Opioid Analgesics for Persistent Pain in the Older Patient: Part II
Part I of this two-part article, published in the March issue of the Journal, provided information on selected general concepts in opioid therapeutics, including the role of opioids in pain management, treatment of concurrent acute pain, toxicity, and drug-drug interactions. Part II will discuss dosing of opioid analgesics, pharmacogenomics, and the individual agents.
Dosing of Opioid Analgesics
Due to space limitations, this dosing section will focus only on opioid-to-opioid switch therapy (also called “opioid rotation”), breakthrough pain (BTP) management, and methadone dosing.
Switching Opioid Analgesics
Opioid-to-opioid switch therapy should be reserved for four clinical reasons: (1) lack of efficacy (for worsening of existing pain, development of analgesic tolerance, or a dose for analgesia in combination products that causes acetaminophen daily-dose ingestion to exceed 4 g); (2) development of intolerable adverse events (AEs; gastrointestinal, central nervous system, cardiovascular); (3) change in patient status (inability to swallow, poor peripheral vascular access, poor or variable dermatologic absorption from transdermal [TD] formulations, requirement for high-dose opioids that cannot be practically administered); and (4) practical considerations (not available in local pharmacies, high cost, large amount needed, route of administration, and opiophobia [fear of 1 opioid “associated” with death or addiction]).1
In this process, the clinician must first calculate the morphine equianalgesic daily dose for the current opioid analgesic(s) using a dose equivalence table similar to the one illustrated in Table I. Then, the daily dose of the new opioid regimen can be calculated using the same table. Remember that equivalence values are route-specific (oral/rectal vs intramuscular [IM]/intravenous [IV]/subcutaneous [SC]). Since cross-tolerance between opioids is incomplete, the actual daily dose of the new opioid that should be prescribed should be lowered by 25-50%. Once the formulation is selected, the appropriate dosing interval (from 4-24 hr or even 72 hr) can be selected.1
When rotating from (an) other opioid(s) to TD fentanyl, two sets of recommendations are available. The very conservative set of recommendations from the initial manufacturer of the TD product (Ortho-McNeil-Janssen Pharmaceuticals, Inc) is illustrated in Table II. However, use of this set of recommendations produces suboptimal initial analgesia in over 50% of patients.2 A somewhat more “aggressive” set of recommendations derived from the results of clinical trials serves to minimize the initial suboptimal analgesia produced by the manufacturer’s set. Table III illustrates this more “aggressive” set of recommendations.3 Regardless of the recommendations used, patients need additional opioid during the initial 18-24 hours after application of the first TD patch to compensate for the lag time until the skin depot is saturated with drug and the delivery to the systemic circulation is at a steady state. Generally, the recommended supplemental opioid dose needed over this period is 25% of the equianalgesic daily dose of the previously-used regimen. Supplemental dosing will not only assist with analgesia during the transition period, but also prevent the emergence of opioid withdrawal signs/symptoms.3
Due to the complex mechanism of action of tramadol/tapentadol, these agents cannot be represented in a dose equivalence table such as Table I. Thus, they cannot enter into the process of opioid-to-opioid switch therapy, as discussed previously.

Breakthrough Pain Management
Along with the scheduled opioid dosage regimen, an “as-needed” opioid regimen is necessary to manage BTP. When precipitants of BTP are known (eg, movement, dressing, wound dressing changes, bathing), a dose of an immediate-release (IR) hydrophilic opioid such as oral morphine, hydromorphone, or oxycodone 0.5 hours before the precipitant can markedly reduce discomfort. With BTP not having a known precipitant, the same three opioids are useful if the pain is slow-onset in nature. In contrast, a lipophilic opioid such as fentanyl may be better if the pain is rapid-onset in nature.4,5
The distinction between hydrophilic and lipophilic opioids for BTP is based on the time-activity profiles of their analgesic effects. Hydrophilic opioids can take up to 30 minutes or more to provide “adequate” or “meaningful” analgesia, this despite the “anticipatory placebo response,” which may decrease this lag time by 10-20 minutes. Parenteral administration of these agents reduces the lag time to “adequate” or “meaningful” analgesia to 15 minutes, or perhaps less. In contrast, the lipophilic opioids have an onset of effect of 5-10 minutes (transmucosal [TM] fentanyl, sublingual methadone).4,5
 Regardless of the opioid selected for BTP, the selection of the actual dosage regimen has been poorly researched. Recommendations have included an oral IR opioid regimen that provides each “rescue” dose to be equal to 5-15% or 10-20% or one-sixth (16.7%) of the 24-hour dose of scheduled opioid. This dose is then offered every 4 hours, as needed. A BTP dose of 10% of the daily scheduled opioid dose, offered every 4 hours, is probably safe in most patients and is widely accepted.4,5
Regardless of the opioid selected for BTP, the selection of the actual dosage regimen has been poorly researched. Recommendations have included an oral IR opioid regimen that provides each “rescue” dose to be equal to 5-15% or 10-20% or one-sixth (16.7%) of the 24-hour dose of scheduled opioid. This dose is then offered every 4 hours, as needed. A BTP dose of 10% of the daily scheduled opioid dose, offered every 4 hours, is probably safe in most patients and is widely accepted.4,5
TM fentanyl as oral TM fentanyl citrate lozenges, fentanyl buccal tablets, or fentanyl buccal soluble film is the only practical lipophilic opioid available for BTP. Although lauded as a potential BTP opioid, methadone is too long-acting, and “as-needed” use may substantially augment the risk inherent in the complicated pharmacokinetics/pharmacodynamics of the drug.6
