Diagnosis and Treatment of Chronic Orthostatic Hypotension
This article is the second in a continuing series on cardiovascular issues in the older adult. The first article in the series, “Aortic Stenosis: A Focused Review on the Elderly,” was published in the March issue of Clinical Geriatrics. The remaining articles in the series, to be published in future issues of the Journal, will discuss such topics as atrial fibrillation, heart failure, peripheral arterial disease, hypertension, and devices for heart rhythm disorders.
_______________________________________________________________________________________________
A significant drop in blood pressure when standing up from a seated or lying position is known as orthostatic or postural hypotension. This can occur acutely with severe dehydration or blood loss, which is usually overt. Chronic orthostatic hypotension becomes relatively common with aging and the presence of frailty, but it can present insidiously and atypically. Undiagnosed or poorly treated orthostatic hypotension can contribute significantly to debility and mobility problems. The following cases illustrate how patient function can be adversely affected when orthostatic hypotension is not properly detected and treated.
Case 1
Mr. H was a 74-year-old man who received a diagnosis of orthostatic hypotension 5 years earlier by a neurologist. At that time, he was started on fludrocortisone and was instructed to use a wedge pillow while sleeping. The patient was functional in activities and instrumental activities of daily living, was active, and was only mildly symptomatic over the following 5 years. Mr. H then underwent urologic surgery for bladder neck stricture that required a period of postoperative bed rest. Shortly after his period of bed rest, he fell and developed a subdural hematoma. The patient spent a total of almost 2 months convalescing in a rehabilitation facility after his urologic surgery due to his subdural hematoma and other medical complications. During his recovery, midodrine was added to his treatment regimen for worsening orthostatic hypotension. Four months after his urologic surgery, the patient still could only stand for 20 seconds at a time, which made rehabilitation problematic, so he was discharged from therapy by his physical therapist. Pyridostigmine was then added to his treatment regimen by his neurologist, but he remained wheelchair-bound due to light-headedness. Two weeks after pyridostigmine was started, Mr. H was admitted to a geriatric evaluation and management unit because of persisting light-headedness. His lying systolic blood pressure was 157 mm Hg, which fell to 88 mm Hg after 3 minutes of standing. On inquiry about his use of the wedge pillow, he stated that he had used it nightly for 5 years to elevate his legs to reduce edema and that he did not know that the pillow was intended to elevate his head. Over the next month, the patient was treated with elevation of the head of his hospital bed to 20 degrees and was continued on midodrine and pyridostigmine. Fludrocortisone was stopped due to worsening edema. He gradually resumed ambulation of household distances, and he especially benefitted from aquatic physical therapy, as the chest-high water prevented hypotension and permitted extended periods of mobility. After 6 weeks, he was discharged from the geriatric evaluation and management unit and was continued on midodrine and pyridostigmine.
Case 2
Mr. J was a 77-year-old man with diabetic neuropathy, hypertension, and nocturia, who was admitted to the hospital for episodic leg weakness. His medications included furosemide, doxazosin, and nortriptyline. The patient was found to have symptomatic orthostatic hypotension, which improved after the furosemide was stopped. Two years after he was discharged, he returned to the emergency department because of episodes of near-syncope, during which he became quite pale. The emergency department physician’s note stated “no orthostatic blood pressure changes,” but it did not document values or how this finding was obtained. Mr. J was sent home, but he was readmitted 3 weeks later with severe dizziness. Midodrine was added to his treatment regimen, and he was transferred to a geriatric evaluation and management unit. At transfer, the patient’s lying systolic blood pressure was 144 mm Hg, which fell to 75 mm Hg after 3 minutes of standing. Two of his chronic medications, doxazosin and nortriptyline, were stopped and the head of his hospital bed was elevated to 20 degrees. Mr. J’s light-headedness resolved, and within 1 year, the midodrine was stopped without recurrence of his symptoms.
