and neck. (Courtesy of John W. Harrington, MD.)
Urticaria. This condition is characterized by well-circumscribed, raised, palpable wheals that blanch with pressure and typically resolve within a few hours. The lesions are usually erythematous and intensely pruritic. Urticaria is the result of dilation and increased capillary permeability and leads to edema of the upper corneum. Type I hypersensitivity to food, drugs, inhalants, and insect venoms is the most common mechanism, but type II (transfusion reaction) hypersensitivity or type III (serum sickness) hypersensitivity is also possible. Cold urticaria, solar urticaria, pressure-induced urticaria (dermographism), and exerciseinduced urticaria result from the corresponding physical factors.
Miliaria rubra. Also known as “prickly heat,” this disorder is the result of blockage of the eccrine sweat glands at approximately the granular layer with resultant retention and leakage of sweat into the surrounding dermis (Figure 3).8 Miliaria rubra is characterized by minute papulovesicles with intense erythema. The condition is common in hot and humid environments. The lesions are usually localized to areas of the body covered by clothing or to flexural areas where the skin can become macerated. Areas in which clothing allows pooling of sweat, such as collars and waist bands, are especially common sites. Miliaria rubra never occurs on the palms or soles and is rarely seen on the face.

Figure 3. Known universally as “prickly heat,” miliaria rubra presents as erythematous, minute papules or papulovesicles that may impart a prickling sensation. The rash occurs on the face. (Courtesy of Alexander K. C. Leung, MD.)
Infections. Pruritus is common in some viral infections, such as chickenpox; superficial fungal infections, such as dermatophytosis; and cutaneous bacterial infections, such as hot-tub folliculitis (Figure 4), which is almost always caused by Pseudomonas species.

Figure 4. This young girl has hot-tub folliculitis. The responsible organism, Pseudomonas aeruginosa, survives in hot tubs, especially those made of wood. Those who become infected usually present with a rash that starts within a few hours to a week after the hottub experience.
 Insect bites/infestations. Insect bites, especially by mosquitoes and fleas, are a common cause of pruritis. Papular urticaria—a delayed hypersensitivity reaction to an insect bite—usually occurs in infants and children during the warmer months: the condition presents as intensely pruritic, erythematous, and umbilicated papules that cluster mainly on the trunk and extensor surfaces of the extremities (Figure 5). Tolerance to the presumed etiological antigens found in the inciting insect’s saliva eventually develops spontaneously in children.
Insect bites/infestations. Insect bites, especially by mosquitoes and fleas, are a common cause of pruritis. Papular urticaria—a delayed hypersensitivity reaction to an insect bite—usually occurs in infants and children during the warmer months: the condition presents as intensely pruritic, erythematous, and umbilicated papules that cluster mainly on the trunk and extensor surfaces of the extremities (Figure 5). Tolerance to the presumed etiological antigens found in the inciting insect’s saliva eventually develops spontaneously in children.

Figure 5. This picture of crusted excoriation and indurated, erythematous papules is typical of that seen in younger persons following insect bites. Unlike the familiar short-lived wheals that typically follow mosquito bites, these more palpable and persistent lesions are often referred to as “papular urticaria.” Such lesions represent a high degree of hypersensitivity to insect salivary antigens. Eventually, repeated bites lead to desensitization and this type of reaction ceases. (Courtesy of Ted Rosen, MD.)
Infestation by the mite Sarcoptes scabiei var hominis causes severe pruritus, which is characteristically worse at night. The eruption consists of wheals, papules, vesicles and thread-like burrows (Figure 6). The lesions are found mainly in the interdigital spaces, wrists, axillae, and genitalia. Unlike the presentation in adults, however, mites may be found (and therefore lesions and pruritus occur) on the feet.


Figure 6. This child presented with an extensive, pruritic rash. Eczematous scaly patches were present on the child’s face, scalp, and wrists. The rash resembled atopic eczema. A scraping taken from the wrist revealed Sarcoptes scabiei mites.
