Patent Foramen Ovale with Platypnea-Orthodeoxia due to Colonic Distention
Association of platypnea-orthodeoxia syndrome (POS) and patent foramen ovale (PFO) and association of PFO and stroke are well-described. In some cases, POS and cryptogenic strokes associated with PFO can be effectively treated with PFO closure; however patient selection remains uncertain. This article presents a case of a large PFO associated with ischemic stroke and reversible POS due to colonic distention resulting in the right hemidiaphragm elevation in the setting of obstipation.
HISTORY
An 81-year-old man was admitted with acute right-sided weakness and dysarthria 3 days after colonoscopy. Acute stroke in the left middle cerebral artery distribution was confirmed. The patient was emergently treated with tissue plasminogen activator with good response. Carotid arterial duplex showed only mild atherosclerotic disease. Transthoracic echocardiogram revealed no valvular pathology but confirmed a PFO with a large right-to-left shunt and an atrial septal aneurysm. Venous duplex ultrasound showed acute left femoro-popliteal venous thrombosis raising suspicion for paradoxical embolization. Right ventricular function on echocardiogram was normal with no signs of pulmonary hypertension. Chest radiograph was notable for colonic interposition between the right hemidiaphragm and liver with resultant right hemidiaphragm elevation.
The patient was hospitalized 20 years earlier with a transient ischemic attack but had a large PFO first documented 8 years later. He had no history of arrhythmias, syncope, or malignancy. Cancer screening was up-to-date and negative. His risk factors for deep venous thrombosis (DVT) included history of varicose veins of the legs and a recent long car ride. With suspicion for paradoxical embolization, therapeutic anticoagulation was initiated, but chest CT showed no evidence of pulmonary embolism.
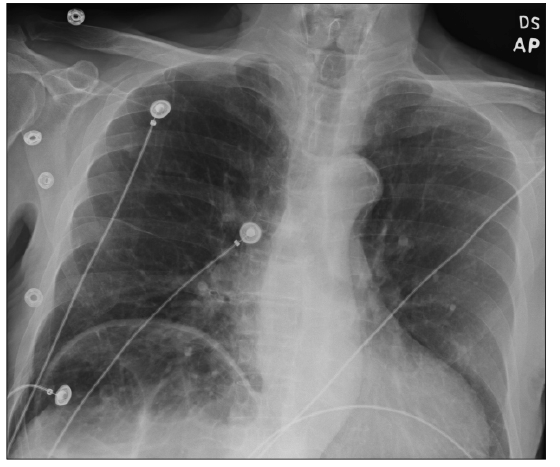
Figure 1. Repeat chest radiographs revealed worsened colonic interposition and distension and right hemidiaphragm elevation producing a shift of the heart into the left side of the chest.
CLINICAL OBSERVATIONS
During the next 2 days, progressive hypoxemia developed. The patient was noted to have POS: while sitting upright, oxygen saturation dropped down to 84% (PaO2 45 mm Hg) on 4 L oxymizer mask and into the high 70s on room air; in the supine position, oxygen saturation was 91% (PaO2 59 mm Hg) on room air. There was no shortness of breath and no increase in the work of breathing. ECG and cardiac troponins were unremarkable. Increased shunting across PFO was suspected as the cause of progressive hypoxemia. Cardiology consult advised against urgent PFO closure in the setting of recent stroke and did not believe that PFO acutely caused hypoxemia, which persisted despite noninvasive ventilation at this point. The patient developed mild leukocytosis and right lower quadrant abdominal discomfort. He had no bowel movements since admission.
RADIOLOGY
Repeat chest radiographs revealed colonic interposition and distension with right hemidiaphragm elevation producing a shift of the heart into the left side of the chest (Figure 1). Repeat bedside echocardiography showed the air filled colon compressing the right atrium, raising the possibility of the worsening right-to-left cardiac shunt. Over the next day, aggressive bowel regimen with colonic decompression produced large amounts of stool with subsequent resolution of hypoxia with POS and improvement of radiographic findings of subdiaphragmatic colonic distention (Figure 2). Arterial blood gas confirmed normalization of PaO2.
