Is It My Chicken?
HISTORY
A 69-year-old Mexican-American female with past medical history significant for hypertension, rheumatoid arthritis, fibromyalgia, and irritable bowel syndrome presented to the emergency room with the acute onset of right hip pain. She was performing her daily house chores, when the pain insidiously started. She could not bear weight while standing due to the intensity of the pain, thus limiting her gait and prompting her emergency room (ER) visit. In addition, she reported subjective fevers at home, which were later confirmed during her hospital admission, but denied any sick contacts, chills, night sweats, trauma, history of falls, dysuria, hematuria, urgency, frequency, hemoptysis, hematochezia, nausea, vomiting, paresthesia, sensory loss, or recent weight loss/gain.
She also denied any recent travel history or having any pets including exposure to reptiles. She lived at home with her husband and son and prior to this episode had been able to perform all her daily activities of living without any problems. She denied having any hemoglobinopathies or a family history of such. Her medications at home included lopressor 25 mg orally twice daily, mobic 15 mg orally once daily, hydroxychloroquine 200 mg orally twice daily, esomeprazole 40 mg orally once daily, hydrochlorothiazide 25 mg orally once daily, fluticasone 2 puffs twice daily, certrizine 10 mg orally once daily, aspirin 81 mg orally once daily, and etanercept 50 mg/ml injection once weekly.
PHYSICAL EXAMINATION
On physical exam, she had marked tenderness to palpation of her right groin directly over her pubic symphisis, but no visible lesion, rashes, masses, or lymph nodes were appreciated. She had normal passive range of motion of her lower extremity but decreased active range of motion of the lower extremity limited by pain on hip flexion, internal and external rotation. Sensory examination was intact to light touch throughout upper and lower extremity bilaterally. The patient's strength was noted to be 4 out of 5 in the lower extremity limited by her pain, but otherwise nonremarkable. Heberden's nodes were palpated on multiple distal interphalangeal joints bilaterally and no evidence of synovitis. She had no vaginal discharge or lesions and her bimanual exam was unimpressive. A gait exam was not performed due her extensive pain on standing. The rest of her physical exam was unremarkable.
LABORATORY TESTS
Her initial labs studies showed a white blood count 11.1, hemoglobin 11.6 g/dl, hematocrit 34.7% (MCV 96) and platelet count of 256. Her sodium was 137 mmol/L, potassium 3.6 mmol/L, chloride 101 mmol/L, bicarbonate 26 mmol/L, blood urea nitrogen 23.5 mg/dL, creatinine 0.85 mg/dL and glucose of 83 mg/dL. Her lactate level was 0.8 mmol/L, calcium 7.9 mmol/L, magnesium 1.9 mmol/L, phosphate 2.7 mmol/L, albumin 7.9 g/dL, alkaline phosphatase 4.1 ug/ml, aspartate aminotransferase 31 ug/ml and alanine aminotransferase 19 IU/L. Urine analysis was unremarkable. Her initial C-reactive protein was reported at 22.4. In addition, brucella serologies were reported as <1:10, HIV panel was negative, and a thyroid-stimulating hormone was reported as 1.190 uIU/mL.
 DIAGNOSIS
DIAGNOSIS
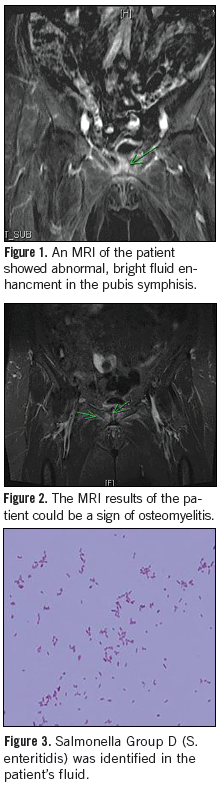
In the ER, a bilateral hip x-ray showed no lytic lesions or evidence of avascular necrosis. In addition a CT abdomen/pelvis showed no intra-abdominal process that would account for the patient’s symptoms. During her admission, a pelvic ultrasound showed no sonographic evidence of pelvic pathology. An MRI was ordered to further investigate her symptoms, which showed an abnormal bright fluid enhancement within the pubis symphisis worrisome for osteomyelitis (Figures 1 and 2). Multiple blood cultures drawn during her hospital admission failed to grow any organisms. She was subsequently started on empiric antibiotics including levofloxacin 500 mg, orally once daily, as well as vancomycin, 1 g intravenously every 12 hours.
To better guide antibiotic therapy, a CT guided pelvic bone biopsy and fine needle aspiration of the fluid accumulated around the pubic symphysis was performed. Acid-fast bacillus stain was negative. Cytology of the fluid aspirate was negative for malignant cells, but grew gram negative rods that were eventually identified as Salmonella Group D (S. enteritidis) (Figure 3).
