Pigmented Oral Lesions: Clues to Identifying the Potentially Malignant
ABSTRACT: Oral nevi, melanotic macules on the lip, atypical amalgam tattoos, melanoacanthomas, and lesions caused by embedded foreign bodies or by perforating injuries of the oral mucosa all require biopsy, since they can resemble melanoma. An important clue in diagnosing melanoma is its marked tendency to ulcerate in the oral cavity. The amelanotic form may be mistaken for a pyogenic granuloma; thus, biopsy is essential. Lentigo maligna is a slow-growing, precancerous, pigmented lesion that generally occurs on the face; half of the reported cases in the oral cavity became malignant. Accordingly, complete excision is indicated. Take care not to confuse lentigo maligna with nevus of Ota, which involves the eye, facial skin, and oral cavity. Although it resembles lentigo maligna, it rarely becomes malignant. Other lesions that may be safely left alone are physiologic melanin deposits (usually gingival and buccal) in dark-skinned persons and oral pigmentation associated with pregnancy, Peutz-Jeghers syndrome, Recklinghausen’s disease, HIV infection, and Laugier-Hunziker syndrome.
_________________________________________________________________________________________________________________________________________________________________
 A variety of oral pigmented lesions may mimic melanoma. What are these lesions—and which require biopsy to rule out a malignant cause? Here, in the second in a series of articles on oral lesions, I offer answers to these and other key questions. The first article (CONSULTANT, April 2012, page 301) focused on white oral lesions and methods of distinguishing those that are benign from those that are potentially deadly. In subsequent articles, I will discuss erythematous and punctate lesions.
A variety of oral pigmented lesions may mimic melanoma. What are these lesions—and which require biopsy to rule out a malignant cause? Here, in the second in a series of articles on oral lesions, I offer answers to these and other key questions. The first article (CONSULTANT, April 2012, page 301) focused on white oral lesions and methods of distinguishing those that are benign from those that are potentially deadly. In subsequent articles, I will discuss erythematous and punctate lesions.
_________________________________________________________________
RELATED CONTENT
White Oral Lesions: How to Distinguish the Benign From the Deadly
A Mouthful of Oral Lesions
_________________________________________________________________
PHYSIOLOGIC PIGMENTATION
Pigmentation in the oral cavity can result from numerous causes (Table). Thus, a careful history is important. Ask the patient about occupational exposures, medications ingested, and familial disorders. Intrinsic substances deposited include melanin, which is the most common, and hemosiderin; extrinsic material consists primarily of heavy metals, such as lead, mercury, bismuth, and silver.
In all persons except albinos, the basal layer of the oral epithelium normally contains melanocytes. Among African-Americans and others who are dark-skinned, areas of increased pigmentation may not be abnormal.
Racial pigmentation. Melanin pigmentation of the oral cavity is sufficiently common among members of all dark-skinned races, regardless of nationality, to be considered physiologic. Pigmented areas may develop anywhere in the oral cavity, although the gingiva and buccal mucosa are common sites of deposition.
The blue-black to brown lesions may be punctate (macular) or diffuse and may form melanoplakia—broad sheets of stained tissue (Figure 1). These melanin deposits have no pathologic implications. If they bother patients for aesthetic reasons, they may be removed from the gingiva by chemical peeling with phenol. This destroys the melanin in the germinative layer of the epithelium.
Oral melanotic macule. This solitary, dark lesion is generally smaller than 1 cm in diameter and arises in persons with light skin. Buchner and Hansen1 noted the following distribution: lower lip, 28.7%; gingiva, 22.8%; buccal mucosa, 16.2%; and hard palate, 6.7%.
A variation of the melanotic macule is the ephelis, or freckle, which generally appears as a small (2- to 3-mm) brown spot on the lip. This lesion is completely benign, but biopsy must be performed to differentiate it from melanoma.

GENETIC CAUSES
A number of inherited diseases are manifested by pigmented oral lesions. Here I will consider Peutz-Jeghers syndrome, Recklinghausen’s disease (neurofibromatosis), Albright’s syndrome, and Carney syndrome.
Peutz-Jeghers syndrome. Oral melanosis and intestinal polyposis occur in this autosomal dominant genetic disorder. The macular melanin deposits often involve the lips, buccal mucosa, and fingers (Figure 2). Lesions may also develop on the gingiva, palate, and tongue. The polyps in the small intestine are benign and do not undergo malignant transformation, but they may cause intussusception during childhood. No treatment is necessary.
