Pericardial Cyst
 A 28-year-old Caucasian male presented to our hospital for evaluation of hematuria. CT showed a 20 cm diameter cystic mass occupying about two-thirds of his right hemithorax (Figures 1 and 2), which was producing severe extrinsic mass effect upon the right lung base, heart border, and dome of the hemidiaphragm. The mass had a smooth thin wall, no internal septation, fat, or calcification. Its fluid content had an attenuation of 13 HU. Initial assessment included cystic adenoid malformation, hamartoma, bronchogenic, or hydatid cyst.
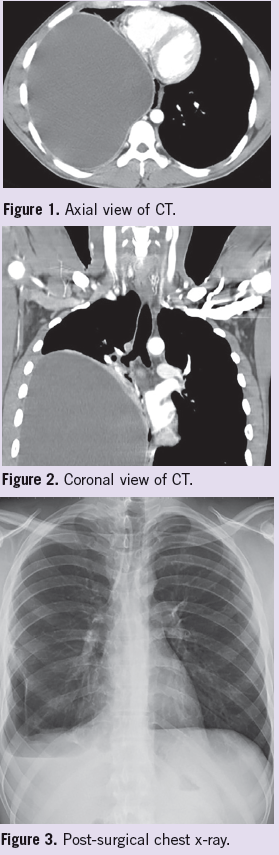
A 28-year-old Caucasian male presented to our hospital for evaluation of hematuria. CT showed a 20 cm diameter cystic mass occupying about two-thirds of his right hemithorax (Figures 1 and 2), which was producing severe extrinsic mass effect upon the right lung base, heart border, and dome of the hemidiaphragm. The mass had a smooth thin wall, no internal septation, fat, or calcification. Its fluid content had an attenuation of 13 HU. Initial assessment included cystic adenoid malformation, hamartoma, bronchogenic, or hydatid cyst.
The patient had long-standing respiratory symptoms, which included exertional dyspnea—a chronic productive cough that is attributed to his smoking habit and asthma. He reported 1 episode of severe right side pleuritic chest pain a few weeks prior to this admission that resolved on its own. He had no history of weight loss, exposure to carcinogens other than nicotine, birds, sick contacts, or recent travel.
Physical examination. The patient was a thin-build male with normal vital signs, exhibiting asymmetrical thoracic wall, and negative signs of respiratory distress. The right inferior portion of the thorax was prominent; however, expansion was normal. On auscultation, breath sounds were decreased in the right pulmonary field with no evidence of rales or wheezes. The inferior two-thirds of the right pulmonary field were dull to percussion as well as having diminished tactile fremitus. Cardiac auscultation was normal with no displacement of point of maximal impulse. No adenopathies or masses palpated. Otherwise, the rest of his examination was unremarkable.
Laboratory tests. An ultrasound guided percutaneous biopsy and aspiration was performed of the cystic mass. Approximately 2 L of exudative brown-tinged fluid was removed, which was negative for malignant cells. Biopsy report indicated hypocellular fibrous tissue with a focal lymphoblastic aggregation and pigment laden macrophages with no evidence of malignancy.
Due to the size of the mass and patient symptoms, a right thoracotomy with resection of the intrathoracic cyst was performed; however, the surgery was uneventful. The patient had a quick recovery. Post-surgical chest x-rays identified expansion of the right lung and resolution of hydropneumothorax (Figure 3). Final pathology report determined the cystic mass to be a pericardial cyst with no evidence of malignancy.
Discussion. Pericardial cysts are uncommon benign congenital intrathoracic anomalies.1,2 They are caused by an incomplete coalescence of fetal lacunae forming the pericardium.2 The estimated incidence of pericardial cysts is 1:100,000.3 More than 60% are discovered between the ages of 30 to 50.
In about 70% of cases, cysts localizes at the right cardiophrenic angle,1 but they can also develop along the upper mediastinum, hilus, or cardiac border.1,4 They are typically unilocular, are lined by endothelium or mesothelium, contain clear serous fluid, and do not communicate with the pericardial space.2 Most of them are asymptomatic and found incidentally.1,3 Episodes of chest pain, tachycardia, persistent cough, cardiac arrhythmias, and lower respiratory tract infection have been described.2,5
Treatment depends on severity of symptoms. When asymptomatic, monitoring with periodic ultrasound is needed to assess size progression. There are reports of spontaneous resolution of pericardial cysts. If rapidly enlargement of cyst size or development of symptoms, surgical resection, or drainage need to be performed when feasible.1, 2
References:
1.Najib MQ, Chaliki HP, Raizada A, et al. Symptomatic pericardial cyst: a case series. Eur J Echocardiogr. 2011;12(11):E43.
2.Satur CM, Hsin MK, Dussek JE. Giant pericardial cysts. Ann Thorac Surg. 1996;61(1):208-210.
3.Elamin WF, Hannan K. Pericardial cyst: an unusual cause of pneumonia. Cases J. 2008;1(1):
26.
4.Hamad HM, Galrinho A, Abreu J, et al. Giant pericardial cyst mimicking dextrocardia on chest X-ray. Rev Port Cardiol. 2013;32(1):49-52.
5.Patel J, Park C, Michaels J, et al. Pericardial cyst: case reports and a literature review. Echocardiography. 2004;21(3):269-272.