Physiological Features of Postural Blood Pressure Changes
Normally, when the body moves from lying to standing, there is an immediate brief drop in systemic vascular resistance and blood pressure. Vascular resistance increases above baseline level within a few seconds of standing, and blood pressure is normalized within 15 seconds of standing. This transient fall in blood pressure does not increase with age. Indeed, an exaggeration of this transient initial orthostatic hypotension occurs most frequently in otherwise healthy young subjects and can only be detected with equipment to monitor continuous beat-to-beat blood pressures.1 The remainder of this article will discuss typical orthostatic hypotension, which occurs more slowly and increases in prevalence with aging.
With standing, a gradual pooling of blood in the legs and splanchnic bed occurs. The baroreceptor reflex compensates largely through increased systemic vascular resistance. Both aging and chronic hypertension diminish postural compensation through a reduction in baroreceptor sensitivity and arterial compliance.2 As a consequence, supine hypertension is a major risk factor for orthostatic hypotension. In addition, there is an attenuation of alpha-1 vasoconstrictor responsiveness to sympathetic stimulation with aging.3 Bed rest, which often occurs with infirmity, accentuates orthostasis, as 1 week of bed rest causes plasma volume to decrease 300 to 500 mL.4
The effect of chronic hypertension on cerebral autoregulation also contributes to symptoms of orthostatic hypotension. Under normal conditions, autoregulation maintains stable cerebral perfusion down to a mean arterial pressure of 60 mm Hg.5 With chronic hypertension, there is an upward shift of the lower limit of autoregulation, which contributes to impaired tolerance of postural declines in blood pressure. This upward shift is reduced with the treatment of hypertension, normalizing cerebral autoregulation.5
Symptoms and Diagnosis of Orthostatic Hypotension
Symptoms of orthostatic hypotension are variable in character and timing. Some patients describe light-headedness or near-syncope, and many describe nonspecific symptoms such as paroxysmal severe fatigue, generalized weakness, or the urgent need to sit down after a period of standing. At my institution, we had a 62-year-old patient with diabetes who was recovering from below-the-knee amputation whose systolic blood pressure dropped from 123 mm Hg while lying to 71 mm Hg after standing for 3 minutes. Upon standing, he informed the nurse that he needed to sit down immediately, but he denied feeling light-headed. My institution has had numerous previously undiagnosed patients who were found on prompt measurement to be quite hypotensive after they “gave out” after walking a few minutes between the parallel bars during physical therapy and asked urgently to sit down.
Orthostatic hypotension can cause falling and syncope. An assessment of elderly fallers in a long-term residential care facility found that orthostatic hypotension was the primary cause of falling in nearly 16% of persons in the intervention group and a possible contributing factor in an additional 26% of persons in the intervention group.6 A review of 2106 patients age 65 years or older who were admitted to a teaching hospital after syncope determined that orthostatic hypotension was the cause in 13%, yet postural blood pressure recording was performed in only 38% of subjects.7 This test had the highest yield for determining the etiology of the syncopal episode, whereas cardiac enzyme tests, head computed tomography scans, electroencephalography, and carotid ultrasonography had the lowest yield.
Measurements for orthostatic hypotension are obtained during 3 minutes of quiet standing,8 which is preceded by measurements in the recumbent position. Patients should preferably be lying for 5 minutes before blood pressure is measured. Two-thirds of patients with orthostatic hypotension may go undetected if the maneuver is performed from sitting-to-standing positions.9 Some studies recommend measuring blood pressure after 1 minute as well as 3 minutes of standing, as hypotension was somewhat more common after 1 minute of standing and the 1-minute decline in systolic pressure was more sensitive in predicting risk of subsequent falls.10 Orthostatic hypotension is most prevalent in the morning when a person first arises.11 In addition to within-day variability, there is variable day-to-day reproducibility, so clinicians should perform postural measurements several times in symptomatic patients before excluding the diagnosis of orthostatic hypotension.12
By consensus, orthostatic hypotension is indicated when there is a reduction of systolic blood pressure of at least 20 mm Hg or diastolic blood pressure of at least 10 mm Hg upon standing.8 Many clinicians, however, feel that symptomatic orthostasis usually results from a reduction in systolic pressure of at least 40 mm Hg, with the standing mean pressure falling at or below the cerebral autoregulation limit of 60 mm Hg (usually a standing systolic blood pressure of ≤90 mm Hg). Postural cardioacceleration in the absence of hypotension strongly suggests hypovolemia.13
In patients with orthostatic hypotension, the time to maximal drop in blood pressure is variable. As previously stated, initial orthostatic hypotension occurs within seconds of standing, whereas typical orthostatic hypotension manifests within 1 to 3 minutes. Symptomatic hypotension delayed up to 30 minutes after standing has been described.14 Gibbons and Freeman15 reported that, among 108 patients with orthostatic hypotension on tilt table testing, 46% had orthostatic hypotension occurring within 3 minutes of tilt table testing, 15% occurring between 3 and 10 minutes, and 39% occurring after 10 minutes.