Pediculosis capitis, pediculosis corporis, and pediculosis pubis, caused by infestation with head lice (Pediculus humanus capitis), body lice (Pediculus humanus corporis) and pubic lice (Phthirus pubis), respectively, are intensely pruritic. In pediculosis capitis, pediculi are not always visible, but nits can usually be found on the hair shafts (Figure 7).9 Pediculosis corporis is rare in children and occurs primarily in children with poor hygiene. Pediculosis corporis presents as pruritic papules, wheals, and excoriations. Pediculosis pubis is usually transmitted by sexual contact and occurs mainly in adolescents. Nits can usually be found on the hair shaft. Adult lice are only occasionally detected. Small blue-gray macules can be found in the pubic area, abdomen, and thighs.

Figure 7. Approximately 3% of school children are affected with head lice. The louse infests only the human head; it sucks blood and secretes saliva, which results in an inflammatory reaction and itching. Head-to-head contact is the mode of transmission. The eggs laid by the female louse are translucent and attach to the hair shaft or scalp. The eggs hatch in a week, and the nits (which are empty egg shells) remain attached to the shaft. (Courtesy of Kirk Barber, MD.)
Infestation with Enterobius vermicularis (pin worm) is an important cause of perianal pruritus in childhood. The pruritus is typically worse at night or during the early hours of the morning.
 Xerosis. This is the most common cause of itching in the absence of a rash.10 Clinically, the skin is dry and cracked and can be covered with fine scales. Arid climates, frequent bathing, and atopic backgrounds are causative factors. Xerosis as a sole cause of itching is more common in adults, in the Northern hemisphere, and during low humidity winter months.
Xerosis. This is the most common cause of itching in the absence of a rash.10 Clinically, the skin is dry and cracked and can be covered with fine scales. Arid climates, frequent bathing, and atopic backgrounds are causative factors. Xerosis as a sole cause of itching is more common in adults, in the Northern hemisphere, and during low humidity winter months.
Aquagenic pruritus. Itching caused by contact with water usually occurs within 30 minutes of a shower and lasts 10 to 120 minutes.2 There are no objective cutaneous alterations and no associated cutaneous or systemic diseases. This is a very rare condition, but one that may be readily reproducible.
SYSTEMIC CAUSES OF PRURITUS
The causes and pathogenesis of pruritus are the same in children and adults. Systemic disease can be associated with generalized pruritus (Table 2). In adults, the prevalence of a systemic illness as the cause of pruritus ranges from 10% to 50%.11 Systemic illness is presumed to be a less common cause of pruritus in children, but prevalence data are not available.

Chronic renal failure. The prevalence of uremic pruritus ranges from 20% to 30% in adult patients with chronic renal failure.2 Pruritus is less likely to develop in patients who are dialysed with more permeable polysulphone membranes than in those who are dialysed with less permeable and less biocompatible membranes.12 Uremic pruritus has been attributed to xerosis, cutaneous mast cell proliferation, secondary hyperparathyroidism, increased deposition of calciu in dermal tissues, accumulation of an unknown pruritogenic substance, hypervitaminosis A, and peripheral neuropathy.4 In most patients, the itching is likely the result of a combination of these factors.