The dosing regimens of “rescue” TM fentanyl are not calculated as a percentage of the total daily maintenance opioid dose.7 For the lozenge formulation, dosing should be initiated at 200 mcg. For each separate pain event, up to two lozenges can be used (the second being started 15 min after completion of the first). The dose should not be escalated until three or four consecutive acute pain events have required two lozenges for pain relief. At that time, the dose should be increased to that of the next available dosage unit strength. The target of dose titration is the achievement of adequate analgesia with only one lozenge per BTP event. If drug intake takes more than 15 minutes or the lozenge is chewed or swallowed, the peak drug concentration will be reduced and analgesia may be compromised. The “lollipop” appearance and sweet taste makes this dosage formulation appealing to young children, in whom it is potentially lethal. Careful secure storage and disposal are mandatory if children may enter the patient’s environment. Dose titration of the buccal tablet formulation is carried out in the same manner as for the lozenge formulation. A unique AE of this formulation is the appearance of mucosal ulcers at the application site. Neither formulation should be used in more than four BTP episodes per day.4,5
With the TM soluble film formulation, titration begins using the 200-mcg strength. A maximum of one film should be used per BTP episode (another “rescue” analgesic can be used 0.5 hr following application of the film). After one failure of BTP treatment, the film strength can be increased by 200 mcg at the next BTP episode (there is no need to wait for 3 or 4 consecutive failures as with the other two TM products). As with the other TM products, this product should not be used in more than four BTP episodes over 24 hours (it also needs to be separated by at least 2 hr between applications). If multiple films must be used simultaneously, they should be spread out and not placed one on top of the next. This product is not intended to be a substitute for either of the other two TM products, as these products are not bioequivalent on a mcg-per-mcg basis.8
If the patient requires three or more “rescue” doses per day, retitration of the scheduled opioid dose is necessary. The increase is calculated on the basis of the total opioid dose (scheduled + “as-needed” doses) taken over the previous 24-hour period. The percentage increase is calculated on the basis of pain severity (eg, pain > 7/10, increase by 50-75+%; pain = 4-7/10, increase by 25-50%; pain < 4/10, increase by 25%). The size of each rescue dose then has to be increased by the same percentage amount.4,5
Many of the above considerations are generally not applicable to tramadol/tapentadol when used for BTP. With mean times to onset of analgesia and times to peak analgesia being 1 and 2-3 hours for tramadol and 1.5 and 3 hours for tapentadol, respectively, these agents would not be good choices for BTP.

Methadone
There is no role for routine therapeutic drug serum concentration monitoring with methadone since the drug concentration ranges associated with efficacy are extremely broad (11-146 and 40-1130 ng/mL in 2 studies).9,10 However, it may be useful in evaluating cases of suspected nonadherence or drug malabsorption. As discussed previously, methadone should only be used on a chronic basis and not as a “rescue” medication for BTP. When used in the nursing home setting, initiation and dosage changes for methadone should be carried out in the morning to take advantage of the long time interval before bedtime for careful patient assessment.
Since methadone has not been considered a potential first-line agent until recently, few data are available to assist clinicians in this use. In frail or older individuals, the initial dose should be 0.5-1 mg every 8 hours (as opposed to the usual initial regimens of 2.5-5 mg every 8 hours or 7.5 mg every 12 hours in the general adult population).11,12 Keeping in mind the second-phase pharmacokinetics of the drug, dosage changes should be made no more frequently than every 4-7 days.
In switching between parenteral and oral methadone, it is recommended to use a dose conversion ratio of 1:0.7 (oral:parenteral)13 and not the 2:1 ratio advocated previously. In switching from therapy with one to several opioids to methadone therapy, it is important to realize that there is more than one morphine:methadone dose conversion ratio to consider. As with any other opioid-to-opioid switch, the clinician must first calculate the morphine equianalgesic daily dose for the current opioid analgesic agent(s) using a dose equivalence table such as Table I. Then, depending on the actual value of the morphine equianalgesic daily dose, the appropriate morphine:methadone dose conversion ratio can be selected. In general, 4:1, 5:1, and 10:1 ratios (oral morphine:oral methadone) are used when the oral morphine equianalgesic doses are less than 90 mg/day, 91-400 mg/day, and greater than 400 mg/day, respectively.14
DO NOT USE THE 1-4:1 RATIOS COMMONLY LISTED IN STANDARD REFERENCES, AS THESE WERE CALCULATED USING SINGLE-DOSE DATA, SUBSTANTIALLY UNDERESTIMATING THE POTENCY OF CHRONIC METHADONE THERAPY.
Few data are available regarding the conversion of TD fentanyl to oral methadone therapy. In the best study to date, a dose conversion ratio of 1:20 (TD fentanyl:oral methadone) was utilized, with the TD patch being removed at the time of the initial oral methadone dose. Three-quarters of patients were successfully switched by this method (success defined as a reduction in pain intensity and/or distress score of 33% from baseline within 4-7 days).15
Another area with a paucity of data at present is the process of switching from methadone therapy to therapy with other opioids. This is understandable, considering the reticence of clinicians until recently to even consider using methadone as a first-line agent. From available information, a reasonable starting dose conversion ratio is 1:4-5 (oral methadone:oral morphine). Multiple, dose-dependent dose equivalence ratios, which occur with “other opioid(s)-to-methadone” switches, do not appear to be relevant when switching in the opposite direction.14,16 Of interest, a recent study has found an important difference in analgesic potency between IV and oral methadone, with methadone:oral morphine dose equivalence ratios of 1(oral):5 and 1(IV):13.5.16 Additional studies are required to investigate this difference further.
