Pneumonia in Children: Update on Causes—and Treatment Options
ABSTRACT: Pneumonia is one of the most common conditions encountered by primary care providers. Certain organisms cause pneumonia in particular age groups. For example, group B streptococci, Gram-negative bacilli (Escherichia coli in particular) and, rarely, Listeria monocytogenes cause pneumonia in neonates. In infants younger than 3 months, group B streptococci and organisms encountered by older children occasionally cause pneumonia, as does Chlamydia trachomatis. Older infants and preschoolers are at risk for infection with Streptococcus pneumoniae and Haemophilus influenzae. In children older than 5 years, S pneumoniae and Mycoplasma pneumoniae are the key pathogens. Let the patient’s age, history, clinical presentation, and radiographic findings guide your choice of therapy. Even though most patients with uncomplicated pneumonia can be treated as outpatients, close follow-up is important. Hospitalize patients younger than 6 months and those with complications.
Key words: pediatric pneumonia, acute respiratory infection
______________________________________________________________________________________________________
Pneumonia is one of the most common conditions seen by primary care physicians who treat children. Respiratory symptoms are among the most common reasons why outpatients seek medical care. The distinction between upper respiratory tract disease and pneumonia should be made so that pneumonia is managed appropriately.
Here we summarize the evaluation of pediatric pneumonia and offer our management recommendations—based on a literature review and on clinical experience—in the outpatient setting.
EPIDEMIOLOGY AND ETIOLOGY
Annually, 2 million children younger than 5 years die of acute respiratory infections. The majority of these deaths occur in Africa and Southeast Asia.1,2 Mortality is much lower in the United States, but morbidity is substantial. In 2000, more than 170,000 children younger than 15 years (excluding newborns) were hospitalized with pneumonia for an average inpatient stay of 3 to 4 days.3 In children younger than 15 years, pneumonia was the documented discharge diagnosis in 28.6 per 10,000 population.3
The exact cause of pneumonia is not determined in most pediatric cases because of the difficulty in obtaining sputum specimens and the low incidence of bacteremia in children.4 Respiratory viruses are a major cause of pneumonia and occur frequently in all age groups—especially in infants and young children. The most common causes of pneumonia include influenza A and B viruses; respiratory syncytial virus (RSV); and Haemophilus parainfluenzae types 1, 2, and 3. Adenovirus and rhinovirus can also cause pneumonia.
The importance of metapneumovirus as a causative agent of childhood pneumonia is still being clarified, as is its role in producing more severe symptoms if coinfection with RSV is present.5
In 2003, coronavirus caused an epidemic of severe acute respiratory syndrome outside the United States (Hong Kong in particular).6 Keep this infection in mind in children who have traveled internationally.
Certain organisms cause pneumonia at particular ages (Table). This makes it possible to select antimicrobials based on a patient’s age. Neonates can become infected with maternal vaginal and rectal flora; therefore, group B streptococci (Streptococcus agalactiae), Gram-negative bacilli (Escherichia coli in particular), and rarely, Listeria monocytogenes are the causes of pneumonia in this age group. In the developing world, Staphylococcus aureus often affects newborns.7

In infants younger than 3 months, group B streptococci and organisms encountered by older children (see Table) occasionally cause pneumonia, along with Chlamydia trachomatis. This atypical pathogen is of particular concern in children between 2 and 19 weeks old.8 Infection with Ureaplasma urealyticum may also present as afebrile pneumonia, but its role in causing disease in young, healthy infants is controversial.9
Older infants and preschoolers (those younger than 5 years) have a great possibility of being infected with Streptococcus pneumoniae. S pneumoniae and Haemophilus influenzae are the leading bacterial pathogens in the developing world.7 Until 2000, S pneumoniae caused more than 100,000 hospitalizations for pneumonia in the United States. The incidence of sterile-site infections was 21 to 33 per 100,000 population.10 In 2002, the rate of invasive pneumococcal disease was 13 per 100,000 population; the decline followed the introduction of the conjugate pneumococcal vaccine in 2001. The effect of the conjugate pneumococcal vaccine on the cause of pediatric pneumonia is yet to be determined.