Hepatobiliary disease. In liver disease, pruritus is a symptom of biliary obstruction, and the association of jaundice and pruritus always signifies biliary obstruction. Pruritus can be associated with intrahepatic or extrahepatic biliary obstruction, drug-induced cholestasis (eg, erythromycin, phenothiazines, oral contraceptives, and anabolic steroids), cholestasis of pregnancy, or primary biliary cirrhosis.13 However, serum and skin bile salt concentrations do not always correlate with the severity of itching.4 A possible explanation is that cholestatic pruritus is caused by an effect of bile salts on the liver and not on the skin. Increased central opioidergic neurotransmission or neuromodulation might be involved in the pathogenesis of cholestatic pruritus.2
Endocrine disorders. The incidence of pruritus in patients with thyrotoxicosis is estimated to be approximately 4% to 11%.13 Various mechanisms have been proposed and include cutaneous vasodilatation, lowered itch threshold, increased kinin activity, and increased sensitivity to catecholamine.4 In hypothyroidism, the pruritus is caused by xerosis.13
Drugs. Pruritus is a common feature of drug eruptions. Certain drugs, such as erythromycin and phenothiazine, can cause choleostatic pruritus (vide supra). Morphine, heroin, and butorphanol cause pruritus by acting on opioid receptors in the CNS.13 Salicylates may trigger or worsen urticaria.
Myeloproliferative disorders.
Approximately 20% to 50% of patients with polycythemia vera experience pruritus, particularly after a hot bath.2 The exact mechanism is not known, but it might be related to elevated serum histamine levels or to iron deficiency.2 Although myeloproliferative disorders are more common in adults, both sporadic and hereditary forms of polycythemia have been described in the pediatric population.
Leukemias of all types, Hodgkin disease, and cutaneous T-cell lymphoma can cause itching.14 The release of histamine from the increased number of circulating basophils, the increased production of histamine from an increase in activity of histidine decarboxylase, and the release of leukopeptidases from abnormal lymphocytes and granulocytes are possible mechanisms for the pruritus.14
Internal malignancy. Pruritus can be a symptom of internal malignancy.14 Itching is usually generalized but can be more pronounced on the shoulders, upper chest, extensor surfaces of the arms, and inner surfaces of the thighs and shins. The intensity and extent of pruritus do not correlate with the extent of malignancy. Pruritogenic neoplasms are much less common in children than in adults.
Psychogenic pruritus. Stress plays an important role in the itching. Pruritus can be a manifestation of an anxiety disorder, obsessive-compulsive disorder, personality disorder, depression, or psychosis.
THE HISTORY
A careful history and thorough physical examination are important in the evaluation of a child with pruritus.
Location. Pruritus restricted to a single anatomical area usually suggests a specific local cause. Pruritus that affects only an exposed area suggests an exogenous cause, such as an insect bite or sunburn. In aquagenic pruritus, the pruritus typically begins on the lower extremities and becomes generalized, sparing of the head, palms, and soles.2 Cholestasisrelated pruritus has a predilection for the hands and feet.4,5 Systemic causes are usually associated with generalized pruritus.
Chronicity. A recent onset suggests
an infection, insect bite, drug reaction, urticaria, or contact dermatitis. Chronic pruritus is more common with atopic dermatitis or a chronic systemic illness.
Time of occurrence. Pruritus is commonly worse at night. This is especially so with scabies. Pruritus from bedbugs and pruritus ani from pinworm infestation usually occur at night. Pruritus that awakens the child at night is usually the consequence of an organic cause, whereas psychogenic pruritus rarely interferes with sleep.2
Character. Pruritus secondary to polycythemia vera is “pricking” in nature.5 Formication (a sensation resembling ants crawling across the skin) suggests an adverse drug effect or psychosis.
Precipitating factors. A pruritic rash that develops following the ingestion of food suggests urticaria or atopic dermatitis. Pruritus that develops after contact with wool suggests atopic dermatitis or contact dermatitis. A history of prolonged contact with saliva, urine, or feces suggests an irritant contact dermatitis. Allergic contact dermatitis is suggested when the pruritic rash is limited to the site of exposure to the allergen, such as nickel with earrings, or a topical medication. Miliaria rubra should be considered when the pruritic rash develops in a hot and humid environment. Pruritus after a hot bath suggests aquagenic pruritus or polycythemia vera.5
Associated symptoms. Anorexia, tiredness, and nausea suggest chronic renal failure. Nervousness, palpitations, weight loss despite an increased appetite, and heat intolerance suggest hyperthyroidism.