Causes of Chronic Orthostatic Hypotension
In addition to bed rest and volume depletion as described previously, other frequent causes of orthostatic hypotension include medications and autonomic dysfunction. Medications that produce vasodilation have the greatest association with orthostatic hypotension. Those that most commonly cause postural hypotension include alpha-blockers, long-acting nitrates, tricyclic antidepressants, phenothiazines, dopaminergic agents, and hydralazine. Chronic antihypertensive therapy, including thiazide diuretics, is only rarely associated with orthostatic hypotension.16 Acute volume depletion from loop diuretics, however, can exacerbate orthostasis. In general, lowering blood pressure appropriately with medications decreases the prevalence of orthostatic hypotension in elderly patients with hypertension.17 Angiotensin-converting enzyme inhibitors in particular may improve baroreceptor sensitivity through suppression of sympathetic activity and may attenuate orthostatic hypotension.18
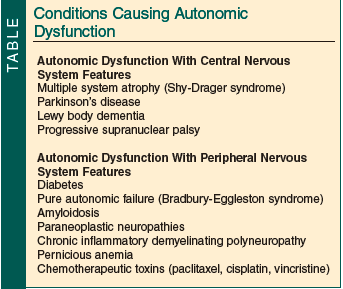
Conditions causing autonomic dysfunction that may be associated with orthostatic hypotension are broken down into those with central nervous system features and those with peripheral nervous system features (Table). Most of these conditions are more prevalent with aging, although pure autonomic failure should be suspected in young or middle-aged patients with orthostasis in the absence of volume depletion. Clinicians should have a high index of suspicion for orthostatic hypotension in patients who have one of these diagnoses if they are falling or feeling profoundly weak.
Treatment of Orthostatic Hypotension
If symptomatic orthostasis persists after discontinuation of exacerbating medications and assurance of volume repletion, the clinician should institute additional measures. It is sometimes advisable to practice permissive hypertension, reducing antihypertensive medications and accepting some supine hypertension in the patient to maintain postural tolerance. Raising the head of the bed 6 inches or to approximately 20 degrees results in improved orthostatic tolerance.19 This decreases nocturnal diuresis and enhances cerebral autoregulation by reducing supine hypertension. A small, short-term study found that waist-high compression hosiery garments with 20 to 30 mm Hg compression reduced orthostatic hypotension and frequently abolished orthostatic dizziness in elderly patients.20 Whether shorter garments are effective is unclear, although another small study of water immersion for patients with orthostatic hypotension demonstrated persistent hypotension with standing immersion to the upper thigh but abolishment of hypotension with standing immersion to the midabdomen.21 These findings are not unexpected, as patients with orthostatic hypotension have pooling of blood in the splanchnic circulation and not just in the legs.
Sometimes nonpharmacologic measures for the treatment of orthostatic hypotension are insufficient. Fludrocortisone treatment for orthostatic hypotension lacks large randomized trials, but in small uncontrolled trials it has been found to prevent postural hypotension.22 It enhances extracellular volume and systemic vascular resistance23 and increases blood vessel sensitivity to catecholamines. Treatment is initiated at 0.1 mg daily and is increased weekly as needed to a maximum of 0.5 mg daily. As a synthetic mineralocorticoid, fludrocortisone causes sodium retention and potassium loss and can cause worsening of heart failure and supine hypertension.