In children older than 5 years, S pneumoniae and Mycoplasma pneumoniae play the most important roles in causing pneumonia. Michelow and colleagues11 found that S pneumoniae was the most commonly identified organism in hospitalized children aged 2 months to 17 years in 1999-2000. Other bacterial pathogens that were rarely detected included Streptococcus pyogenes, Streptococcus milleri, and S aureus. H influenzae (nontypeable more likely in the immunized child) and Moraxella catarrhalis were not detected in any of the patients in that study, but data from other developed countries attest to infrequent occurrences of these pathogens in early childhood.12
The atypical pathogens M pneumoniae and Chlamydia pneumoniae are, respectively, the second and third most commonly identified bacterial causes of community-acquired pneumonia11 and are especially prevalent in the 5- to 10-year-old age group.12 However, preschool-aged children are also at risk: in Michelow’s study, they experienced as many episodes of atypical pneumonia as older children.11 Approximately one quarter of patients may have a mixed bacterial and viral infection.
PATHOGENESIS
Pneumonia results from invasion of the lower respiratory tract with an infectious agent that originated in the upper respiratory tract or bloodstream. Bacterial pathogens can produce bronchopneumonia (patchy consolidation) or lobar pneumonia (whole-lobe or partial-lobe consolidation). The pathology of lobar pneumonia is characterized by the presence of bacteria; vascular engorgement; and the massive influx of erythrocytes, neutrophils, and fibrin into the alveolar space.13 Eventually, resolution occurs when macrophages clean up the debris of the fibrinous exudate.
Complications may arise if tissue necrosis persists (forming an abscess) or if fluid spreads to the pleural space (forming a pleural effusion or empyema). Since the advent of the conjugate pneumococcal vaccine, the number of cases of empyema secondary to S pneumoniae pneumonia has decreased. S aureus has become the most commonly identified cause of empyema in children.14 Although a general pattern of disease can be associated with certain organisms—such as lobar pneumonia secondary to S pneumoniae infection and empyema more likely resulting from S aureus infection—any of these manifestations can result from infection with any of the bacterial pathogens.15
Viruses and atypical pathogens can produce an interstitial pneumonitis in which the inflammatory reaction in the lower respiratory tract is limited to the alveolar wall. Typically, the alveolar spaces are free of exudates but the alveolar septae are widened from the influx of various inflammatory cells.13 A secondary bacterial infection may develop in a patient already infected with a virus or atypical pathogen, especially in the presence of alveolar exudates. Suspect this complication when a patient experiences resurgence of fever, worsening of symptoms and change in the radiographic findings.
CLINICAL PRESENTATION
The type of pneumonia and age of the patient affect the clinical presentation. In general, bacterial pneumonia presents abruptly with high fever and may be accompanied by a productive cough. Viral or atypical pneumonia can present insidiously with upper respiratory tract symptoms, wheezing, and minimal fever.
Neonates with pneumonia display respiratory distress, temperature instability, and lethargy. Early onset of group B streptococcal disease usually occurs within the first 24 hours of life, but it can occur at any time between 0 and 6 days of age.16
The infant with pneumonia in the first several months of life may be febrile, tachypneic or apneic, and irritable. Fever and tachypnea may be the only findings in a young infant or toddler with pneumonia. Atypical pathogens (ie, C trachomatis) can lead to an afebrile illness accompanied by cough, tachypnea, or wheezing.
The older child with bacterial pneumonia will experience abrupt onset of fever, cough, and malaise. Minimal fever, malaise, and lingering cough typify atypical pneumonia. Poor oral intake, nausea, vomiting, and abdominal pain may manifest in any person with pneumonia.
