Potential Adverse Effects of Proton Pump Inhibitors in the Elderly
Introduction
Since the introduction of omeprazole in 1989, proton pump inhibitors (PPIs) have become one of the most commonly prescribed classes of medications in the world. In 2007, PPI sales in the United States were in excess of $11 billion.1 Esomeprazole and lansoprazole both ranked among the top five drugs sold in the United States in 2007.1
Overall, with their high safety profile and demonstrated efficacy, PPIs represent a major advance in the treatment of acid-related disorders ranging from peptic ulcer disease to erosive esophagitis. However, it has been shown that PPIs are often misused and overused, which may have significant implications.2-7 With the widespread and frequent long-term use of PPIs, several adverse effects have come to light that may call for more selective prescribing practices, particularly in older adults who may be more vulnerable and likely to suffer the consequences of such adverse effects. With an estimated 8% of males and 15% of females age 65 years and older experiencing reflux and potentially using acid-suppressive therapy, 8 understanding the risks for potential adverse effects associated with PPIs is critical in this population.
In this article, we review the current data on selected negative outcomes that may result from PPI use. Specifically, increasing evidence demonstrates that PPI therapy may be associated with the development of Clostridium difficile infections, hip fractures, community-acquired pneumonia, vitamin B12 deficiency, and possibly immunoglobulin E–mediated allergic reactions. The implications of such adverse outcomes, along with the evidence of the inappropriate use of PPIs, underscore the need for more judicious use of this class of medications.
Pathophysiology
PPIs achieve acid suppression by binding to a specific enzyme on the parietal cell, known as the proton pump, resulting in inhibition of gastric acid secretion by the proton pump.9 PPIs are generally well tolerated. The overall incidence of side effects is similar to placebo, which is less than 5%.10 The most common side effects reported are headache, diarrhea, abdominal pain, and nausea. The etiology of these side effects, particularly diarrhea, may be related to alterations in gut flora caused by acid suppression.10 The only contraindication to the use of PPIs is a known history of hypersensitivity to this class of medications. PPIs do not require dosage adjustment in renal or hepatic dysfunction.
Indications and Approved Uses
PPIs are accepted for the treatment and remission maintenance of acute gastric and duodenal ulcers, symptomatic gastroesophageal reflux disease (GERD), erosive esophagitis, pathological hypersecretory conditions such as Zollinger-Ellison syndrome, nonsteroidal anti-inflammatory drug–induced gastric ulcers, and eradication of Helicobacter pylori (Table I).10-13
In 2008, the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents published recommendations regarding the utilization of PPIs to decrease the risk of upper-gastrointestinal (GI) events associated with antiplatelet therapy for primary or secondary treatment of cardiovascular disease.14 The recommendations suggest that PPIs should be used in the following clinical situations in order to reduce risks of GI bleeding: when patients are taking aspirin or clopidogrel and have a history of an ulcer (either bleeding or nonbleeding); or when patients are taking dual antiplatelet therapy or concomitant anticoagulation therapy.14

Overuse/Misuse
While it is clear that PPI therapy can be beneficial when used appropriately in the treatment of various GI disorders, evidence suggests that PPIs are often overused and misused.2-7 In many cases, PPIs are initiated or continued for prolonged periods of time, without sufficient evaluation of the need for therapy. In fact, Manoharan et al15 showed that in more than half of elderly inpatients who were prescribed acid-suppression therapy upon hospital discharge, there was no clearly documented indication for such therapy. Another study by Nardino and colleagues4 showed that 65% of medical inpatients who were prescribed PPIs did not have an approved indication for use. Yet another study conducted at a major Australian teaching hospital showed that 63% of medical inpatients were receiving PPIs for unapproved indications. 3 Common examples of unapproved utilizations of PPIs, which lack evidence to support their practice, involve treatment of low-risk inpatients as a means of prophylaxis against “stress” ulcers and concurrent administration with corticosteroids to prevent peptic ulcer disease in noncritically ill inpatients.2-7
Drug Interactions and Polypharmacy
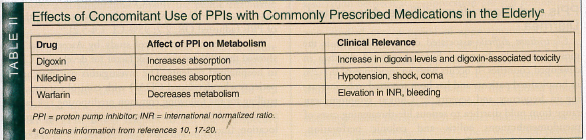
Polypharmacy, defined as the use of multiple medications and/or the administration of multiple medications that are not clinically indicated, 16 is a common and potentially problematic occurrence in the elderly. One consequence of polypharmacy is drug interaction. This is an important consequence to consider when initiating PPIs since they can affect the absorption and metabolism of several medications commonly prescribed in the elderly, such as digoxin, nifedipine, and warfarin.10 By altering gastric pH, PPIs can affect the bioavailability of different medications. 17 In addition, PPIs are metabolized by the hepatic cytochrome P450 system and thereby can affect the metabolism of medications also using this system (Table II). Omeprazole possesses the greatest potential for altering the P450 system. For instance, studies have shown that the initiation of omeprazole can increase the absorption of digoxin, resulting in toxic digoxin levels,18,19 and can decrease the metabolism of warfarin,17 resulting in an increased international normalized ratio (INR) and bleeding.20
In January 2009, the Food and Drug Administration released an early communication about the potential interactions between omeprazole and clopidogrel.21 The concern that omeprazole may lower the efficacy of clopidogrel remains controversial and unsubstantiated given that available studies show conflicting results.22-25 However, a recent large, retrospective cohort study by Ho et al26 found that patients taking a PPI and clopidogrel post–acute coronary syndrome have a modest increased risk of death or rehospitalization as compared to those patients taking clopidogrel alone (odds ratio [OR], 1.25; 95% confidence interval [CI], 1.11-1.4). The results of this study suggest that the risks and benefits of PPI therapy in patients taking clopidogrel should be carefully considered. Further research studies released in 2010 continue to show conflicting results.27,28 Overall, there are strong pharmacodynamic data suggesting that an interaction exists between clopidogrel and PPIs; however, the clinical significance of this interaction is still the subject of continued debate and ongoing research.