Pharmacogenomics
The era of pharmacogenomics, the study of the effect of genetic influences on the pharmacokinetics and pharmacodynamics of drugs, is still quite young. However, early investigations suggest that much of the variability in response to opioids may, in fact, be linked to gene-based effects on opioid-metabolizing proteins (CYP450 family), transporter proteins (mediating transport across the gut wall and blood-brain barrier, P-glycoprotein family), and mu-opioid receptors (OPRM1 is the gene encoding the mu-opioid receptor).17-19 For example, the interindividual variability in the activity of CYP450 isozyme 3A4 can exceed 40-fold. This is gene-based, since over 30 single nucleotide polymorphisms (SNPs) have been found for this enzyme. Large interindividual variability in the activities of isozymes 2B6, 2D6, 1A2, 2C8, 2C9, and 2C19 have also been found, each associated with multiple SNP forms. Transport proteins, such as those of the P-glycoprotein family, affect oral drug bioavailability and transport across the blood-brain barrier. Over 100 SNPs of the ABCB1 gene encoding P-glycoprotein have been found. Over 100 SNPs of the OPRM1 gene encoding the mu-opioid receptor have also been found. These latter variants may provide at least a partial explanation for the wide differences in magnitude of opioid analgesia and/or tolerability with a given dose and dosage requirements in patients.17-20 Whether or not determinations of these genetic polymorphisms will be useful, even on a limited basis, for optimizing pain control in opioid recipients in the future is unknown.
Individual Agents
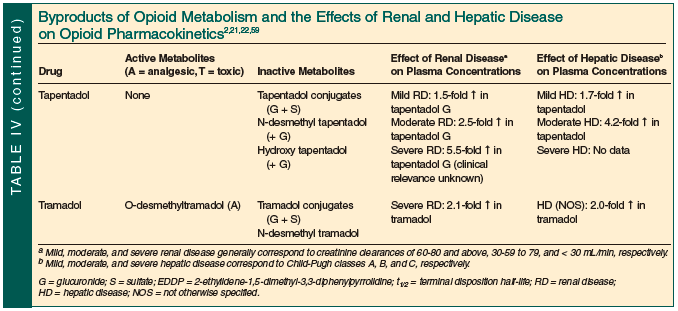
The reader is referred to Table IV for summaries of the metabolic byproducts of each of the 11 opioids reviewed, and the effects of renal and hepatic disease on their disposition.
Codeine
Analgesia begins within 10-30 minutes of oral codeine administration, peaks at 30-60 minutes, and lasts for 4-6 hours.2,21 After administration, the parent compound and six metabolites are found in plasma.2 The latter include the O-demethylated metabolite morphine, morphine 3- and 6-glucuronides (M-3-G and M-6-G, respectively), and the N-demethylated metabolite normorphine; codeine-6-glucuronide (C-6-G); and the N-demethylated metabolite norcodeine.22 The N-demethylated metabolites are inactive, while morphine, M-6-G, and C-6-G are active analgesics and M-3-G is an active neuroexcitatory toxin.22 Most of the analgesia of codeine is considered to be due to its active morphine metabolite. The two N-demethylation reactions are catalyzed via CYP450 isozyme 3A4.22 The O-demethylation of codeine to morphine and dihydrocodeine to dihydromorphine is mediated by CYP450 isozyme 2D6, an enzyme whose activity is under genetic control. Poor metabolizers (PMs) via this enzyme can be expected to derive less analgesia from codeine: 5-10% of Caucasians in Europe and North America and less than 2% of Asians, African Americans, Ethiopians, Saudis, and Australian aborigines.23 Co-administration of drugs inhibiting CYP450 isozyme 2D6 will have a similar effect (eg, cimetidine, amiodarone, quinine, quinidine, bupropion, selective serotonin and serotonin-norepinephrine reuptake inhibitors, ritonavir).24 In contrast, ultrafast metabolizers (UMs) via gene duplication may be expected to derive more analgesia from codeine: Scandinavians, 1-2%; Middle Europeans/North Americans, 4-5%; Southern Europeans, 7-12%; Asians, 0.5-2.5%; Saudis, 21%; and Ethiopians, 29%. However, a very real danger of fatal respiratory depression exists in UMs, especially if renal impairment co-exists.25
Fentanyl
Analgesia begins within 5-10 minutes of parenteral or TM fentanyl administration and lasts for 1-4 hours. Analgesia is delayed after application of a TD fentanyl patch due to the time needed to saturate the skin “reservoir” beneath the patch, thus producing a “depot” of drug. This period lasts for 12-14 hours, at which point fentanyl begins to enter the circulation. The duration of effect while the TD patch is maintained is 48-72 hours.21,26
Fentanyl is primarily metabolized, with only 7% being eliminated in unchanged form. Primary metabolites include the N-dealkylation product (via CYP450 isozyme 3A4) norfentanyl, the hydroxylated metabolites hydroxypropionyl fentanyl and hydroxypropionyl norfentanyl, propionic acid, and 4-N-anilinopiperidine. CYP450 isozymes 1A2, 2D6, 2C9, and 2C19 are also involved in fentanyl metabolism, although to a lesser extent than CYP450 3A4.21,22,26,27
Advancing age significantly alters fentanyl pharmacokinetics. In one study using TD fentanyl, the times to peak plasma concentrations (Cmax) were similar in the elderly (mean age, 83 yr) and young (mean age, 48 yr) groups. However, the t1/2 after patch removal was significantly longer in the elderly versus young group (means of 43 vs 20 hr, respectively; P < 0.05).28 In another study using IV fentanyl, the t1/2 was significantly prolonged (mean, 289 vs 945 min; P < 0.005), and the total body clearance was significantly reduced (mean, 0.991 vs 0.275L/min; P < 0.005) in elderly (mean age, 67 yr) as compared with young (mean age, 37 yr) patients. Age correlated with t1/2 (r = 0.82; P < 0.01) and total body clearance (r = -0.80; P < 0.05).29 In a study by Kharasch et al30 using the TM lozenge formulation (single 10-mcg/kg dose), there were no significant intergroup differences in pharmacokinetic parameters in elderly (60-75 yr) versus young (18-40 yr) subjects. However, using pupillometry to measure pharmacodynamic response, the elderly group had a significantly smaller maximum reduction in pupil diameter from baseline (3.1 vs 4.5 mm; P < 0.05), and the time to peak response was prolonged (1.04 vs 0.79 hr; P < 0.05).30
An increase in body temperature, from endogenous fever and exogenous heat sources (heat lamp, electric blanket) enhances fentanyl bioavailability through the skin, probably secondary to vasodilation and increased skin blood flow. A rise in oral temperature to 104 degrees F produced a mean 33% increase in serum fentanyl concentrations. Thus, fentanyl dosing may require adjustment during hyperthermia.