DISCUSSION
Salmonella are nonspore forming, gram negative rods. Over 1800 serotypes have been isolated and subdivided into 6groups: A, B, C1, C2, D, and E. Numerous hosts exist including poultry, pigs, cows, various pets (reptiles too) and humans. Transmission occurs through ingestion of contaminated food or water, or by direct inoculation.1-4
Salmonella infections, including osteomyelitis, which is rare and accounts for approximately <1% of all salmonella infections,1,4,5 are usually seen in association with sickle cell disease. This is possibly due to the microscopic bowel infarcts allowing salmonella passage into the blood stream.1,2 Other risk factors include autoimmune disease such as lupus and rheumatoid arthritis, HIV infections, diabetes, hematologic neoplasms, cirrhosis of the liver, other hemoglobinopathies, and the use of immunosuppressive therapies most notably the tumor necrosis factor alpha (TNF-alpha) antagonists.3-7
Our patient had been using etanercept for over 1 year for her rheumatoid arthritis. Etanercept is a recombinant protein that is identical to a portion of the TNF-alpha receptor, hence it acts as a decoy binding TNF-alpha before it reaches its receptors.2,7 TNF-alpha plays an essential role in the immune mediated response to infection via toll like receptors (TLR) and the activation of cytokines such as interferon-gamma, interleukin-12, and phagocytes. TNF-alpha is also essential for the formation and maintenance of granulomas, which is a key component of host defense against intracellular pathogens.8,9 TNF-alpha blockade leads to a greater adherence of salmonella to the intestinal wall, with a decline of the TLR-4, dendritic phagocytic cells, decreased production of cytokines, less granulomas formation and maintenance, hence causing an impaired immune response to salmonella species resulting in invasive infections.7-9 The above is the most probable explanation of how our patient developed osteomyelitis.
Interestingly enough, infliximab compared to the other 2 TNF-alpha antagonist (entanercept and adalimumab), is associated with a higher risk of infection. Infliximab, seems to have a much higher affinity for TNF-alpha and to induce apoptosis of monocytes and T cells. It also has a longer half-life; greater than 2 months post-infusion.7,10
MANAGEMENT
CRP titers are useful markers in assisting with the progression and resolution of the disease. Usually, relief of symptoms is accompanied by a decrease in CRP titers as was seen in the case with our patient.4,6
Various antibiotics can be used in the setting of salmonella infections including fluoroquinolones, trimethroprim-sulfamethaxozole, ampicillin, or third-generation cephalosporins. Due to resistance, fluoroquinolones and third -generation cephalosporins are usually chosen if the susceptibilities are unknown.3
Our patient was initially empirically started on intravenous vancomycin and oral levofloxacin. The vancomycin was stopped after identification of the bacteria and levofloxacin was continued during her hospital stay. She was discharged on ciprofloxacin for a total of 6 weeks as per direction from our infectious disease colleagues. No surgical intervention was deemed necessary. Upon discharge, our patient's CRP was 4.6 (1.2 mg/dL 1-month post-discharge) and she was able to ambulate with a walker and bear weight on her affected lower extremity. She opted not to use etanercept in the future.
Joseph My, DO, Dept. of Internal Medicine, San Antonio Military Medical Center (SAMMC – North)
Irfan Haider, MS3, San Antonio, Ft. Sam Houston, TX.
Sayed K. Ali, MD, Faculty, South Texas Veterans Health Care System, San Antonio, TXFaculty, University of Texas Health Science Center, San Antonio TX.
References:
1. Sanchez AA, Mazurek MT, Clapper MF. Salmonella osteomyelitis presenting as fibrous dsyplasia. Clin Orthop Relat Res. 1996;(330):185-189.
2. Nowinski RJ, Albert MC. Salmonella osteomyelitis secondary to iguana exposure. Clin Orthop Relat Res. 2000;(372):250-253.
3. Hohmann EL. Non-thyphoidal salmonellosis. Clin Infect Dis. 2001;32(2):263-269.
4. Chang IC. Salmonella spondylodiscitis in patient without sickle cell disease. Clin Orthop and Relat Res. 2005;(430):243-247.
5. Gupta SK, Pandit A, White DG, Evans PD. Salmonella osteomyelitis of the thoracic spine, an unusual presentation. Postgrad Med J. 2004;80(940):110-111.
6. VanCappelle HG, Veenedaal D, deVogel PL. Salmonella panama osteomyelitis in an otherwise healthy patient. Clin Orthop Relat Res. 1995;(321):235-238.
7. Crum NF, Lederman ER, Wallace MR. Infections associated with tumor necrosis factor-alpha antagonists.Medicine (Baltimore). 2005;84(5):291-302.
8. Rijkeboer A, Voskuyl A, Van Agtmael M. Fatal Salmonella enteritidis septicemia in a rheumatoid arthritis patient with TNF-alpha antagonist. Scand J Infect Dis. 2007;39(1):80-83.
9. Netea MG, Radstake T, Joosten LA, et al. Salmonella septicemia in rheumatoid arthritis patient receiving anti-tumor necrosis factor therapy. Arthritis Rhem. 2003;48(7):1853-1857.
10. Salliot C, Gossec L, Ruyssen-Witrand A, et al. Infection during TNF-alpha blocker therapy for rheumatic disease in daily practice: a systematic retrospective study of 709 patients. Rheumatology (Oxford). 2007;46(2):327-334.


