Peer Reviewed
Predicting Survival From In-Hospital CPR
Cardiopulmonary resuscitation (CPR) was developed to treat individuals who have a sudden unexpected cardiac arrest due to a heart attack, drug overdose, hypothermia, drowning accident, or other reversible condition. However, CPR is now widely used to treat arrests in people with severe underlying illnesses and poor overall likelihood of survival. The purpose of this article is to discuss patient and physician attitudes regarding CPR and survival from CPR, and to examine published general and disease-specific survival rates from in-hospital CPR. Through this, we aim to aid physicians in having useful conversations with patients and their families about survival rates from in-hospital CPR.
There are many misconceptions surrounding survivability from CPR, among both physicians and patients. The general public grossly overestimates the effectiveness of CPR, and attitudes about CPR are often shaped by media portrayal. A study reviewing 97 episodes of the television shows “ER,” “Chicago Hope,” and “Rescue 911” in which CPR was depicted revealed that 75% of persons survived the immediate arrest and that 67% survived to hospital discharge.1 In another study of patients age 70 years and older, 81% believed that their chance of surviving inpatient CPR and leaving the hospital was 50% or better, and 23% believed that their chance was 90% or better.2
Conversely, studies have shown much lower CPR survival rates. A meta-analysis of studies examining the rates of survival from in-hospital CPR found an overall immediate survival rate of 40.7% and a survival to hospital discharge rate of 13.4%.3 More recently, a Canadian study of 247 hospitalized patients who underwent cardiac arrest found that only 22.4% of those with witnessed arrests survived to hospital discharge, and that only 1% of those with unwitnessed arrests survived CPR to hospital discharge.4
Physicians also are poor at predicting survival from CPR. In a 1996 study, 51 attending physicians and residents in internal medicine and family practice were given one-page summaries of admission data for patients who underwent in-hospital CPR. The physicians were then asked to predict survival to stabilization and survival to discharge. The results showed that physicians were no better at identifying patients who would survive resuscitation than would be expected by chance alone.5 In addition, there appears to be little consensus among physicians on the definition of futile treatment as it pertains to CPR survivability. Curtis et al6 conducted a study of second- and third-year residents who applied the futility rationale and found that the definition of futility varied widely among resident physicians.
When examining survival from CPR, it is crucial to assess not only the immediate success of a CPR attempt, but also survival of the patient to hospital discharge. Simply surviving a CPR attempt does not necessarily translate into the patient surviving until discharge. This point was emphasized in a 1988 retrospective review by Taffet and colleagues,7 which showed that survival to discharge is a meaningful marker for CPR survivability, particularly in elderly patients. Authors found that of the 77 CPR efforts in patients age 70 years or older who had arrests, 31% were successful, and 92% of these initial survivors were alive after 24 hours. However, none of these patients survived to hospital discharge.7 In addition, CPR can be a particularly stressful event to endure, with patients possibly sustaining rib fractures and undergoing intubation and mechanical ventilation. For the families of patients who do not survive, they are subjected to watching their loved ones go through what some may consider an “undignified” and an uncomfortable, rather than a “natural,” death.
Factors That Influence CPR Survivability
 Several studies have looked at survival from in-hospital CPR, and results vary depending on patient type, underlying conditions, and setting. Factors that have been found to influence the likelihood of CPR survival include sepsis, cancer, dementia, increased age, azotemia, stroke, and congestive heart failure. Physicians would benefit greatly from the regular use of tools that accurately predict the likelihood of CPR survival based on these factors. One such tool is the Pre-Arrest Morbidity (PAM) index (Table I), which was initially proposed by George et al8 in 1989 to help identify hospitalized patients who have little chance of surviving CPR. The PAM index uses 15 clinical characteristics to evaluate pre-arrest morbidity and predict CPR survivability. The calculated PAM score is inversely related to the likelihood of short-term and long-term survival from CPR, and in the George study, no patient with a score greater than 8 survived to discharge.8 Patients with a PAM score of 7 or greater had a less than 15% chance of long-term survival following CPR.
Several studies have looked at survival from in-hospital CPR, and results vary depending on patient type, underlying conditions, and setting. Factors that have been found to influence the likelihood of CPR survival include sepsis, cancer, dementia, increased age, azotemia, stroke, and congestive heart failure. Physicians would benefit greatly from the regular use of tools that accurately predict the likelihood of CPR survival based on these factors. One such tool is the Pre-Arrest Morbidity (PAM) index (Table I), which was initially proposed by George et al8 in 1989 to help identify hospitalized patients who have little chance of surviving CPR. The PAM index uses 15 clinical characteristics to evaluate pre-arrest morbidity and predict CPR survivability. The calculated PAM score is inversely related to the likelihood of short-term and long-term survival from CPR, and in the George study, no patient with a score greater than 8 survived to discharge.8 Patients with a PAM score of 7 or greater had a less than 15% chance of long-term survival following CPR.