Hydrocodone and Hydromorphone
Generally thought of more as an antitussive, hydrocodone is also a potent opioid analgesic. After oral dosing, it has an onset of analgesic effect at 1 hour, peak effect at 2 hours, and a duration of action of 4-6 hours.2,21
It is primarily metabolized by O-demethylation (mediated via CYP450 isozyme 2D6) to the active metabolite hydromorphone followed by glucuronidation of both species. It is also metabolized by N-demethylation (mediated via CYP450 isozyme 3A4) to the active metabolite norhydrocodone.22,31 Approximately 40% of the elimination of hydrocodone occurs via non-CYP450–mediated pathways. Minor metabolites include dihydromorphine (which is active), dihydrocodeine, isodihydromorphine, isodihydrocodeine, and hydromorphone-3-glucuronide.22 Hydromorphone-3-glucuronide is neurotoxic. Hydrocodone is primarily considered a prodrug for hydromorphone and not as a primary analgesic. CYP450 isozyme 2D6 polymorphisms can be expected to play a similar role with respect to hydrocodone as they do with codeine (see above).
Levorphanol
The onset of levorphanol analgesia occurs at 10+ minutes after oral administration, peaks at 1 hour, and lasts for 6-8 (or more) hours.2An N-methyl-D-aspartate (NMDA) receptor antagonist like methadone, it appears to be primarily glucuronidated to an inactive 3-glucuronide metabolite. Whether it is neurotoxic like the 3-glucuronide metabolites of morphine and hydromorphone is not known. Little, if any, N-demethylation occurs in humans.21,22,32
Oxymorphone
The onset, peak, and duration of analgesia of the oral IR/extended-release (ER) formulations of oxymorphone are equal to or greater than 0.5/unknown hours, 1/unknown hours, and 4-6/12 hours, respectively.33 Oxymorphone is primarily metabolized by glucuronidation (to a 3-glucuronide), 7,8-ketoreduction (to 6-- and 6--hydroxyoxymorphone, which are subsequently glucuronidated at the 3-position), and N-demethylation (to noroxymorphone, which is subsequently glucuronidated at the 3-position). Only the hydroxy metabolites are considered to be active. However, whether or not the 3-glucuronide metabolites are neurotoxic is not known.21,22,34
Plasma oxymorphone, oxymorphone-3-glucuronide, and 6-hydroxy metabolite concentrations are increased by a mean of 40% in older ( 65 yr) as compared with younger (18-40 yr) subjects. On average, oxymorphone area under the curve (AUC) and Cmax are increased by 40% and 50%, respectively, in elderly as compared with young subjects.33
Oxycodone
Onset of analgesia after oral administration of IR and ER formulations are within 10-15 minutes and less than 1 hour, respectively. Peak analgesia occurs after 0.5-1 hour (both formulations) and lasts 3-4 hours (IR formulation) and 12 hours (ER formulation).2,21 Oxycodone is primarily metabolized by O-demethylation (to oxymorphone via CYP450 isozyme 2D6), by N-demethylation (to noroxycodone via CYP450 isozyme 3A4, which then undergoes glucuronidation at the 3-position), and by 7,8-ketoreduction (to 6-- and 6--oxycodol). Oxymorphone is subject to glucuronidation (to a 3-glucuronide), to N-demethylation (to noroxymorphone via CYP450 isozyme 2D6), and to 7,8-ketoreduction (to 6-- and 6--hydroxyoxymorphone which are subsequently glucuronidated at the 3-position). Oxymorphone and noroxymorphone are considered to be active metabolites.21,22 However, whether or not the 3-glucuronide metabolites are neurotoxic is not known. CYP450 isozyme 2D6 polymorphisms can be expected to play a similar role with respect to oxycodone as they do with codeine (see above).