DISCUSSION
While platypnea-orthodeoxia syndrome is relatively uncommon1, PFO has estimated prevalence of 25%-30%. In some cases, POS has been successfully treated by PFO closure with presumably reduced ventilation-perfusion mismatch accentuated by orthostasis.2,3 After a lung surgery, or in the setting of pulmonary illness when pulmonary pressures rise, PFO may act as a release valve. However, shunting across PFO may occur even in the presence of normal pulmonary pressures and may occasionally result in stroke.4,5
The patient selection for PFO closure remains unclear due to mixed results in clinical trials fueling the debate of its hemodynamic significance.6 Both stroke and DVT incidence rise with age, strengthening the paradoxical embolization theory. However, being common, not all PFOs are associated with POS. It is possible that the degree of shunting across PFO may respond to changes of the intra-abdominal pressure, a connection that is likely to be overlooked.

Figure 2. Aggressive bowel regimen with colonic decompression produced large amounts of stool with resolution of hypoxia and platypnea-orthodeoxia and improvement of radiographic findings of subdiaphragmatic colonic distention.
In our patient with a preexisting large PFO, it was difficult to appreciate the exact degree of intracardiac shunt increase on bedside echocardiogram even though compression of the right cardiac chambers by the elevated hemidiaphragm was noted. The chest radiographs confirmed an elevated right hemidiaphragm due to colonic interposition that likely worsened the ventilation-perfusion mismatch. The gradual resolution of the POS following bowel decompression suggests that severe colonic distention played a significant role in worsening cardiopulmonary hemodynamics.
A case of severe POS requiring mechanical ventilation related to the right hemidiaphragmatic elevation in association with PFO was previously described. There, POS was attributed to the positional changes in the right atrial configuration that caused stretching of the PFO open.5 To our knowledge, this is the first case report of PFO associated with POS produced by colonic distention and severe obstipation. It illustrates that PFO may have variable impact on development of POS and that POS may result from interplay between hemodynamic factors, including rising intra-abdominal pressure.
Andrew K. Kurklinsky, MD, is an assistant professor of medicine at Mayo Clinic College of Medicine; division of cardiovascular medicine at Mayo Clinic in Jacksonville, FL.
Jose C. Yataco, MD, is an assistant professor of medicine at Mayo Clinic College of Medicine; department of critical care medicine at Mayo Clinic, Jacksonville, FL.
Mohamad H. Yamani, MD, is a professor of medicine at Mayo Clinic College of Medicine; division of cardiovascular medicine at Mayo Clinic, Jacksonville, FL.
Emir Festic, MD, is an assistant professor of medicine at Mayo Clinic College of Medicine; department of critical care medicine at Mayo Clinic, Jacksonville, FL.
References:
1.Rodrigues P, Palma P, Sousa-Pereira L. Platypnea-orthodeoxia syndrome in review: Defining a new disease? Cardiology. 2012;123(1):15-23.
2.Mojadidi MK, Gevorgyan R, Tobis J. The effect of patent foramen ovale closure in patients with orthodeoxia-platypnea syndrome. J Am Coll Cardiol. 2013;1:E1911.
3.Rodrigues P, Sousa-Pereira L, Palma P, et al. The mysterious intermittent hypoxemia. Eur Heart J. 2012;33:1110.
4.Cannarile P, Padeletti M, Maffei S, et al. Platypnea-ortodeoxia syndrome after an acute ischemic stroke. Eur Heart J. 2012;33:1109.
5.Sakagianni K, Evrenoglou D, Mytas D, Vavuranakis M. Platypnea-orthodeoxia syndrome related to right hemidiaphragmatic elevation and a 'stretched' patent foramen ovale. BMJ Case Rep. 2012;2012.
6.George S, Hildick-Smith D. Patent foramen ovale: Diagnosis, indications for closure and complications. Bri J of Cardiol. 2011;18(5-6):219-222.