Overall recommendations would suggest caution in prescribing PPI therapy to patients who also take clopidogrel, but acid suppression should not be withheld if there is a clear indication for its use. Clinicians should also be mindful that in the elderly, PPI use with digoxin, nifedipine, and warfarin can potentiate digoxin toxicity, hypotension, and increased INR, respectively (Table II).
PPIs and Clostridium difficile–Associated Diarrhea
Clostridium difficile–associated diarrhea (CDAD) is the most commonly diagnosed hospital-acquired diarrhea in developed countries. It occurs with an incidence of 0.1-2% in hospitalized patients and has been reported to be increasing in frequency and severity.29,30 Clinical symptoms can range from mild diarrhea to serious life-threatening cases of pseudomembranous colitis and colonic perforation. Established risk factors for CDAD include antibiotic therapy, advanced age, significant comorbidity, chemotherapy or other immunosuppressants, GI procedures and surgery, stay in an Intensive Care Unit, residence in a nursing home, and prolonged hospitalization.29,30 More recently, it has been proposed that acid-suppressive therapy is also a risk factor for CDAD. Gastric acid has a protective role in the defense against ingested bacteria, and thus, decreasing acid would lead to diminished defense mechanisms against foreign invaders.29,30 Decreased gastric acidity is a known risk factor for other causes of infectious diarrhea, including salmonella and cholera.29,30 Having a higher gastric pH, such as the pH achieved with PPI use, may facilitate colonization by C. difficile with subsequent toxin production and toxin-mediated intestinal injury and inflammation.29
Multiple studies have examined the possible role of PPI use in the development of CDAD. Although conflicting data exist involving this potential relationship, there is enough evidence to warrant concern about the possible role of PPIs in patients at risk for CDAD.29-35 In a prospective case-control study of 155 consecutive inpatients with CDAD, it was shown that CDAD was independently associated with acid-suppression therapy (OR, 1.90; 95% CI, 1.10-3.29).30 Although CDAD was more strongly associated with antibiotic use (OR, 13.1; 95% CI, 6.6-26.1), the results suggest that the risk of CDAD in hospitalized patients receiving antibiotics may be compounded by exposure to PPI therapy.30
In 2004, Dial and colleagues31 conducted a cohort study involving 1187 inpatients who received antibiotics. Within this cohort, patients who had also received a PPI or H2 blocker were compared to patients who had not received any form of acid-suppressive therapy. Overall, 81 (6.8%) of the 1187 inpatients developed CDAD. CDAD was significantly associated with use of PPIs (adjusted OR, 2.1; 95% CI, 1.2-3.5).31 The investigators also included a case-control study during the same time period in order to control for other confounding factors that could not be addressed in the cohort study. In this case-control study, cases were identified as patients with a history of diarrhea and a positive C. difficile toxin assay. Controls were chosen from a list of patients who had been prescribed antibiotics while in the hospital during this same study period. Control subjects were matched to cases by inpatient ward, age, class of antibiotics, and, when possible, number of antibiotics. Overall, it was found that CDAD was significantly associated with the use of PPIs (adjusted OR, 2.7; 95% CI, 1.4-5.2).31
A more recent case-control study by Aseeri et al29 also showed that PPI use was a risk factor for developing CDAD in hospitalized patients. The investigators pair-matched 94 patients who developed CDAD with control patients, controlling for the following common predisposing risk factors: admission date; antibiotic exposure; gender; age; patient location (medical vs surgical unit); and room type. The investigators reported that patients with CDAD were significantly more likely than controls to receive acid-suppressive therapy during hospitalization: 76.6% versus 42.6%, respectively (P = 0.030). Multivariate analysis showed that CDAD was associated with the use of PPIs with an OR of 3.6 (95% CI, 1.7-8.3; P < 0.001). 29
