An 8-year-old Hispanic child with no significant medical history presented to our pediatric clinic after 2 episodes of vomiting, diarrhea, and abdominal pain. Symptoms had begun earlier the same morning; the child and his parents described the vomitus as "yellowish" and diarrhea "watery." There was no associated fever.
The abdominal pain was "sharp," intermittent, and confined to the left lower quadrant and periumbilical area. It did not radiate and lasted only for a few minutes. Nothing seemed to exacerbate the pain, nor was it relieved with vomiting or diarrhea.
The patient's last meal the previous night was a taco. No other family member had eaten the same thing.
The patient denied sore throat, dysphagia, urinary symptoms, and rash. There was no recent travel history. His parents had given him a single dose of Pepto-Bismol before they brought him in for evaluation.
On physical examination, the child was afebrile and his vital signs were stable--except for tachycardia, with a pulse of 137 beats per minute. The child was well-developed and well-nourished. He was in obvious distress--lying on the examination table, clutching his abdomen--but appeared to be nontoxic.
There were no remarkable physical findings other than marked pain to palpation of the left lower quadrant with guarding. There was equivocal rebound tenderness to the same area. The patient had no significant periumbilical tenderness and no tenderness in other quadrants. He had hyperactive bowel sounds in all 4 quadrants without succussion splash. There were no palpable masses.
The patient had negative psoas and obturator signs and no obvious Murphy sign. Pain was not relieved by sitting forward and upright. He did have some equivocal bilateral costovertebral angle tenderness. There were no purpuric lesions or rashes.

After the history and physical examination, urinalysis was done and an acute abdominal series was obtained. Urinalysis results were negative, including for ketones. Chest films were normal. Results of the abdominal series were negative; there were no air fluid levels, no free fluid, and no signs of obstruction (Figure 1).
Shortly after the patient returned to the office from the radiology department, a fluid challenge was attempted. Initially he did well, but then he writhed with abdominal pain and vomited a yellowish--almost greenish--vomitus. After this witnessed emesis, the patient was sent directly back to the hospital for laboratory work and a CT scan of the abdomen/pelvis with contrast.
The white blood cell count was elevated (19,500/µL); there was a left shift with 92% segmented neutrophils and 2% band forms. Results of a complete metabolic profile were within normal limits. There was no metabolic gap. Amylase levels were normal at 47 U/L. The C-reactive protein value was also normal at 0.0 mg/dL, as was lipase at 17 U/dL.
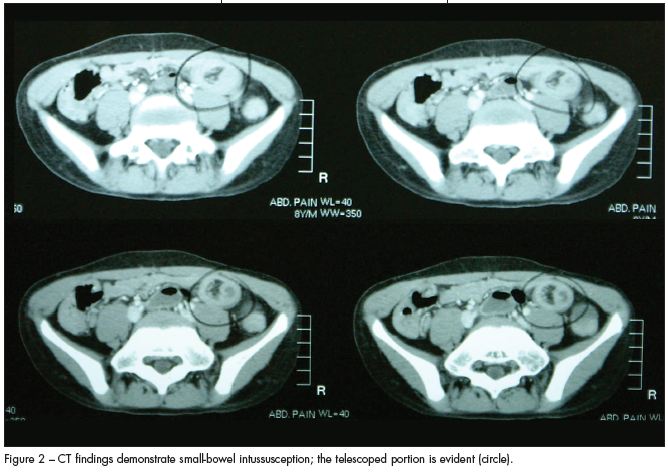
The abdominal CT scan showed the problem: the patient had a significant length of ileal-ileo intussusception (Figure 2).
After the patient returned to the office from the radiology department, an intravenous line was placed and a fluid bolus of normal saline given. This was followed by infusion of dextrose( 5% with half normal saline at a 100% maintenance rate. An emergent surgical consult was obtained in the pediatric office. A local surgeon felt that the child would be best served at a tertiary care facility for pediatric surgical services. Subsequently, the child was emergently transferred by air to such a facility for emergent reduction of his ileal-ileo intussusception.