EVALUATION
The patient’s history of present illness and past medical history are essential in determining the possible cause of the pneumonia. Note the patient’s immune status: an immunocompromised child may have an opportunistic infection (with Pneumocystis carinii, for example) in addition to infection with the typical and atypical organisms that an immunocompetent child may encounter. A history of international travel and the time of year that the symptoms are occurring expand the list of possible pathogens.
During the physical examination, determine the respiratory rate for a full minute—especially in younger patients—and compare the rate with normal values for that child’s age group. Observe the patient for any signs of respiratory distress (retractions, cyanosis) and auscultate the chest for wheezing, rhonchi, or decreased breath sounds. In older patients, it may be possible to check for signs of lower respiratory tract disease, such as dullness to percussion, increased fremitus, and egophony.
When you suspect viral pneumonia or if influenza and/or RSV infection are prevalent in your community, perform a rapid antigen test (if readily available). The difficulty of obtaining an adequate sputum sample in a young child precludes sputum analysis from being a routine component of the outpatient evaluation of uncomplicated pediatric pneumonia. A total serum white blood cell count and differential and measurement of sedimentation rate and C-reactive protein level are nonspecific aids that may provide evidence for a viral or bacterial cause. Blood cultures are of limited value in the diagnosis of pneumonia but should be obtained in the young febrile infant—especially if that infant is not fully immunized against pneumococci.
Anteroposterior and lateral chest radiographs help reveal areas of consolidation or interstitial disease in the ill patient (Figure 1). The pattern of abnormal findings on x-ray films provides a clue to the possible causative agent. Bacteria (S pneumoniae) are more likely to produce a lobar pattern and viral or atypical pathogens are more likely to produce an interstitial pattern. These radiographic descriptions are not absolute: bacterial and viral pathogens can produce various patterns of radiographic findings.

Occasionally we have seen patients whose radiographic features lagged behind the clinical presentation. Dehydration may affect the radiographic results. Hash and associates17 described an association between improved hydration and worsening of chest film findings in adults with clinical pneumonia. A patient may have a normal initial chest radiograph, but—after hydration is improved—an infiltrate may become evident on a subsequent film.17
During outpatient treatment, order follow-up chest radiographs when you suspect a complication such as pleural effusion or empyema, evidenced by chest pain, failure to respond to antibiotics, recurrence of fever, and worsening respiratory tract signs. Upright and lateral decubitus radiographs also may be necessary in this setting. After a patient completes therapy for uncomplicated pneumonia, repeated chest radiographs are not necessary; if they are obtained, however, be aware that initial radiographic abnormalities may take 6 or more weeks to resolve.
The chest radiograph is not capable of detecting all pneumonias. High-resolution CT scans can detect infiltrates that are not evident on plain chest radiographs,18 but this modality is not usually readily available in most outpatient settings. A chest CT scan may be required in a pediatric patient with a normal chest radiograph and serious or unexplained respiratory symptoms—especially a febrile immunocompromised patient.19
More invasive testing is not routine in the general pediatric clinic. In complicated cases, referral for bronchoscopy; bronchoalveolar lavage; or collection of a pleural fluid sample for culture, Gram stain, and analysis (cell count; levels of glucose, protein, and lactate dehydrogenase; pH; and specific gravity) may be needed.
TREATMENT
The patient’s age, history, clinical presentation, and radiographic findings guide the choice of therapy. Should the child be hospitalized or treated as an outpatient? Is the child’s illness most likely the result of a virus? Bacterium? Atypical pathogen? If you suspect viral infection, supportive care includes adequate hydration, oxygen, and analgesics for general discomfort. If influenza is diagnosed within 48 hours of illness, the child may be a candidate for the available anti-influenza medications.20 When you suspect bacterial or atypical pneumonia, base your choice of empiric antibiotic therapy on the most likely causative organisms.