Finally, a recent cohort study conducted by Howell and colleagues36 looked at the intensity of acid-suppression therapy in relation to the risk of nosocomial CDAD. This study involved analysis of data collected on over 100,000 discharged patients from a tertiary medical center over a five-year period. The risk of nosocomial CDAD was examined in four different groups, including those receiving no acid suppression, histamine2-receptor antagonist (H2RA) therapy, daily PPI therapy, and PPI therapy more frequently than daily. They found that as the level of acid suppression increased, the relative risk of nosocomial CDAD increased, from 1 (no acid suppression) to 1.53 (95% CI, 1.12-2.10; H2RA), to 1.74 (95% CI, 1.39-2.18; daily PPI), and to 2.36 (95% CI, 1.79-3.11; more frequent than daily PPI).36 Their results suggest that increasing levels of pharmacologic acid suppression are associated with increased risks of nosocomial CDAD.36
Overall, the data suggest an appreciable association (OR ranging from 1.90 to 3.6) between PPI use with development of CDAD.
Continued on next page
PPIs and Food Allergies
In addition to their relation to CDAD, PPIs may also play a role in promoting increased allergic reactivity in patients on acid-suppressive therapy.37 Rising food allergen formation possibly associated with PPIs may result in escalating rates of severe allergic reactions such as anaphylaxis and lead to significant restrictions in diet. Untersmayr et al37 investigated the potential role of PPIs in promoting immunoglobulin E (IgE)–mediated food allergies. Based on their animal experiments, it was hypothesized that food proteins may cause increased allergenicity if they survive through the normally acidic contents of the stomach.
This mechanism of increased IgE reactivity can be understood by realizing that acid-suppressive therapy raises gastric pH to around 5.0. It is known that the optimum pH of pepsins in the stomach is between 1.8 and 3.2. Therefore, acid suppression impairs the peptic enzymatic digestion of proteins.38 When food proteins are not degraded in the stomach, they retain their protein structure. It has been speculated that this preserved food protein structure is a prerequisite for the development of IgE antibodies to the food.38
An observational cohort study was performed with 152 patients who were starting treatment with H2 receptor blockers or PPIs. Blood samples to test for IgE-specific antibodies to 19 specific foods were drawn before and after 3 months of acid-suppressive therapy. Investigators found that 25% of patients who were on acid-suppressive therapy for a period of 3 months formed new IgE antibodies toward food antigens. Fifty control patients who were not treated with acid-suppressive therapy were recruited in order to exclude a nonspecific boost in IgE reactivity during the pollen season. The control subjects showed no change in their IgE patterns during the course of the study. Of the 25% of patients on acid-suppressive therapy who formed new IgE antibodies, 10% had a boost of pre-existing food-specific IgE, and 15% had new IgE formation. As compared to 50 age-matched healthy controls, the relative risk of developing the increase of an IgE food allergen response after 3 months of acid-suppressive therapy was 10.5 (95% CI, 1.44-76.48; P = 0.0203).37 Five months after discontinuation of the H2 blocker or PPI, serum IgE reactivity decreased but was still present in 6% of patients.37 To determine the in vivo relevance of these results, skin prick testing was done. After 8 months (including 3 mo of acid-suppressive therapy and subsequent 5 mo after discontinuation of therapy), 33 patients with elevated serum, allergen-specific IgE antibodies underwent skin prick testing with the 19 food extracts. The percentage of positive skin reactions was higher in exposed patients versus controls (7.02% of patients vs 1.00% of controls had positive skin reactions).
Overall, the relationship between PPI therapy and the development of IgE food allergens remains unclear but may be significant. More studies in this area are needed to clarify this potential association, and whether there are meaningful clinical implications.
PPIs and Community-Acquired Pneumonia
H2RAs and PPIs create a hypochlorhydric to achlorhydric environment in the gut, thereby facilitating survival of certain ingested pathogens that would otherwise be killed by unaltered pH gastric juices. Regurgitation of ingested bacteria into the oropharynx can precipitate respiratory infections.