In a single-dose (20 mg of controlled-release formulation) study with 28 healthy volunteers (14 young [21-45 yr] and 14 elderly [65-79 yr]), there were no significant intergroup differences in oxycodone and noroxycodone 48-hour AUC values. However, young males had a significantly higher mean 48-hour oxymorphone AUC (21.3 ng/mL/h) than those of both female age groups (young 9.9 and elderly 3.7 ng/mL/h), and elderly males (14.3 ng/mL/h) had a significantly higher AUC than that of elderly females. In the same study, the pharmacodynamic effects of a single 20-mg dose of controlled-release oxycodone were measured as a function of age. Defining drug effect as “do you feel any effects of the drug?”, the drug-effect 48-hour AUC was not altered by aging but was significantly enhanced in females versus males.35
In a recent study, single oral-dose pharmacokinetics of oxycodone 10 mg were evaluated in 40 patients following orthopedic surgery.36 Four age groups were created, each with 10 patients: 20-40 years old (A); 60-70 years old (B); 70-80 years old (C); and 80-90 years old (D). Mean oxycodone apparent oral drug clearance was 1.89, 1.59, 1.05, and 1.30 L/min in groups A to D, respectively (A vs C, P < 0.01; A vs D, P < 0.05). Thus, over the age range of this investigation, apparent oral drug clearance fell 50-80%. Corresponding mean oxycodone t1/2 was 3.7, 4.5, 5.3, and 5.7 hours (overall, P = 0.034; A vs C, P < 0.05). Corresponding mean noroxycodone t1/2 was 6.3, 7.9, 9.2, and 9.0 hours (overall, P = 0.031; A vs C and A vs D, both P < 0.05). The effects of CYP450 isozyme 2D6 polymorphisms were not altered as a function of age. Lastly, the variability in pharmacokinetic parameters was higher in older as compared with younger patients. For example, the coefficient of variation of AUC to infinity was 9% in group A and ranged from 27-37% in groups B through D.36
Unlike the case with codeine, inhibition of CYP450 isozyme 2D6 does not impair the analgesia associated with oxycodone by limiting the generation of its active metabolite, oxymorphone.37
Morphine
The onset of meaningful analgesia occurs at approximately 0.5 hours after oral administration of the IR formulation followed by peak analgesia within 1 hour. The duration of analgesia is 3-4 hours for the oral IR and 8-24 hours for the oral controlled-delivery formulations.2,21
Morphine is glucuronidated at the 3- and 6-positions, producing morphine 3- and 6-glucuronides (M-3-G and M-6-G), respectively. The 6-glucuronide is more potent as an analgesic than morphine itself, while the 3-glucuronide is active as a neurotoxin. Other metabolites include the N-demethylated product normorphine, a 3,6-diglucuronide, and a 3-ethereal sulfate. 21,38
The effect of aging on morphine pharmacokinetics has been the subject of two studies. In one study, 13 young (24-28 yr) and seven elderly (60-69 yr) subjects each received a single 10-mg/70-kg IV dose.39 Total body clearance was significantly lower in the elderly as compared with the young (means of 1.66 vs 2.02 L/h/kg; P = 0.05). Although the mean t1/2 in the elderly was almost double that in the young (9.29 vs 5.97 hr, respectively), this difference was not significant (P = 0.079). In another study, eight young (23-30 yr) and nine elderly (68-90 yr) healthy subjects each received 3 single 10-mg doses (IV, oral solution, oral ER tablet).40 After IV dosing, the mean total body clearance was reduced by 35% in the elderly as compared with young subjects (0.80 vs 1.23 L/h/kg, respectively; P = 0.01). After dosing with the oral solution, only the mean Cmax values significantly differed (elderly: 20.9 ng/mL, young: 10.8 ng/mL; P = 0.02). After dosing with the tablet, the mean morphine Cmax and AUC were significantly greater in the elderly group (8.1 ng/mL and 43.4 ng/mL/h, respectively) as compared with the young group (5.5 ng/mL [P = 0.04] and 28.0 ng/mL/h [P = 0.02], respectively).
Methadone
After single oral doses, the onset of methadone analgesia occurs at 0.5-1 hour, and duration of analgesia is 4-6 hours. However, after chronic oral dosing, the duration is prolonged to 8-24 hours.26
Methadone undergoes extensive metabolism in the gut wall and liver. Totals of nine and three metabolites can be isolated from the urine and feces, respectively. CYP450 isozymes 3A4, 1A2, and 2D6 mediate metabolism. The major metabolites are 2-ethylidene-1,5-dimethyl-3,3-diphenylpyrrolidine (EDDP; mediated via CYP450 isozyme 3A4) and pyrroline, which are both inactive pharmacologically. Methadol and normethadol are two minor active analgesic metabolites.26
Unlike morphine and selected other opioids, methadone metabolism is greatly affected by genetic (via CYP450 isozyme 2D6) and environmental influences (eg, latter via smoking, concurrent use of enzyme inducers/inhibitors).19,26,41
In a retrospective study using data collected from 186 patients with cancer being treated with methadone, factors related to the high interpatient variability in the total body clearance of the drug were assessed. The mean clearance was 186 mL/min, but the range was broad (-23 to 2100 mL/min). Univariate risk factors for increased clearance included concurrent use of phenytoin, spironolactone, verapamil, and estrogens (primarily, diethylstilbestrol). Univariate risk factors for decreased clearance included concurrent use of amitriptyline, presence of certain cancer types, and an age of 65 years or older. Unfortunately, the factors taken together explained only 40% of the variability in total body clearance. Multivariate analysis, which could allow confounding univariate variables to be eliminated, was not performed.42
Tramadol
Tramadol is not a pure opioid receptor agonist. It is a dual mechanism (mu-opioid receptor agonist plus norepinephrine-serotonin reuptake inhibitor) compound.43 As such, it has a complex molecular basis for its analgesia. It is metabolized to an active O-desmethyl compound. Both the parent compound and the active metabolite exist as optically-active enantiomers (ie, as (-)- and (+)-enantiomers, which can differ in their receptor binding and activity characteristics). Both enantiomers of the parent compound and the active metabolite are involved in analgesia. For example, norepinephrine and serotonin reuptake inhibition are primarily associated with (-)- tramadol and (+)- tramadol, respectively. Mu-opioid receptor agonism is primarily associated with (+)- O-desmethyltramadol and, to a lesser extent, with (+)- tramadol. The relative contributions of these different mechanisms of action to the overall effect will vary over time since, as the parent compound is metabolized, the contribution of norepinephrine/serotonin reuptake inhibition will decline while that of mu-opioid receptor agonism will rise. The result is a complex time- and metabolism-dependent pattern of pharmacologic activities.44,45