Patients who are up to 6 months old need to be hospitalized and treated with intravenous antibiotics effective against the typical causative agents in this age group. Obtain blood samples for culture before you start therapy. If afebrile pneumonitis is likely, outpatient treatment with a macrolide is appropriate. Although there is an association between orally administered erythromycin and the development of pyloric stenosis in infants younger than 6 weeks, the American Academy of Pediatrics still recommends erythromycin for suspected Chlamydia infections.8 Be sure to warn parents of this possible association.
The older infant, toddler, and school-aged child can be treated safely as an outpatient if the patient is immunocompetent, appears to be well, is able to stay adequately hydrated, and is not hypoxic. When viral pneumonia is likely, provide supportive care for the child. For the young child with suspected bacterial pneumonia, we recommend initial therapy with amoxicillin, amoxicillinclavulanate, or cefuroxime. If resistant S pneumoniae is a major factor in your community, high-dose amoxicillin may be necessary.
Clindamycin is an alternative if a child with suspected pneumococcal infection is beta-lactam–allergic. A macrolide is another option; however, standard doses of azithromycin, for example, provide marginal beta-lactamase coverage. Although S pneumoniae is the most likely bacterial cause of pneumonia, antibiotics such as amoxicillin-clavulanate and cefuroxime allow for treatment of beta-lactamase–producing organisms (such as nontypeable H influenzae), which may be an increasing threat in this era of conjugate pneumococcal vaccine use.
Treat the older child and adolescent with a macrolide initially because atypical pathogens have a greater significance in this age group. If the child fails to respond, it is reasonable to add or switch to one of the previously mentioned antibiotics.
The management of a complication of pneumonia depends on its severity; patients typically require hospitalization for close monitoring. Pneumonia with a small effusion can be successfully treated with antibiotics alone, but large parapneumonic effusions and empyemas often require drainage.14 Seek surgical consultation to determine the best course for each circumstance.
Because the treatment of pneumonia is empiric, outpatients need to be reevaluated frequently to ensure adequate response. Hospitalization is necessary for the child whose health worsens despite optimal outpatient management.
COMPLICATIONS
Complications of pneumonia can be local and may occur secondary to the spread of pulmonary infections to contiguous structures (eg, pleural effusion and empyema, pericarditis, and worsening of pulmonary infection leading to formation of a pulmonary abscess) (Figure 2). Complications can also be systemic; they may arise secondary to bacteremia, which can cause meningitis, osteomyelitis, or septic arthritis.
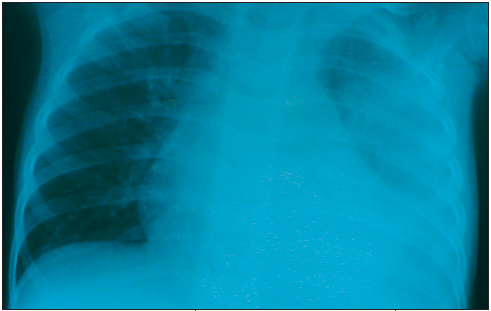
Figure 2 – This chest film shows a left-sided pleural effusion associated with pneumonia.
Bacterial pneumonia is the most common cause of pleural effusion or empyema. Pleural effusion can be a part of the clinical spectrum of pneumonia as a synpneumonic effusion, or it may be a complication that leads to an accumulation of pus in the pleural cavity, resulting in an empyema. Patients often have signs and symptoms of pneumonia along with a characteristic pleural rub (especially in small pleural collections), worsening of fever, respiratory distress, decreased air entry on the affected side, dullness to percussion, and mediastinal shift to the opposite side if the fluid accumulation is rapid and significant. These complications are more common in patients with staphylococcal or streptococcal pneumonias and in those who use antibiotics inappropriately or incompletely.
Treatment of children with a complication includes ultrasonograms or chest CT scans for diagnosis, use of antibiotics based on sensitivity patterns, and thoracotomy with tube drainage. Most patients respond to these interventions and rarely require additional interventions such as injection of fibrinolytic agents into the pleural space.