In 2004, Laheij and colleagues39 published a prospective cohort study with a nested case-control analysis of a national health database in the Netherlands to examine the association between acid-suppression use and community-acquired pneumonia (CAP). Of the 364,683 adults who were studied over a period of approximately 2.7 years, 19,459 were considered exposed, defined as receiving a first prescription for an acid-suppressive agent. It was reported that 10,177 received H2RAs and 12,337 received PPIs, while 3055 individuals used both. In the exposed group, 477 individuals developed pneumonia, either while taking acid-suppressive therapy (185) or after discontinuation of the acid-suppressive agent (292). There were 5366 persons with pneumonia in the nonexposed group. The relative risk for patients taking an acid suppressant developing CAP was 1.6 as compared to those patients not taking an acid suppressant. Pneumonia was confirmed by chest x-ray, sputum culture, or clinical symptoms. To reduce confounding by indication, a nested case-control analysis was conducted among the 477 adults who developed pneumonia during or after discontinuation of the acid-suppressive medication. Four hundred seventy-five of those patients were matched to 4690 controls for sex, age, and index date of pneumonia. Acid-suppressive use was defined as current if the prescription included the index date of pneumonia, and was defined as past if the end of the last prescription was before the index date. Past was further broken down into recent past if the end of the last prescription was less than 30 days, past if between 30 and 180 days ago, and distant past if more than 180 days ago. Laheij et al39 pointed out that as compared to the controls, the patients with pneumonia more often had comorbid conditions such as diabetes mellitus, heart failure, and pulmonary disease, as well as antibiotic usage. After adjustment of confounders such as medical comorbidities and use of antibiotics, it was found that current use of a PPI or a H2RA was associated with a small increase in risk of CAP (adjusted OR, 1.27; 95% CI, 1.06-1.54). Within this group, the risk of CAP appeared most pronounced among patients who began an acid suppressant within the last 30 days (adjusted OR, 2.12; 95% CI, 1.29-3.48). Researchers also found a positive association between increased defined daily dose (DDD) of a PPI and CAP: more than one DDD yielded an adjusted OR of 2.28 (95% CI, 1.26-4.10).
In 2007, Gulmez and colleagues40 published a population-based, case-control study of patients in Denmark. They studied 7642 patients with a discharge diagnosis of CAP. CAP was confirmed by x-ray, culture, and polymerase chain reaction test. Current use of a PPI was defined as use in the past 90 days prior to CAP diagnosis, and past use was defined as greater than 90 days. Patients with CAP who were currently taking a PPI had a moderately increased risk of CAP (OR, 1.5; 95% CI, 1.3-1.7). The risk was most profound in users who started a PPI within 0-7 days (OR, 5.0; 95% CI, 2.1-11.7). Unlike Laheij et al,39 Gulmez et al did not see an increased risk of CAP among H2RA users or in those taking increased daily doses of PPIs. They did not find an association with recent past use (last prescription 90-180 days before CAP index date) or distant past use (> 180 days before CAP index date) of acid-suppressive agents.
In 2008, Sarkar and colleagues41 published a large (case patients, n = 80,066; control participants, n = 799,881), nested case-control study of a United Kingdom database to examine the association between PPI use and CAP. Overall, they found that patients who began a PPI within the past 30 days had an increased risk for CAP. This risk increased dramatically in patients who began a PPI less than 2 weeks prior to CAP diagnosis. Specifically, initiation of PPI 2, 7, and 14 days prior to diagnosis yielded an OR of 6.53 (95% CI, 3.95-10.80), of 3.79 (95% CI, 2.66-5.42), and of 3.21 (95% CI, 2.46-4.18), respectively. Patients with longer-term, current use of a PPI did not have an increased risk for CAP.
PPIs take approximately seven days to yield maximum acid-suppressive effect.41 It is hypothesized that aspiration of pathogens into the hypochlorhydric to achlorhydric environment in the gut can predispose a patient to CAP. As Sarkar et al41 noted, intuitively, one would predict that those patients who have been taking PPIs chronically would be the most at risk of developing CAP. However, these three studies failed to support this hypothesis.39-41 In contrast, the results of these studies suggest that an increased risk of CAP is associated with initiation and recent use of an acid-suppressive agent.
Herzig and colleagues42 recently published the first prospective study examining the relationship between acid-suppressive agents and hospital-acquired pneumonia (HAP) in nonventilated patients. There were 63,878 admissions eligible for the study. Of the 52% prescribed an acid-suppressive medication, 83% received a PPI and 23% received a H2RA. The adjusted OR of HAP in those receiving a PPI after adjustment of age and comorbidities was 1.3 (95% CI, 1.1-1.4). The adjusted OR of HAP in those receiving a H2RA was 1.2 (95% CI, 0.98-1.14). The authors found that the association between acid-suppressive agents and HAP was only statistically significant for PPI use.