After single oral doses of the IR product, peak analgesia is achieved at 2-3 hours after administration.43,46,47 Tramadol is extensively metabolized via O-demethylation (catalyzed by CYP450 isozyme 2D6), N-demethylation (catalyzed by CYP450 isozymes 3A4 and 2B6), and glucuronidation and sulfation of tramadol and the two demethylated metabolites.43,46-48 Only the O-desmethyltramadol metabolite is active as an analgesic. Thirty percent of urinary excretion is as the unchanged parent compound and 70% as metabolites.43,46-48
Another complicating factor is the polymorphic metabolism via CYP450 isozyme 2D6, which results in generation of O-desmethyltramadol. As discussed previously, the majority of the population are extensive (or normal) metabolizers while a minority are PMs. Being a PM results in elevated tramadol and reduced O-desmethyltramadol serum concentrations similar to those seen when a CYP450 isozyme 2D6 inhibitor is co-ingested. This situation becomes even more complicated if a PM individual is also co-ingesting a CYP450 isozyme 2D6 inhibitor. These individuals frequently have suboptimal analgesia, even if the dose is escalated above recommended limits. As mentioned above, another category, the UM has been discovered. Being a UM results in reduced tramadol and increased O-desmethyltramadol serum concentrations similar to those seen when a potent CYP450 enzyme inducer is co-ingested. Again, a UM individual co-ingesting a CYP450 enzyme inducer becomes even more complicated. In fact, UM individuals are at increased risk of severe opioid intoxication, including fatal respiratory depression, because they generate unusually large amounts of the active metabolite.49-53
Few data are available regarding the effect of aging on the pharmacokinetics of tramadol. Elderly persons over 75 years of age have modest increases in mean tramadol Cmax and mean tramadol Tmax as compared with those of younger individuals (for 50 mg IR orally x 1 dose, 208 vs 154 ng/mL and 1.9 vs 1.6 hr, respectively; no statistical testing done).43 In subjects with unspecified degrees of hepatic impairment receiving a single 50-mg IR dose orally as compared with healthy volunteers, the mean tramadol Cmax was increased (from 154 to 217 ng/mL), the mean tramadol Tmax was increased (from 1.6 to 1.9 hr), the tramadol t1/2 was increased (from 5.6-6.7 to 13.3 hr), and the O-desmethyltramadol t1/2 was increased (from 6.7-7 to 18.5 hr; no statistical testing done).43 Renal impairment also produces increases in mean t1/2 for tramadol and the active metabolite (for creatinine clearances < 30 mL/min, 5.6-6.7 to 10.6 hr for tramadol and 6.7-7 to 11.5 hr for the metabolite; for creatinine clearances < 5 mL/min, 5.6-6.7 to 11 hr for tramadol and 6.7-7 to 16.9 hr for the metabolite).43
Tapentadol
Tapentadol has the same mechanism of analgesic activity as does tramadol. However, its pattern of pharmacologic activities is simplified by an absence of enantiomeric forms, one or more active metabolites, and polymorphic drug metabolism (CYP450 isozyme 2D6).54,55
Tapentadol has an onset of analgesia and peak analgesia at means of 1-1.5 and 3 hours after ingestion, respectively.56 It is 97% metabolized, with 3% being renally excreted as parent compound.57 Metabolism is primarily via glucuronidation (55%) and sulfation (14%).57 Oxidation occurs to a lesser extent (13% being via N-demethylation mediated by CYP450 isozymes 2C19 and 2C9; 2% being via hydroxylation mediated by CYP450 isozyme 2D6).57 Both of the latter metabolites undergo glucuronidation.57
Tapentadol pharmacokinetics are similar in elderly persons as compared with younger individuals, except for a mean reduction in Cmax of 16% in the elderly.54 Mean tapentadol glucuronide serum concentrations rise in mild, moderate, and severe renal impairment by 1.5-, 2.5-, and 5.5-fold, respectively. The clinical relevance of this is unknown.54 Mean tapentadol serum concentrations rise 1.7- and 4.2-fold in mild (Child-Pugh class A) and moderate (Child-Pugh class B) hepatic impairment, respectively.54 Corresponding fold-increases in t1/2 are 1.2 and 1.4.54 In addition, the rate of formation of tapentadol glucuronide is reduced. There are no data available from individuals with severe renal or hepatic (Child-Pugh class C) impairment.
Inhibitors of glucuronidation may have clinically-important effects on serum tapentadol concentrations. For example, probenecid increases tapentadol serum concentrations by a mean of 57%.54 There are no data regarding the effect of more potent inhibitors of glucuronidation such as valproate and fluconazole, or inducers of glucuronidation (eg, carbamazepine, rifampin, estrogens).58
Conclusion
The opioids have been utilized for their analgesic properties for thousands of years. Today, these agents are among the most effective analgesics available for the treatment of moderate-to-severe acute and chronic pain of virtually all etiologies. However, their use in older individuals has been linked to an elevated risk of AEs as compared with younger individuals, making patients and prescribers reticent to use them. In most individuals, it is possible to reduce the AE risk and to maximize the therapeutic potential by learning how to use a small number of agents well. In most cases, tolerance develops to opioid AEs over a reasonably short period of time, and patients can be supported over this period with nonpharmacologic and pharmacologic measures. Pre-emptive stimulant laxative therapy is almost always successful in preventing the development of constipation, an AE where tolerance does not develop. Although few elder-specific data are available, there are adequate data upon which opioid dosing recommendations in the elderly, and in those with compromised renal or hepatic disease (based on data in Table IV),2,21,22,59 have been formulated. In addition, relatively easy methods for switching from one opioid to another, including TD fentanyl and methadone, are available to clinicians. In a few specific situations, one opioid may be preferred over others. However, in most patients, several opioids can be utilized, and the selection process becomes largely one of choosing an agent with which the prescriber has extensive experience.