Midodrine is a peripheral alpha-1 agonist that does not cross the blood-brain barrier, so it causes less anxiety and tremor than other alpha agonists such as pseudoephedrine. A randomized controlled trial in which subjects took midodrine for 3 weeks found it to be effective in reducing orthostatic hypotension and associated symptoms.24The main adverse effects of midodrine are pilomotor reactions, urinary retention, and supine hypertension. As a vasopressor, the peak effect occurs after 1 hour, with a duration of action of 4 hours. As a result, this thrice-daily medication is dosed early in the day (eg, at 7:00 AM, 11:00 AM, and 3:00 PM). Patients should strictly avoid the recumbent position during the period of midodrine activity. Treatment is initiated at 2.5 mg 3 times daily, with a maximum dose of 10 mg 3 times daily. It may be given concomitantly with fludrocortisone.
Pyridostigmine is a peripheral acetylcholinesterase inhibitor that has been shown in a short-term, randomized controlled study to reduce the fall in standing blood pressure with no significant increase in supine blood pressure, which corresponded with improvement in symptoms of orthostasis.24 The therapeutic rationale is that the cholinesterase inhibition amplifies the signal at the sympathetic ganglion, increasing the release of norepinephrine by the postganglionic nerves. There is less risk of supine hypertension, as sympathetic activity is low in the supine position. Treatment is initiated at 30 mg twice daily, with a gradual increase to a maximum of 60 mg 3 times daily. Adverse effects include diarrhea, urinary urgency, nausea, and bradycardia.
Other treatments such as erythropoietin, caffeine, and nonsteroidal anti-inflammatory drugs have been studied for orthostatic hypotension, but only in small numbers of patients or in an uncontrolled manner. Caffeine has been studied more extensively for the treatment of postprandial hypotension.
Conclusion
Chronic orthostatic hypotension should be suspected in older patients with hypertension who present with light-headedness, paroxysmal weakness, or syncope. It is essential that orthostatic blood pressure measurements are performed correctly, as prematurely obtaining the standing measurement will cause a significant underestimation of postural fall in blood pressure. If there is a high index of suspicion, the standing measurement should be extended beyond the usual 3 minutes of standing. In patients with large postural drops in blood pressure, it is worthwhile to stop potentially offending medications, but it is inadvisable to broadly stop antihypertensive medications, as chronic control of hypertension reduces orthostatic tendencies. Measures such as raising the head of the bed to 20 degrees and wearing waist-high compression garments have been found to be effective. Persistent symptomatic orthostatic hypotension should be treated cautiously with pharmacologic interventions. Proper attention to detail in the diagnosis and treatment can lead to a reduction in symptoms and improved quality of life.
The author reports no relevant financial relationships.
Dr. Meuleman is Associate Director of Clinical Affairs, Geriatric Research, Education and Clinical Center, North Florida/South Georgia Veterans Affairs Health System, and Associate Professor of Aging and Geriatrics, University of Florida College of Medicine, VA Medical Center, Gainesville.
References
1. Wieling W, Krediet CT, Dijk N, Linzer M, Tschakovsky ME. Initial orthostatic hypotension: review of a forgotten condition. Clin Sci (Lond). 2007;112(3):157-165.
2. Lakatta EG. Do hypertension and aging have a similar effect on the myocardium? Circulation. 1987;75(1 Pt 2):I69-I77.
3. Davy KP, Seals DR, Tanaka H. Augmented cardiopulmonary and integrative sympathetic baroreflexes but attenuated peripheral vasoconstriction with age. Hypertension. 1998;32(2):298-304.
4. Harper CM, Lyles YM. Physiology and complications of bed rest. J Am Geriatric Soc. 1988;36(11):1047-1054.
5. van Beek AH, Claassen JA, Olde Rikkert MG, Jansen RW. Cerebral autoregulation: an overview of current concepts and methodology with special focus on the elderly. J Cereb Blood Flow Metab. 2008;28(6):1071-1085.