The pediatric radiologists who reviewed his CT scan agreed with the diagnosis of ileal-ileo intussusception. However, during laparotomy, surgeons could not find the intussusceptum. They believed that it may have spontaneously resolved with the barium from the CT scan sometime during transport. Lucky for this child, they also identified no lead point. He was subsequently discharged after 4 days of postoperative care.
INTUSSUSCEPTIONIntussusception is the invagination of a portion of the bowel into itself, which is pulled along further into itself during peristalsis. As the intussusceptum invaginates further, lymphatic flow occurs, followed by venous obstruction. As the intussusceptum obstructs the lumen of the intestine, distention occurs and further peristaltic waves cause colicky, episodic abdominal pain. As the edema from lymphatic and venous obstruction increases, arterial flow is eventually also obstructed, resulting in ischemic bowel and subsequent shedding of mucus into the bowel lumen. Further, venous engorgement promotes leakage of blood through the capillary membranes into the lumen. Together, this forms the classic "currant jelly" stools noted in intussusception. However, though relatively diagnostic, this finding occurs only in a small percentage of cases and is a fairly late sign of already occurring bowel ischemia.
Intussusception is the most common cause of intestinal obstruction in children 3 months to 3 years old. It occurs most frequently between 3 and 18 months: approximately 65% of cases develop before 12 months.1,2 Although 10% of patients may have had a history of diarrhea--and many have signs and symptoms of an upper respiratory tract infection--no clear cause of intussusception is typically identified. In older children, anatomic abnormality often acts as a lead point. Abnormalities include polyps, Meckel diverticulum, nodular or ectopic pancreas, intestinal lymphoma, cysts, localized edema or hemorrhages (such as with abdominal trauma), Henoch-Schönlein purpura, hemophilia, and leukemia. Postoperative intussusception and intussusception in children with cystic fibrosis are also fairly common.1
The "classic" picture is that of a well infant who suddenly appears to have significant abdominal pain and vomiting. After colicky pain, normal stool is typically passed and the infant may appear well again. Vomitus is nonbilious at first but may become bilious as the obstruction progresses, and abdominal distention can be seen. The classic triad of vomiting, colicky abdominal pain, and bloody stool is not universal and may occur in as few as 10% of cases. As the obstruction progresses, the child may appear profoundly lethargic and quite ill.1,2
If the intussusceptum extends to the anus, it can sometimes be palpated on rectal examination. About 95% of cases are ileocolic; consequently,a sausage-shaped mass can also typically be palpated in the area of the hepatic flexure. In 3% of cases, the intussusception can prolapse through the rectum. A typical intussusception involves the invagination of the terminal ileum into the cecum and colon, which pulls the ileocecal region distally. As a result, the right lower quadrant may feel empty to palpation: this is known as the Dance sign.1
The diagnosis is typically made from the clinical history. Physical findings, including a sausage-shaped mass, bloody stool, or guaiac-positive rectal examination with colicky abdominal pain and vomiting should also raise clinical suspicion of this process. Plain films of the abdomen may reveal obstruction, a soft tissue density outlined by an air-filled colon (a so-called crescent sign on plain films), or no abnormality.2
Sonograms may also identify an intussusception if patients are too ill for diagnostic and possibly therapeutic enema. The gold standard for diagnosis is the contrast enema, which may also reduce the intussusception during the procedure. A failed reduction with contrast enema demands immediate surgical reduction. Reduction with air or radiocontrast enema is successful in up to 80% of cases; however, nearly 25% of patients require surgical resection of nonviable intestine on diagnosis.
The recurrence rate after either enema or surgical reduction is approximately 5%.1 A small-bowel intussusception typically is diagnosed with an upper GI series with a small-bowel follow-through series. Surgical reduction is usually required.2
A delay in diagnosis and therapy can lead to infarction of the affected bowel, peritonitis, perforation, and (if untreated) death within 2 to 5 days.1