The author reports no relevant financial relationships.
Dr. Guay is Professor of Experimental & Clinical Pharmacology, College of Pharmacy, University of Minnesota, and Consultant, HealthPartners Inc., Minneapolis. 1. Vadalouca A, Moka E, Argyra E, et al. Opioid rotation in patients with cancer: A review of the current literature. J Opioid Manage 2008;4:213-250.
2. Facts and comparisons. Wolters Kluwer Health Website. www.factsandcomparisons.com/online-products.aspx. Accessed February 16, 2010.
3. Breitbart W, Chandler S, Eagel B, et al. An alternative algorithm for dosing transdermal fentanyl for cancer-related pain. Oncology (Williston Park) 2000;14:695-705, 709-719.
4. Hagen NA, Biondo P, Stiles C. Assessment and management of breakthrough pain in cancer patients: Current approaches and emerging research. Curr Pain Headache Rep 2008;12:241-248.
5. William L, MacLeod R. Management of breakthrough pain in patients with cancer. Drugs 2008;68:913-924.
6. Peppin JF. The use of methadone “as needed,” it is justified? J Opioid Manage 2009;5:7-9.
7. Christie JM, Simmonds M, Patt R, et al. Dose-titration, multicenter study of oral transmucosal fentanyl citrate for the treatment of breakthrough pain in cancer patients using transdermal fentanyl for persistent pain. J Clin Oncol 1998;16:3238-3245.
8. Onsolis™ (fentanyl buccal soluble film) [packaging insert]. Somerset, NJ: Meda Pharmaceuticals; 2009.
9. Paalzow L, Nilsson L, Stenberg P. Pharmacokinetic basis for optimal methadone treatment of pain in cancer patients. Acta Anaesthesiol Scand Suppl 1982;74:55-58.
10. Inturrisi CE, Colburn WA, Kaiko RF, et al. Pharmacokinetics and pharmacodynamics of methadone in patients with chronic pain. Clin Pharmacol Ther 1987;41:392-401.
11. Bruera M, Palmer JL, Bosnjak S, et al. Methadone versus morphine as a first-line strong opioid for cancer pain: A randomized, double-blind study. J Clin Oncol 2004;22:185-192.
12. Hays L, Reid C, Doran M, Geary K. Use of methadone for the treatment of diabetic neuropathy. Diabetes Care 2005;28:485-487.
13. González-Barboteo J, Porta-Sales J, Sánchez D, et al. Conversion from parenteral to oral methadone. J Pain Palliat Care Pharmacother 2008;22:200-205.
14. Weschules DJ, Bain KT. A systematic review of opioid conversion ratios used with methadone for the treatment of pain. Pain Med 2008;9:595-612. Published Online: June 28, 2008.
15. Mercadante S, Ferrera P, Villari P, Casuccio A. Rapid switching between transdermal fentanyl and methadone in cancer patients. J Clin Oncol 2005;23:5229-5234.
16. Walker PW, Palla S, Pei BL, et al. Switching from methadone to a different opioid: What is the equianalgesic dose ratio? J Palliat Med 2008;11:1103-1108.
17. Reynolds KK, Ramey-Hartung B, Jortani SA. The value of CYP2D6 and OPRM1 pharmacogenetic testing for opioid therapy. Clin Lab Med 2008;28:581-598.
18. Kasai S, Hayashida M, Sora I, Ikeda K. Candidate gene polymorphisms predicting individual sensitivity to opioids. Naunyn Schmiedebergs Arch Pharmacol 2008;377:269-281. Published Online: November 13, 2007.
19. Li Y, Kantelip JP, Gerritsen-van Schieveen P, Davani S. Interindividual variability of methadone response: Impact of genetic polymorphism. Mol Drug Ther 2008;12:109-124.
20. Hayashida M, Nagashima M, Satoh Y, et al. Analgesic requirements after major abdominal surgery are associated with OPRM1 gene polymorphism genotype and haplotype. Pharmacogenomics 2008;9:1605-1616.
21. 2009 AHFS Drug Information. American Society of Health-System Pharmacists, Bethesda, MD. www.ahfsdruginformation.com. Accessed February 16, 2010.
22. Coller JK, Cristrup LL, Somogyi AA. Role of active metabolites in the use of opioids. Eur J Clin Pharmacol 2009;65:121-139. Published Online: October 29, 2008.
23. Chen ZR, Somogyi AA, Reynolds G, Bochner F. Disposition and metabolism of codeine after single and chronic doses in one poor and seven extensive metabolizers. Br J Clin Pharmacol 1991;31:381-390.
24. Drug interactions. http://medicine.iupui.edu/clinpharm/DDIs/. Accessed February 12, 2010.
25. Stamer UM, Stüber F, Muders T, Musshoff F. Respiratory depression with tramadol in a patient with renal impairment and CYP2D6 gene duplication. Anesth Analg 2008;107:926-929.
26. Guay DR. Methadone for persistent pain in the older patient. Aging Health 2006;2:313-324.
27. Mather LE. Clinical pharmacokinetics of fentanyl and its newer derivatives. Clin Pharmacokinet 1983;8:422-446.
28. Esteve M, Levron JC, Flaisler B, et al. Does aging modify pharmacokinetics of transdermal fentanyl? Anesthesiology 1991;75:A705.
29. Bentley JB, Botel JD, Nenad RE Jr, Gillespie TJ. Age and fentanyl pharmacokinetics. Anesth Analg 1982;61:968-971.
30. Kharasch ED, Hoffer C, Whittington D. Influence of age on the pharmacokinetics and pharmacodynamics of oral transmucosal fentanyl citrate. Anesthesiology 2004;101:738-743.