Overall, studies suggest that there is a modestly increased risk of developing CAP related to current or recent use of PPIs. However, some feel that the association of PPIs with CAP may result from the confounding presence of the underlying condition, namely GERD, and not PPI use itself.13,43,44 Perhaps those patients with more severe reflux are at higher risk for aspiration and subsequent CAP regardless of their use of an acid-suppressive agent.44 Further studies are needed to elucidate the nature of the relationship between the occurrence of CAP and PPI therapy.
PPIs and Hip Fractures
Recent studies have demonstrated an association between long-term PPI use and hip fractures in the elderly.45-48 It has been proposed that an acidic environment facilitates calcium absorption in the gut49; therefore, PPIs can decrease calcium absorption. PPIs can also interfere with bone metabolism by weakly inhibiting proton transport within osteoclasts, and possibly suppressing osteoclast activity.49
In 2006, Yang et al45 published a large, nested case-control study of patients from a United Kingdom database focusing on patients age 50 years and older who took a PPI for at least 1 year. They found a positive association between increasing duration and daily dosages of PPI and hip fracture. One year of PPI use had an adjusted OR of 1.44 (95% CI, 1.26-1.54), and 4 years of PPI use had an adjusted OR of 1.59 (95% CI, 1.39-1.80). PPI use of greater than 1 daily dose had an adjusted OR of 2.65 (95% CI, 1.80-3.90).
The same year, Vestergaard and colleagues46 published a large case-control study performed in Denmark and found an increased risk of any fracture in patients using a PPI within 1 year. The OR of hip fracture with 1 year of PPI use was 1.60 (95% CI, 1.25-2.04). However, they were unable to confirm Yang et al’s finding of increased hip fracture risk with increasing daily doses of PPI.
A more recent study published in 2008 by Targownick et al47 analyzing a Canadian database found that PPI use of 5 or more years was modestly associated with increased risk of hip fracture (adjusted OR, 1.62; 95% CI, 1.02-2.58).
In 2010, Gray and colleagues50 published results from a prospective analysis of postmenopausal women enrolled in the Women’s Health Initiative Observational Study and Clinical Trials taking a PPI or a H2RA for less than 1 year, 1-3 years, or greater than 3 years. The study did not show an increased risk in hip fractures in the 3396 women who were taking a PPI for any of the above lengths of time (hazard ratio [HR], 1.00; 95% CI, 0.71-1.40). Unlike the previous studies, 45-47 Gray et al50 did not find a positive correlation between longer duration of PPI use and increased hip fracture risk; however, the authors noted that they had fewer women (392) taking a PPI for more than 3 years. The study did find an increased risk of spine fractures (HR, 1.25; 95% CI, 1.15-13.6), forearm or wrist fractures (HR, 1.26; 95% CI, 1.05-1.51), and total fractures (HR, 1.25; 95% CI, 1.15-1.36) in women using a PPI.
Based on these aforementioned studies, the evidence suggesting the association of PPI use with increased risk of hip fracture is modest at best and remains unclear. The specific risks related to the duration and dose of PPIs also need to be studied further. The correlation of PPIs with hip fractures may result from confounding factors that were not adequately controlled. For instance, critiques of Yang et al’s study point out that the patients with hip fractures were more likely than their controls to have used medications such as antiseizure agents, antipsychotics, anxiolytics, and antidepressants, many of which have also been linked with higher risks for falls, osteoporosis, and hip fracture.51 While the relationship between hip fractures and PPIs deserves serious consideration, more definitive studies are still needed to significantly impact prescribing practice.