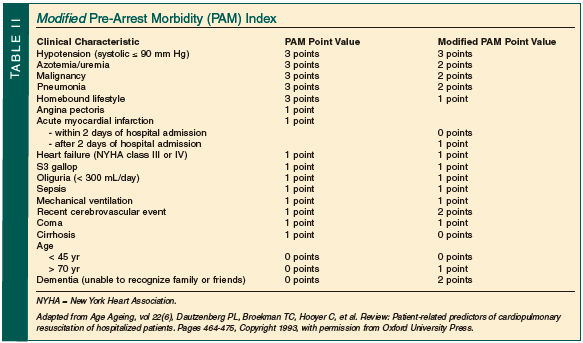
It is important to note that the PAM index proposed by George et al was based on a single study of 140 patients in one institution. Because of this, questions have been raised about its generalizability. Other studies have helped to validate the PAM score as a useful tool. A meta-analysis by Cohn and colleagues9 reviewing 21 studies from 1965-1989 found that the strongest negative predictors of survival from CPR were renal failure, cancer, and age greater than 60 years. On the other hand, the presence of acute myocardial infarction (MI) strongly correlated positively with survival, supporting the observation that CPR was initially designed to be used in people with electrical cardiac abnormalities. Based on their results, Cohn et al concluded that the PAM index is a useful method of stratifying probability of survival from CPR, particularly when applied to patients with high PAM scores, who have very little chance of survival. It was noted that the PAM index does not take into account factors that positively correlate with survival, such as acute MI. Dautzenberg et al10 proposed a modified PAM index (Table II) based on a systematic review of 32 studies evaluating the utility of patient-related factors in predicting the effectiveness of CPR. While this review found that the PAM index was superior to single factors in predicting survival, the modified PAM index was found to best predict survival in the studies reviewed. The modified PAM index score, like the original PAM index score, correlates linearly and inversely with CPR success.
While further studies with larger empirical data are needed to support the PAM and the modified PAM index, we advocate their use by physicians as tools to assist in predicting likelihood of CPR survival to hospital discharge. Of course, these indices must be used in conjunction with clinical judgment and experience, taking each patient’s specific circumstance into account.
Cancer and dementia are two common causes of morbidity and mortality in the elderly that are worth examining in more detail. An analysis of 42 studies from 1966-2005 comprising 1707 patients with localized or metastatic malignant disease showed that survival to hospital discharge in patients with localized disease was 9.5%, comparable to the 10.1% survival rate in unselected patients in general medical/surgical wards. However, survival to discharge in patients with metastatic disease was only 5.6%.11 Subgroup analysis of more recent studies (since 1990) in this meta-analysis did show slightly better survival rates in patients with metastatic disease. This might be due to the more judicious use of codes in the most ill. Nevertheless, one can conclude from this meta-analysis that the presence of metastatic cancer, especially with a high PAM index, makes survival to hospital discharge unlikely.
Among patients with dementia, many of whom reside in long-term care facilities, survival from CPR to hospital discharge is estimated to be three times less likely than in patients without dementia.3 In particular, among resuscitated nursing home residents (with and without dementia), studies have found that the immediate survival rate from CPR is between 10% and 40%, with less than 3% on average (5 studies with survival rates of 3% or less, 1 with a rate of 5%, and 1 with a rate of 10.5%) subsequently discharged from the hospital alive.12 If we consider the decreased success rate of CPR observed in patients with dementia, along with the decreased success rate in the nursing home population as a whole, it is probable that less than 3% of residents in long-term care institutions with dementia undergoing CPR can be expected to survive to hospital discharge. For severe dementia, likelihood of survival is likely even less.
Lastly, it is important to examine whether providing patients with information about survivability actually influences their decision about whether or not to pursue CPR. Murphy et al13 surveyed 371 patients over the age of 60 years about their wishes to undergo CPR in case of cardiac arrest. Although 41% opted to undergo CPR before learning the actual probability of surviving it, only 22% opted for CPR after learning the probability of survival. An even smaller percentage (6%) of those surveyed over the age of 86 years opted for CPR when informed about the likelihood of survival. These results support the belief that informing patients about their chances of surviving CPR does alter patient decision-making as to whether to opt for CPR in case of cardiac arrest.
Summary
As with other medical therapies, it is helpful for clinicians to provide patients with evidence-based predictions on the likelihood of CPR survivability when possible. While serious medical conditions such as cancer, even when metastatic, do not appear to lead to zero survival to discharge after an in-hospital resuscitation episode, survival in these cases is low enough that many patients with serious chronic conditions may choose to forgo CPR if provided with data on CPR survivability. Using tools like the PAM index and the modified PAM index can help physicians provide patients and their families with meaningful and accurate information on their likelihood of surviving CPR to hospital discharge, and thus may allow some patients to forego an intervention that is likely to be futile and harmful to their dignity and quality of life.
The authors report no relevant financial relationships.
Dr. Alabi is a Primary Care Physician and Geriatrician, North Shore Physicians Group, Salem, MA; and Dr. Haines is an Instructor, Department of Family & Community Medicine, Thomas Jefferson University Hospital, Philadelphia, PA.