Drug use. Medications such as erythromycin, oral contraceptives, and anabolic steroids can cause pruritus. Narcotic analgesics may also trigger histamine release and, therefore, pruritus.
Exposure to infections and infestations.
A history of known exposure to chickenpox, pediculosis, or scabies is important. Occurrence in siblings may suggest a communicable cause of pruritus, such as those mentioned above.
Exposure to pets. A pruritic rash that develops following exposure to a dog or cat suggests atopic dermatitis, flea bite, or infestation with a non-burrowing and nonhuman mite, such as canine scabies, notoedric or feline scabies, or cheyletiella in both types of animals.
Psychosocial history. Any psychosocial stress should be noted as a potential cause or aggravating factor for the pruritus.
Past health. Any previous hospitalization or significant illness should be noted. A history of dermatological disorder, chronic renal failure, hepatobiliary disease, or thyroid disorder suggests the corresponding illness as a cause of the pruritus. With a history of dermatological disorder, the diagnosis, treatment, and result of the treatment should be noted.
Family history. A family history of atopy or thyroid disorder suggests the corresponding disease. Itching in other family members suggests a common exposure, such as insect bite, pediculosis, or scabies.
PHYSICAL EXAMINATION
General. The weight and height should be plotted on standard growth charts. Poor growth suggests a chronic disorder, such as chronic renal failure or hepatic disorder. A polished and beveled appearance to the fingernails indicates that the pruritus is severe and the scratching is chronic. Seams of the patient’s clothing should be examined for body lice if pediculosis corporis is suspected.
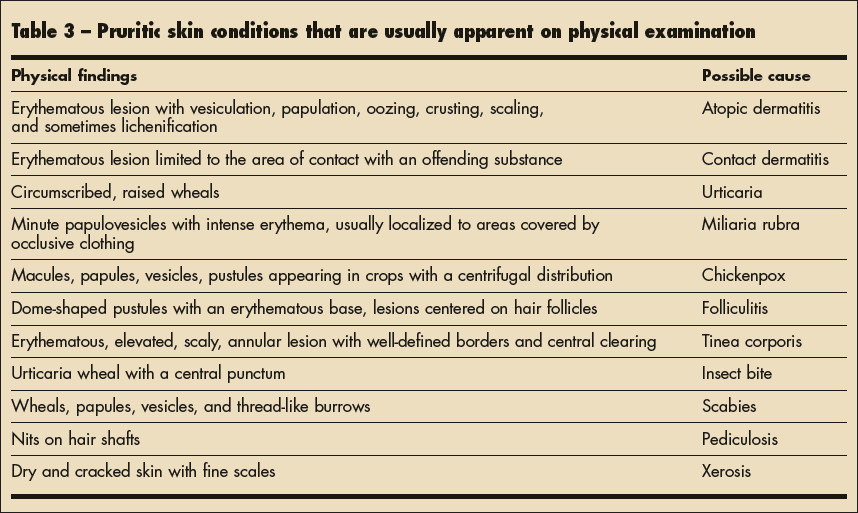
Skin. The skin should be carefully examined for disease as a cause of pruritus (Table 3). Excoriations, secondary infection, post-inflammatory hypopigmentation or hyperpigmentation, lichenification, and scars should be noted. Sparing of the upper mid-back, which the patient cannot reach, is referred to as the “butterfly sign”: it suggests a systemic cause.2,15
Associated signs. The presence of goiter, hand tremor, and exophthalmos suggests hyperthyroidism. Pallor, hypertension, and growth failure suggest chronic renal failure. Jaundice, spider angioma, palmar erythema, hepatosplenomegaly, and ascites suggest a hepatic disorder.