PPIs and Vitamin B12 Deficiency
Another proposed adverse effect of long-term PPI use is cobalamin malabsorption. Several mechanisms have been proposed by which PPI use may lead to cobalamin malabsorption. First, a more basic gastric environment may slow the release of cobalamin from dietary food sources.49 Another potential mechanism involves the risk of bacterial overgrowth that can result from PPI use. The excess bacteria in the small intestine may consume cobalamin before it can be absorbed.49,52 Yet another mechanism of decreased cobalamin absorption involves the theoretical possibility that PPIs could reduce intrinsic factor secretion by inhibiting parietal cell proton pumps; however, this has not been found to occur in actual practice.53 Overall, studies have shown that acid suppression may decrease vitamin B12 absorption, and with long-term use, may result in reductions in serum B12 levels.49,54 However, questions still remain regarding whether patients may develop clinical vitamin B12 deficiency as opposed to simply exhibiting reductions in serum levels that are still within the normal range.49,54 A particularly vulnerable population would be older adults, who are already at risk for cobalamin deficiency. Vitamin B12 deficiency can have significant consequences such as the development of dementia or neuropathy. Such conditions may not fully reverse, even with repletion.9
With regard to the geriatric population, adults over the age of 65 years are estimated to have a 5-15% prevalence of B12 deficiency.9 The etiology for B12 deficiency in older adults is thought to be related to malabsorption of dietary B12. This malabsorption may be from atrophic gastritis, age-related hypochlorhydria, or other conditions such as H. pylori infection. 9 It can take months to years for a B12 deficiency to manifest secondary to malabsorption because liver stores of B12 can compensate for decreased dietary intake.9
Valuck et al9 examined the relation of acid suppression and B12 deficiency by conducting a case-control study with patients in a geriatric primary care setting. They enrolled patients age 65 years and older who had documentation that a serum B12 laboratory assessment had already been completed. They compared 53 vitamin B12–deficient cases with 212 controls for past or current use of acid-suppression therapy based on subjects’ medical records. The following variables were controlled for: age; gender; multivitamin use; and H. pylori infection. Overall, researchers found that current use of acid-suppression therapy for at least 12 months was associated with a significantly increased risk of vitamin B12 deficiency (OR, 4.45; 95% CI, 1.47-13.34).9 However, they did not find an association between short-term current use or past use of acid suppression and B12 deficiency.
Another study looked at the potential association between chronic acid suppression and the initiation of B12 supplementation. Force and colleagues55 conducted a retrospective case-control study, in which 125 cases were identified as those patients who initiated vitamin B12 supplementation during the defined study period. The 125 cases were matched to 500 controls. The cases were then compared to the controls with regard to exposure to chronic acid-suppression therapy (defined as treatment with H2 blocker or PPI use for > 10 mo of the 12 mo that preceded initiation of B12 supplementation).55 Overall, 23 cases (18.4%) were found to have used chronic acid-suppression therapy as compared to 55 (11.0%) of the control group. Patients who initiated B12 supplementation were more likely than controls to have received chronic acid-suppression therapy (P = 0.025; OR, 1.82; 95% CI, 1.08-3.09).55
Overall, data suggest that while it would be extremely costly and possibly unnecessary to monitor B12 levels in all patients taking acid-suppression therapy, it may be prudent to monitor levels in patients who are chronically taking acid-suppressive therapy or in those already at higher risk for B12 deficiency, such as the elderly or those with dementia.9

Conclusion
Understanding the possible harms of commonly prescribed medications such as PPIs becomes paramount, particularly in the elderly, where issues such as polypharmacy and medication adverse effects and interactions are commonly encountered. PPI use is clearly indicated for certain conditions such as active peptic ulcer disease or stress ulcer prophylaxis in high-risk patients. However, when these conditions are not present, discontinuation of PPIs should be considered.4,29 While it is clear that PPI therapy is beneficial when used appropriately in the treatment of various GI disorders, growing evidence suggests that PPI therapy may be associated with several adverse outcomes, including C. difficile infections, CAP, hip fractures, B12 deficiency, and possibly IgE-mediated allergic reactions (Table III). Such associations appear modest, yet data are limited by study size and/or design. Further studies are needed to explore the true relationship of PPIs to these outcomes.
The authors report no relevant financial relationships.
Dr. Kapadia is a Family Medicine Physician, Grand Junction VA Medical Center, Grand Junction, CO; Dr. Wynn is a Family Medicine Physician, Community Health Center of Meriden, Meriden, CT; and Dr. Salzman is Assistant Professor, Department of Family and Community Medicine, Division of Geriatric Medicine, Thomas Jefferson University Hospital, Philadelphia, PA.
References
1. Top 200 generic drugs by retail dollars in 2007. Accessed June 21, 2010.
2. Mat Saad AZ, Collins N, Lobo MM, O’Connor HJ. Proton pump inhibitors: A survey of prescribing in an Irish general hospital. Int J Clin Pract 2005;59:31-34.
3. Naunton M, Peterson GM, Bleasel MD. Overuse of proton pump inhibitors. J Clin Pharm Ther 2000;25:333-340.
4. Nardino RJ, Vender RJ, Herbert PN. Overuse of acid-suppressive therapy in hospitalized patients. Am J Gastroenterol 2000;95:3118-3122.
5. Parente F, Cucino C, Gallus S, et al. Hospital use of acid-suppressive medications and its fall-out on prescribing in general practice: A 1-month survey. Aliment Pharamacol Ther 2003;17:1503-1506.
6. Walker NM, McDonald J. An evaluation of the use of proton pump inhibitors. Pharm World Sci 2001;23:116-117.
7. Pohland CJ, Scavnicky SA, Lasky SS, Good CB. Lansoprazole overutilization: Methods for step-down therapy. Am J Manag Care 2003;9:353-358.