31. Hutchinson MR, Menelaou A, Foster DJR, et al. CYP2D6 and CYP3A4 involvement in the primary oxidative metabolism of hydrocodone by human liver microsomes. Br J Clin Pharmacol 2004;57:287-297.
32. Dixon R, Crews T, Inturrisi C, Foley K. Levorphanol: Pharmacokinetics and steady-state plasma concentrations in patients with pain. Res Commun Chem Pathol Pharmacol 1983;41:3-17.
33. Guay DR. Use of oral oxymorphone in the elderly. Consult Pharm 2007;22:417-430.
34. Adams MP, Ahdieh H. Pharmacokinetics and dose-proportionality of oxymorphone extended release and its metabolites: results of a randomized crossover study. Pharmacotherapy 2004;24:468-476.
35. Kaiko RF, Benziger DP, Fitzmartin RD, et al. Pharmacokinetic-pharmacodynamic relationships of controlled-release oxycodone. Clin Pharmacol The 1996;59:52-61.
36. Liukas A, Kuusniemi K, Aantaa R, et al. Plasma concentrations of oral oxycodone are greatly increased in the elderly. Clin Pharmacol Ther 2008;84:462-467.
37. Guay DR. Opioid analgesics for persistent pain in the older patient. Aging Health 2006;2:669-690.
38. Lugo RA, Kern SE. Clinical pharmacokinetics of morphine. J Pain Palliat Care Pharmacother 2002;16:5-18.
39. Owen JA, Sitar DS, Berger L, et al. Age-related morphine kinetics. Clin Pharmacol Ther 1983;34:364-368.
40. Baillie SP, Bateman DN, Coates PE, Woodhouse KW. Age and the pharmacokinetics of morphine. Age Ageing 1989;18:258-262.
41. Shiran MR, Lennard MS, Iqbal MZ, et al. Contribution of the activities of CYP3A, CYP2D6, CYP1A2 and other potential covariates to the disposition of methadone in patients undergoing methadone maintenance treatment. Br J Clin Pharmacol 2009;67:29-37.
42. Plummer JL, Gourlay GK, Cherry DA, Cousins MJ. Estimation of methadone clearance: Application in the management of cancer pain. Pain 1988;33:313-322.
43. Ultram® (tramadol hydrochloride) tablets [package insert]. Raritan, NJ: Ortho-McNeil Pharmaceutical, Inc.; 2007.
44. Raffa RB, Friderichs E, Reimann W, et al. Complementary and synergistic antinociceptive interaction between the enantiomers of tramadol. 1993;267:331-340.
45. Frink MC, Hennies HH, Englberger W, et al. Influence of tramadol on neurotransmitter systems of the rat brain. Arzneimittelforschung 1996;46:1029-1036.
46. Ardakani YH, Rouini MR. Pharmacokinetics of tramadol and its three main metabolites in healthy male and female volunteers. Biopharm Drug Dispos 2007;28:527-534.
47. García Quetglas E, Azanza JR, Cardenas E, et al. Stereoselective pharmacokinetic analysis of tramadol and its main phase I metabolites in healthy subjects after intravenous and oral administration of racemic tramadol. Biopharm Drug Dispos 2007;28:19-33.
48. Lintz W, Erlacin S, Frankus E, Uragg H. Biotransformation of tramadol in man and animal [in German]. Arzneimittelforschung 1981;31:1932-1943.
49. Poulsen L, Arendt-Nielsen L, Brøsen K, Sindrup SH. The hypoalgesic effect of tramadol in relation to CYP2D6. Clin Pharmacol Ther 1996;60:636-644.
50. Halling J, Weihe P, Brøsen K. CYP2D6 polymorphism in relation to tramadol metabolism: A study of Faroese patients. 2008;30:271-275.
51. Kirchheiner J, Keulen JT, Bauer S, et al. Effects of the CYP2D6 gene duplication on the pharmacokinetics and pharmacodynamics of tramadol. ,i>J Clin Psychopharmacol 2008;28:78-83.
52. Stamer UM, Musshoff F, Kobilay M, et al. Concentrations of tramadol and O-desmethyltramadol enantiomers in different CYP2D6 genotypes. Clin Pharmacol Ther 2007;82:41-47. Published Online: March 14, 2007.
53. Enggaard TP, Poulsen L, Arendt-Nielsen L, et al. The analgesic effect of tramadol after intravenous injection in healthy volunteers in relation to CYP2D6. Anesth Analg 2006;102:146-150.
54. Nucynta™ (tapentado immediate-release oral) tablets [package insert]. Raritan, NJ: PriCara, division of Ortho-McNeil-Janssen Pharmaceuticals, Inc.; 2009.
55. Guay DRP. Is tapentadol an advance on tramadol? Consult Pharm 2009;24(11):833-840. 56. Kleinert R, Lange C, Steup A, et al. Single dose analgesic efficacy of tapentadol in postsurgical dental pain: The results of a randomized, double-blind, placebo-controlled study. Anesth Analg 2008;107:2048-2055.
57. Terlinden R, Ossig J, Fliegert F, et al. Absorption, metabolism, and excretion of 14C-labeled tapentadol HCl in healthy male subjects. Eur J Drug Metab Pharmacokinet 2007;32:163-169.
58. Kiang TK, Ensom MH, Chang TK. UDP-glucuronosyltransferases and clinical drug-drug interactions. Pharmacol Ther 2005;106:97-132. Published Online: January 12, 2005.
59. Davison SN, Mayo PR. Pain management in chronic kidney disease: The pharmacokinetics and pharmacodynamics of hydromorphone and hydromorphone-3-glucuronide in hemodialysis patients. J Opioid Manage 2008;4:335-336, 339-344.


