Young Man With a Numb Chin
A 25-year-old man was admitted to the hospital because of upper back pain. He had a history of rectal adenocarcinoma with metastases to the bladder, which had been diagnosed 2 years earlier. An MRI scan of the spine revealed multiple spinal metastases; there was a large epidural mass at C7-T4 with anterior cord compression. The patient then started palliative radiation therapy to the spine.
Within a few days the patient complained of being unable to feel the left side of his chin. He pointed out that he had bitten the left side of his lip while trying to eat. Physical examination revealed a deficit only in the sensation of pain, temperature, and light touch in the area of his left chin below the lip. The remainder of the facial sensory examination was normal. Facial muscle movement was intact. All other cranial nerves were intact.
What is the likely cause of this patient’s neurologic deficit?
(Answer on Next Page)
 Answer: Numb chin syndrome (mental neuropathy)
Answer: Numb chin syndrome (mental neuropathy)
Numb chin syndrome has been described in the literature since the 1960s and has been recognized as a sign of possible serious illness since that time.1 It is defined as a numbness or paresthesia over the territory of the mental nerve, which includes the chin and lower lip.
This syndrome can result from nonmalignant etiologies, such as trauma, drugs, diabetes mellitus, syphilis, amyloidosis, sarcoidosis, sickle cell anemia, and vasculitis, but the most common and most worrisome cause is metastatic malignancy.2,3 Numb chin syndrome has most frequently been associated with breast cancer and lymphoma; however, it has also been linked to many other malignancies.4 Often a marker for recurrence of a known and now widespread malignancy, it has also been the initial presenting symptom of a new and advanced malignancy.3 In fact, Massey and colleagues5 found that in 47% of cases, numb chin syndrome preceded the diagnosis of the primary tumor.
Symptoms in this syndrome are linked to the inferior alveolar nerve. This nerve has only sensory capabilities and innervates the lower lip and chin as well as the lower gingiva and teeth.2 It originates as part of the posterior trunk of the mandibular division of the trigeminal nerve. It enters the mandible at the mandibular foramen and travels along the mandible until it exits
at the mental foramen. Upon exit from the mental foramen, the inferior alveolar nerve becomes the mental nerve.2
Thus, the neuropathy has been hypothesized to be caused by several different mechanisms. The possibilities include compression of the inferior alveolar nerve itself by mandibular metastases, mandibular nerve compression by skull-base tumors, leptomeningeal metastases, and tumor cell infiltration of the inferior alveolar nerve sheath.3 Lossos and Siegal4 found in a report of 42 patients with numb chin syndrome that mandibular metastases were the most common cause of this syndrome and leptomeningeal metastases occurred next most commonly. They stated that these two etiologies may sometimes be differentiated by the presence of other cranial neuropathies indicating a leptomeningeal origin. Burt and associates2 argued that mandibular metastases are by far the most common cause of numb chin syndrome and if such metastases have not been found, then it is likely they were simply not detectable at that time and by current technology.
In addition to a thorough history and physical examination, the recommended studies in the evaluation of numb chin syndrome include a panoramic radiograph of the mandible, CT of the brain and skull base, MRI, and nuclear bone scintigraphy. If the cause of the patient’s symptoms remains uncertain, cerebral spinal fluid examination may be useful in identifying leptomeningeal metastases.3
Therapy is usually directed at the specific cause, whether it is malignant or benign. In the case of mandibular metastases, systemic therapy should be initiated or changed. Skull-base tumors may respond to local radiation therapy, and leptomeningeal metastases may respond to whole brain irradiation or intrathecal methotrexate injection.4 Unfortunately, the appearance of the numb chin syndrome in the setting of malignancy is a sign of poor prognosis, and treating the syndrome does not improve the outcome.3 Patients with mandibular metastases survive approximately 5 months, and patients with leptomeningeal metastases survive about 12 months.4
OUTCOME OF THIS CASE
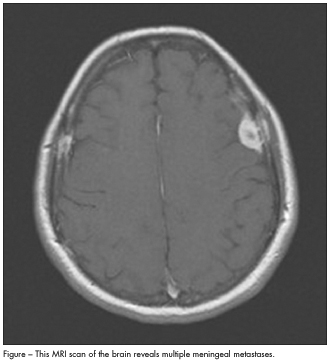
The patient in this case had already received a diagnosis of metastatic adenocarcinoma that was clearly progressive. An MRI scan of the brain revealed multiple meningeal metastases (Figure). No further investigations of his numb chin syndrome were undertaken. It was believed that the meningeal metastases were
the cause of his symptoms, and he started whole brain radiation after completing the local radiation to his epidural metastasis. He may have had a mandibular metastasis, but obtaining this information would not have affected his already poor prognosis. He was referred to hospice care.
TAKE-HOME POINT
Numb chin syndrome is a seemingly small complaint that may foretell a serious illness. In an otherwise healthy patient, it should prompt a search for a primary malignancy. In a patient with a known malignancy, it should prompt a search for recurrent and progressive disease.
- Calverly JR, Mohnac AM. Syndrome of the numb chin. Arch Intern Med. 1963;112:819-821.
- Burt RK, Sharfman WH, Karp BI, Wilson WH. Mental neuropathy (numb chin syndrome): a harbinger of tumor progression or relapse. Cancer. 1992;70:877-881.
- Marinella MA. Numb chin syndrome: a subtle clue to possible serious illness. Hospital Physician. 2000;36:54-56.
- Lossos A, Siegal T. Numb chin syndrome in cancer patients: etiology, response to treatment, and prognostic significance. Neurology. 1992;42:1181-1184.
- Massey EW, Moore J, Schold SC. Mental neuropathy from systemic cancer. Neurology. 1981;31:1277-1281.