8. Shams D, Siddiqui NH, Heif, MM. Gastroesophageal reflux disease in older adults: What is the difference? Clinical Geriatrics 2009;17(3):32-37.
9. Valuck RJ, Ruscin JM. A case-control study on adverse effects: H2 blocker or proton pump inhibitor use and risk of vitamin B12 deficiency in older adults. J Clin Epidemiol 2004;57:422-428.
10. Vanderhoff BT, Tahboub RM. Proton pump inhibitors: An update. Am Fam Physician 2002;66:273-280.
11. Pham CQ, Regal RE, Bostwick TR, et al. Acid suppressive therapy use on an inpatient internal medicine service. Ann Pharmacother 2006;40:1261-1266.
12. Shi S, Klotz U. Proton pump inhibitors: An update of their clinical use and pharmacokinetics. Eur J Clin Pharmacol 2008;64:935-951. Published Online: August 5, 2008.
13. Detsky ME, Juurlink DN. Does gastric acid suppression increase the risk of community-acquired pneumonia? CMAJ 2005;172(3):331.
14. Bhatt DL, Scheiman J, Abraham NS, et al; American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use: A Report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. Circulation 2008;118:1894-1909. Published Online: October 3, 2008.
15. Manoharan T, Darzins P. Acid suppression in the elderly. Australasian Journal on Ageing 2006;25(3):164-166.
16. Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother2007;5(4):345-351.
17. Sutfin T, Balmer K, Boström H, et al. Stereoselective interaction of omeprazole with warfarin in healthy men. Ther Drug Monit 1989;11:176-184.
18. Kiley CA, Cragin DJ, Roth BJ. Omeprazole-associated digoxin toxicity. South Med J 2007;100(4):400-402.
19. Oosterhuis B, Jonkman JH, Anderson T, et al. Minor effect of multiple dose omperazole on the pharmacokinetics of digoxin after a single oral dose. B J Clin Pharmacol 1991;32:569-572.
20. McCarthy DM, McLaughlin TP, Griffis DL, Yazdani C. Impact of cotherapy with some proton pump inhibitors on medical claims among HMO patients already using other common drugs also cleared by cythochrome. Am J Ther 2003;10:330-340.
21. Early communication about ongoing safety review of clopidogrel bisulfate (marketed as Plavix). U.S. Food and Drug Administration. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm079520.htm. Updated February 23, 2010. Accessed June 28, 2010.
22. Small DS, Farid NA, Payne CD, et al. Effects of the proton pump inhibitor lansoprazole on the pharmacokinetics and pharmacodynamics of prasugrel and clopidogrel. J Clin Pharmacol 2008;48:475-484. Published Online: February 26, 2008.
23. Siller-Matula JM, Spiel AO, Lang IM, et al. Effects of pantoprazole and esomeprazole on platelet inhibition by clopidogrel. Am Heart J 2009;157:148e1-148.e5. Published Online: November 6, 2008.
24. Gilard M, Arnaud B, Cornily JC, et al. Influence of omeprazole on the antiplatelet action of clopidogrel associated with aspirin: The randomized, double-blind OCLA (Omeprazole CLopidogrel Aspirin) study. J Am Coll Cardiol 2008;51:256-260.
25. Gilard M, Arnaud B, Le Gal C, et al. Influence of omeprazole on the antiplatelet action of clopidogrel associated to aspirin. J Thromb Haemost 2006;4:2508-2509. Published Online: August 8, 2006.
26. Ho MP, Maddox TM, Wang L, et al. Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome JAMA 2009;301:937-944.
27. Ray WA, Murray KT, Griffin MR, et al. Outcomes with concurrent use of clopidogrel and proton pump inhibitors: A cohort study. Ann Intern Med 2010;152 (6):337-345.
28. Stockl KM, Le L, Zakharyan A, et al. Risk of rehospitalization for patients using clopidogrel with a proton pump inhibitor. Arch Intern Med 2010;170(8):704-710.
29. Aseeri M, Schroeder T, Kramer J, Zackula R. Gastric acid suppression by proton pump inhibitors as a risk factor for clostridium difficile-associated diarrhea in hospitalized patients. Am J Gastroenterol 2008;103:2308-2313. Published Online: August 12, 2008.
30. Yearsley KA, Gilby LJ, Ramadas AV, et al. Proton pump inhibitor therapy is a risk factor for clostridium difficile-associated diarrhea. Aliment Pharmacol Ther 2006;24:613-619.
31. Dial S, Alrasadi K, Manoukian C, et al. Risk of clostridium difficile diarrhea among hospital inpatients prescribed proton pump inhibitors: Cohort and case-control studies. CMAJ 2004;171:33-38.