6. Rubenstein LZ, Robbins AS, Josephson KR, Schulman BL, Osterweil D. The value of assessing falls in an elderly population. A randomized clinical trial. Ann Intern Med. 1990;113(4):308-316.
7. Mendu ML, McAvay G, Lampert R, Stoehr J, Tinetti ME. Yield of diagnostic tests in evaluating syncopal episodes in older patients. Arch Intern Med. 2009;169(14):1299-1305.
8. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. The Consensus Committee of the American Autonomic Society and the American Academy of Neurology. Neurology. 1996;46(5):1470.
9. Mader S, Hornick T, Winger J. Effect of initial recumbent or sitting positions on postural blood pressure measurements. Gerontologist. 1987;27:206A.
10. Gangavati A, Hajjar I, Quach L, et al. Hypertension, orthostatic hypotension, and the risk of falls in a community-dwelling elderly population: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston study. J Am Geriatr Soc. 2011;59(3):383-389. doi:10.1111/j.1532-5415.2011.03317.x.
11. Ooi WL, Barrett S, Hossain M, Kelley-Gagnon M, Lipsitz LA. Patterns of orthostatic blood pressure change and their clinical correlates in a frail, elderly population. JAMA. 1997;277(16):1299-1304.
12. Belmin J, Abderrhamane M, Medjahed S, et al. Variability of blood pressure response to orthostatism and reproducibility of the diagnosis of orthostatic hypotension in elderly subjects. J Gerontol A Biol Sci Med Sci. 2000;55(11):M667-M671.
13. McGee S, Abernethy WB 3rd, Simel DL. The rational clinical examination. Is this patient hypovolemic? JAMA. 1999;281(11):1022-1029.
14. Streeten DHP, Anderson GH Jr. Delayed orthostatic intolerance. Arch Intern Med. 1992;152(5):1066-1072.
15. Gibbons CH, Freeman R. Delayed orthostatic hypotension. A frequent cause of orthostatic intolerance. Neurology. 2006;67(1):28-32.
16. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA. 1991;265(24):3255-3264.
17. Masuo K, Mikami H, Ogihara T, Tuck ML. Changes in frequency of orthostatic hypotension in elderly hypertensive patients under medications. Am J Hypertens. 1996;9(3):263-268.
18. Slavachevsky I, Rachmani R, Levi Z, Brosh D, Lidar, Ravid M. Effect of enalapril and nifedipine on orthostatic hypotension in older hypertensive patients. J Am Geriatric Soc. 2000;48(7):807-810.
19. Fan CW, Gasparro D, Crowley V, Cunningham CJ. Acute haemodynamic response to sleeping head-up at 6 inches in older inpatients. Clin Auton Res. 2009;19(1):51-57.
20. Henry R, Rowe J, O’Mahony D. Haemodynamic analysis of efficacy of compression hosiery in elderly fallers with orthostatic hypotension. Lancet. 1999;354(9172):45-46.
21. Jaeger PH, Fawer R, Brunner HR, Monti M, Regli F, Schelling JL. Immersion and venous occlusion plethysmography in patients with idiopathic orthostatic hypotension. Clin Exp Hypertens. 1981;3(5):919-927.
22. van Lieshout JJ, ten Harkel AD, Wieling W. Fludrocortisone and sleeping in the head-up position limit the postural decrease in cardiac output in autonomic failure. Clin Auton Res. 2000;10(1):35-42.
23. Wieling W, Van Lieshout JJ, Hainswoth R. Extracellular fluid volume expansion in patients with posturally related syncope. Clin Auton Res. 2002;12(4):242-249.
24. Low PA, Gilden JL, Freeman R, Sheng KN, McElligott MA. Efficacy of midodrine vs placebo in neurogenic orthostatic hypotension. A randomized, double-blind multicenter study. Midodrine Study Group [published correction appears in JAMA. 1997;278(5):388]. JAMA. 1997;277(13):1046-1051.
25. Singer W, Sandroni P, Opfer-Gehrking TL, et al. Pyridostigmine treatment trial in neurogenic orthostatic hypotension. Arch Neurol. 2006;63(4):513-518.