LABORATORY EVALUATION
Laboratory tests are not necessary for most children. Testing is warranted when indicated by the history or physical examination findings. A patch test might be necessary to confirm the diagnosis of allergic contact dermatitis. Microscopic examination of a potassium hydroxide wet mount preparation of infected material should be done when you suspect fungal infection. Consider microscopic examination of a skin scraping placed in mineral oil from burrows or papules if scabies is suspected. Egg of E vermicularis can be detected on adhesive cellophane tape pressed against the perianal area in the early morning. A complete blood count is indicated if a myeloproliferative disorder is considered. Tests of thyroid or renal function are required if the corresponding disorder is suspected. In select cases, a skin biopsy should be considered if the pruritus is persistent and the etiology is obscure. Objective measurements of itch can be made with limb-worn digital accelerometers and infrared video.14 Appropriate radiological imaging or scans may be performed if pediatric malignancy is suspected because of weight loss, localized pain, or other suggestive signs/symptoms.
TREATMENT
Treat the underlying cause whenever possible. Symptomatic treatment for pruritus is essential to break the itch-scratch cycle.
Precipitating or contributing factors need to be avoided. Skin is less itchy in a cool environment. Advise patients to wear comfortable loose clothing, to choose cooler ambient temperatures, and to avoid very hot baths and woolen clothing.1 Excessive bathing can lead to xerosis and is to be avoided. Tell parents to chose a mild and fragrance-free soap, to trim their child’s fingernails to reduce the potential for skin damage from scratching, and to apply a fragrance- free moisturizer when dry skin seems causative or provocative.
Local applications of pramoxine or calamine lotion sooth the skin.13 Additional relief can be obtained by adding low concentrations (one-quarter to one-half percent) menthol and phenol to the topical vehicle.1 Topical application of an antihistamine should be avoided because of the potential for contact sensitization.
Topical application of hydrocortisone or an immunomodulator can be used to treat atopic dermatitis.6 Topical calcineurin inhibitors (TCI), such as tacrolimus ointment or pimecrolimus cream have become standard “step-down” products following initial improvement of atopic dermatitis due to topical corticosteroids. Such compounds are, however, contraindicated in children younger than 2 years of age and for long-term use. The antipruritic effect is the result of anti-inflammatory and immunosuppressive properties. Ultimately, the goal is to transition the pediatric patient to topical management with a nonsteroidal, non-TCI agents, such MimyX or Atopiclair—both of which are moisturizer-based preparations with a modicum of anti-inflammatory effect.
Oral antihistamines are helpful for the symptomatic treatment of pruritus. Of the H1-antihistamines, hydroxyzine is considered to be more effective than diphenhydramine hydrochloride and cyproheptadine.13 The second-generation antihistamines, such as terfenadine, loratadine, and astemizole have fewer CNS effects and are nonsedating. These medications are also less effective, however. Because H2 receptors are not involved in the pathogenesis of itch, H2 antihistamines, such as cimetidine and ranitidine, are not helpful in histamine-induced pruritus. However, the combination of an H1 and H2 antihistamine may be beneficial in severe urticaria. A preliminary study has shown that mirtazapine is effective, especially for patients with nocturnal itch and chronic pruritus.16
REFERENCES
- Weisshaar E, Kucenic MJ, Fleischer AB Jr. Pruritus: a review. Acta Derm Venereol Suppl (Stockh). 2003;213:5-32.
- Twycross R, Greaves MW, Handwerker H, et al. Itch: scratching more than the surface. QJM. 2003; 96:7-26.
- Greaves M. Mediators of pruritus. In: Bolognia JL, Jorizzo JL, Rapini RP, et al, eds. Dermatology. Philadelphia: Mosby; 2003:85-93.
- Etter L, Myers SA. Pruritus in systemic disease: mechanisms and management. Dermatol Clin. 2002; 20:459-472.
- Hiramanek N. Itch: a symptom of occult disease. Aust Fam Physician. 2004;33:495-499.
- Leung AK, Barber KA. Managing childhood atopic dermatitis. Adv Ther. 2003;20:129-137.