32. Leonard J, Marshall JK, Moayyedi P. Systematic review of the risk of enteric infection in patients taking acid suppression. Am J Gastroenterol 2007;102:2047-2056. Published Online: May 17, 2007.
33. Shah S, Lewis A, Leopold D, et al. Gastric acid suppression does not promote clostridial diarrhoea in the elderly. QJM 2000;93:175-181.
34. Cunningham R, Dale B, Undy B, Gaunt N. Proton pump inhibitors as a risk factor for clostridium difficile diarrhoea. J Hosp Infect 2003;54:243-245.
35. Lowe DO, Mamdani MM, Kopp A, et al. Proton pump inhibitors and hospitalization for clostridium difficile-associated disease: A population-based study. Clin Infect Dis 2006;43:1272-1276. Published Online: October 13, 2006.
36. Howell MD, Novack V, Grgurich P, et al. Iatrogenic gastric acid suppression and the risk of nosocomial Clostridium difficile infection. Arch Intern Med 2010;170(9):784-790.
37. Untersmayr E, Bakos N, Scholl I, et al. Anti-ulcer drugs promote IgE formation toward dietary antigens in adult patients. FASEB 2005;19(6):656-658. Published online January 25, 2005.
38. Untersmayr E, Schöll I, Swoboda I, et al. Antacid medication inhibits digestion of dietary proteins and causes food allergy: A fish allergy model in BALB/c mice. J Allergy Clin Immunol 2003;112:616-623.
39. Laheij RJ, Sturkenoboom MC, Hassing RJ, et al. Risk of community-acquired pneumonia and use of gastric acid-suppressive drugs. JAMA 2004;292(16):1955-1960.
40. Gulmez SE, Holm A, Frederiksen H, et al. Use of proton pump inhibitors and the risk of community-acquired pneumonia: A population-based case-control study. Arch Intern Med 2007;167:950-995.
41. Sarkar M, Hennessy S, Yang Y. Proton-pump inhibitor and the risk for community-acquired pneumonia. Ann Intern Med 2008;149:391-398.
42. Herzig SJ, Howell MD, Ngo LH, Marcantonio ER. Acid-suppressive medication use and the risk for hospital-acquired pneumonia. JAMA 2009;301(20):2120-2128.
43. Sataloff R. Community-acquired pneumonia and use of gastric acid-suppressive drugs. JAMA 2005;293:7:795-796.
44. Gregor JC. Acid suppression and pneumonia: A clinical indication for rational prescribing. JAMA 2004;292:16:2012-2013.
45. Yang YX, Lewis, JD, Epstein, S. Metz DC. Long-term proton pump inhibitor therapy and risk of hip fracture. JAMA 2006;296:2947-2953.
46. Vestergaard P, Rejnmark L, Mosekilde L. Proton pump inhibitors, histamine H2 receptor antagonists, and other antacid medications and the risk of fracture. Calcif Tissue Int 2006;79:76-83. Published Online: August 15, 2006.
47. Targownik LE, Lix LM, Metge CJ, et al. Use of proton pump inhibitors and risk of osteoporosis-related fractures. CMAJ 2008;179:319-326.
48. Roux C, Briot K, Gossec L, et al. Increase in vertebral fracture risk in postmenopausal women using omeprazole. Calcif Tissue Int 2009;84(1):13-19. Published Online: November 21, 2008.
49. Coté GA, Howden CW. Potential adverse effects of proton pump inhibitors. Curr Gastroenterol Rep 2008;10:208-214.
50. Gray SL, LaCroix AZ, Larson J, et al. Proton pump inhibitor use, hip fracture, and change in bone mineral density in postmenopausal women: Results from the Women’s Health Initiative. Arch Intern Med 2010;170(9):765-771.
51. Johnson DA. Do ppis increase risk for hip fracture? Journal Watch. http://gastroenterology.jwatch.org/cgi/content/full/2007/105/1. Accessed June 21, 2010.
52. Fried M, Siegrist H, Frei R, et al. Duodenal bacterial overgrowth during treatment in outpatients with omeprazole. Gut 1994;35:23-26.
53. Howden CW. Vitamin B12 levels during prolonged treatment with proton pump inhibitors. J Clin Gastroenterol 2000;30(1):29-33.
54. Laine L, Ahnen D, Mcclain C, et al. Review article: Potential gastrointestinal effects of long-term acid suppression with proton pump inhibitors. Aliment Pharmacol Ther 2000;14(6):651-668.
55. Force RW, Meeker AD, Cady PS, et al. Ambulatory care increased vitamin B12 requirement associated with chronic acid-suppression therapy. Ann Pharmacother 2003;37:490-493.


