Young Woman With Left Eye Swelling and Pain

A 25-year-old woman presented to the emergency department with left eye swelling and pain of several days’ duration. A CT scan of the orbits without contrast was ordered, and the patient was given meperidine for pain and lorazepam for agitation.
HISTORY
The patient was obtunded and uncooperative. Although it was difficult to obtain a detailed medical history from her, she did admit to having used intravenous drugs, and it was later learned she had consumed “a bag” of heroin earlier that day. HIV and hepatitis C virus status were unknown.
 PHYSICAL EXAMINATION
PHYSICAL EXAMINATION
The patient appeared thin and undernourished, and she had numerous tattoos on her upper torso and neck. There was extensive swelling of the left upper and lower eyelids with marked proptosis and clear discharge with dried crusting on the eyelashes (Figure 1). The patient could not open her left eye and complained of pain when the examining physician attempted to open the lid manually. There were no palpable lymph nodes in the head and neck, and the remainder of the physical examination was unremarkable.
LABORATORY RESULTS
White blood cell count was 9400/µL, with 87.9% neutrophils and 6.9% lymphocytes; hemoglobin level, 10.6 g/dL; hematocrit, 31.4%; and platelet count, 467,000/µL. Sodium level was 128 mEq/L; potassium, 4 mEq/L; chloride, 91 mEq/L; carbon dioxide, 23 mEq/L; glucose, 113 mg/dL; blood urea nitrogen, 10 mg/dL; creatinine, 0.4 mg/dL; and calcium, 8.8 mg/dL. A serum pregnancy test was negative.
IMAGING STUDY RESULTS
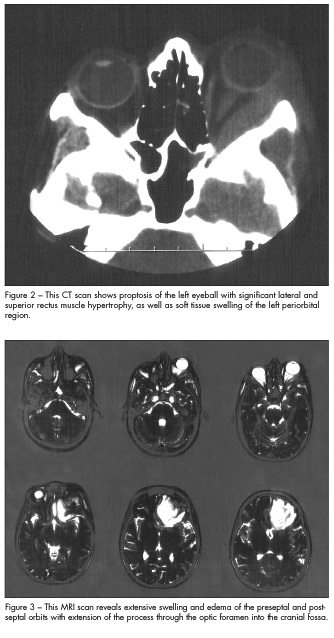
The CT scan showed proptosis of the left eyeball with significant lateral and superior rectus muscle hypertrophy, as well as soft tissue swelling of the left periorbital region (Figure 2). Periorbital cellulitis was diagnosed, and the patient was admitted.
HOSPITAL COURSE
Cefoxitin was started, and an ophthalmology consultation was ordered. The next morning, the patient was found to have decreased vision in the affected eye. MRI of the head with and without gadolinium contrast was ordered. The MRI findings demonstrated extensive swelling and edema of the preseptal and postseptal orbits with extension of the process through the optic foramen into the cranial fossa (Figure 3). There was extensive involvement of the left frontal lobe with a significant mass effect consistent with an abscess.
The patient was transferred immediately to a tertiary care facility for neurosurgical and ophthalmic intervention, and she underwent an emergency craniotomy that evening. A team of neurosurgeons and ophthalmologists removed 15 cc of frank, white pus from the anterior lobe and 5 to 10 cc from the orbit. The patient’s condition improved during her hospital stay, and partial vision in the affected eye was preserved.
THE TAKE-HOME MESSAGE
This case highlights the importance of maintaining a low threshold of suspicion for soft tissue pathologies involving the head and neck, especially when the patient has a history of intravenous drug abuse. When a CT of the orbits is ordered for periorbital cellulitis, a CT of the head should be ordered as well, if there is even the slightest suspicion that there may be extension of the infection. Although the exact cause of the abscess was not determined in this case, the importance of rapid intervention whenever vision is threatened cannot be overstated.