REFERENCES:
1. Woodwell DA, Cherry DK. National Ambulatory Medical Care Survey: 2002 Summary. Advance Data From Vital and Health Statistics. No. 346. August 2004. Available at: www.cdc.gov/nchs/data/ad/ad346.pdf. Accessed August 1, 2005.
2. Williams BG, Gouws E, Boschi-Pinto C, et al. Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect Dis. 2002;2:25-32.
3. Kozak LJ, Hall MJ, Owings MF. National Hospital Discharge Survey: 2000 annual summary with detailed diagnosis and procedure data. National Center for Health Statistics. Vital Health Stat 13. 2002;153: 1-194.
4. Juven T, Mertsola J, Waris M, et al. Etiology of community-acquired pneumonia in 254 hospitalized children. Pediatr Infect Dis J. 2000;19:293-298.
5. Konig B, Konig W, Arnold R, et al. Prospective study of human metapneumovirus infection in children less than 3 years of age. J Clin Microbiol. 2004;42:4632-4635.
6. Leung CW, Kwan YW, Ko PW, et al. Severe acute respiratory syndrome among children. Pediatrics. 2004;113:e535-e543.
7. Centers for Disease Control and Prevention Division of Bacterial and Mycotic Diseases. Pneumonia among children in developing countries. Available at: www.cdc.gov/ncidod/dbmd/diseaseinfo/pneumchilddevcount_t.htm. Accessed August 1, 2005.
8. American Academy of Pediatrics. Chlamydia trachomatis. In: Pickering LK, ed. Red Book: 2003 Report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, Ill: American Academy of Pediatrics; 2003:238-243.
9. American Academy of Pediatrics. Ureaplasma urealyticum infections. In: Pickering LK, ed. Red Book: 2003 Report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, Ill: American Academy of Pediatrics; 2003:671-672.
10. Centers for Disease Control and Prevention Division of Bacterial and Mycotic Diseases. Streptococcus pneumoniae disease. Available at: www.cdc.gov/ncidod/dbmd/diseaseinfo/streppneum_t.htm. Accessed August 1, 2005.
11. Michelow IC, Olsen K, Lozano J, et al. Epidemiology and clinical characteristics of communityacquired pneumonia in hospitalized children. Pediatrics. 2004;113:701-707.
12. Heiskanen-Kosma T, Korppi M, Jokinen C, et al. Etiology of childhood pneumonia: serologic results of a prospective, population-based study. Pediatr Infect Dis J. 1998;17:986-991.
13. Kobzik L. The lung. In: Cotran RS, Kumar V, Collins T, et al, eds. Robbins Pathologic Basis of Disease. 6th ed. Philadelphia: WB Saunders Company; 1999:717-721.
14. Schultz KD, Fan LL, Pinsky J, et al. The changing face of pleural empyemas in children: epidemiology and management. Pediatrics. 2004;113: 1735-1740.
15. Klein JO. Bacterial pneumonias. In: Feigin RD, Cherry JD, Demmler GJ, Kaplan SL, eds. Textbook of Pediatric Infectious Diseases. 5th ed. Philadelphia: WB Saunders Company; 2004:299-310.
16. American Academy of Pediatrics. Group B streptococcal infections. In: Pickering LK, ed. Red Book: 2003 Report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, Ill: American Academy of Pediatrics; 2003:585-591.
17. Hash RB, Stephens JL, Laurens MB, Vogel RL. The relationship between volume status, hydration, and radiographic findings in the diagnosis of community- acquired pneumonia. J Fam Pract. 2000;49: 833-837.
18. Syrjala H, Broas M, Suramo I, et al. High-resolution computed tomography for the diagnosis of community-acquired pneumonia. Clin Infect Dis. 1998;27:358-363.
19. Kuhn JP, Brody AS. High-resolution CT of pediatric lung disease. Radiol Clin North Am. 2002;40: 89-110.
20. Nield LS, Kamat DM. Influenza: are you ready? Consultant for Pediatricians. 2004;3:436-440.