Recklinghausen’s disease. Lightly pigmented cutaneous areas (café au lait spots) develop in some patients with neurofibromatosis. Some of these patients also have macular pigmentation of the oral mucosa, especially on the lips, as a result of melanin deposition. Again, no treatment is necessary.
Albright’s syndrome. This disease of unknown origin is marked by the triad of polyostotic fibrous dysplasia, precocious puberty, and cutaneous pigmentation. Involvement of the oral cavity (café au lait pigmentation) is rare; lips are the site of predilection.
Carney syndrome. This syndrome of facial and mucocutaneous pigmentation, visceral and soft-tissue myxomas, and endocrine overactivity is inherited in an autosomal dominant fashion. In their review of 58 cases, Cook and colleagues2 found 62% had extensive facial freckling; 50%, lip lesions; 71%, cardiac myxomas; and 41%, skin myxomas. They also found 47 lesions involving the adrenal cortex, pituitary, and testes. The occurrence of cardiac myxomas makes this condition potentially lethal.
 HORMONAL IMBALANCE
HORMONAL IMBALANCE
The classic endocrine syndrome characterized by oral melanosis is adrenal insufficiency, or Addison’s disease. Also, pregnancy may cause physiologic changes that affect the oral mucosa.
Addison’s disease. Because of the deficiency of adrenal glucocorticoids (cortisol and corticosterone), the corticotropin-pituitary feedback mechanism remains uninhibited; this results in increased pigmentation from the release of melanocyte-stimulating hormone. The causes of Addison’s disease include tuberculosis, fungal infection, idiopathic adrenal atrophy, tumor metastasis, and amyloidosis.
The oral lesions are generally diffuse and multifocal, but they may be macular (Figure 3); they are accompanied by darkening of the skin as well as hypotension. Other metabolic abnormalities of Addison’s disease include hyponatremia, hyperkalemia, hypoglycemia, and lymphocytosis. The diagnosis of adrenal insufficiency is established by the 24-hour corticotropin-stimulation test. Treat patients with hormone replacement and by determining and managing the underlying cause.
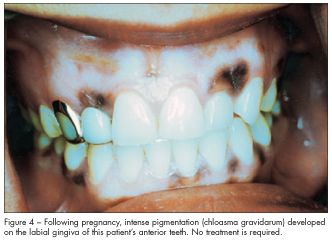
Chloasma. During late pregnancy, physiologic changes produce the characteristic pigmentation of the facial skin known as chloasma gravidarum, or the mask of pregnancy (Figure 4). This condition results from melanocyte stimulation by maternal corticotropin, placental corticotropin-releasing hormone, and ß-endorphin release. In rare cases, there is an intraoral counterpart wherein women experience melanin pigmentation, especially of the gingiva, during or following pregnancy. No treatment is required for this condition.
(Continued on next page)
SYSTEMIC DISEASE
In patients with chronic lung disease and also in those with bronchogenic—but not metastatic—carcinoma, macular pigmentation (3 to 5 cm) on the soft palate, especially laterally, has been reported. Although all the patients were smokers, Merchant and associates3 found no comparable pigmentation in smokers without lung disease. These authors suggest that ectopic adrenocorticotropic hormone production in the lung may cause the pigmentation.
 DRUG THERAPY
DRUG THERAPY
A number of chemical agents can produce oral melanin pigmentation. Quinacrine—originally an antimalarial agent that has been used to treat rheumatoid disorders—occasionally causes oral melanosis. The hard palate is the principal site of involvement.
Chlorpromazine, quinidine, clofazimine, ketoconazole, oral contraceptives, and chemotherapeutic agents (particularly busulfan) may also produce oral pigmentation. Establish the diagnosis by taking a careful history. The pigmentation resolves when the medication is discontinued.
However, the blue oral pigmentation seen with long-term minocycline therapy actually represents insoluble salts of the metabolic degradation of the drug. These salts are deposited in the underlying bone and are visible through the translucent mucosa. Eisen4 found this pigmentation in 10% of 331 patients who took 100 mg of minocycline daily for more than 6 months to treat acne. The most common sites were the maxillary and mandibular anterior alveolus, followed by the lingual aspect of the posterior mandible and the hard palate. Incidence but not intensity increased with the duration of use, and the change was irreversible.
FOREIGN BODIES
Deposits of extrinsic materials in the oral cavity can mimic melanoma.
Amalgam tattoo. This relatively common pigmented lesion is produced when the oral mucosa rubs against an adjacent dental restoration. Fragments of silver or mercury in the amalgam become embedded in the soft tissue, causing precipitation of proteins in immature collagen fibers.
These solitary, localized, gray-black lesions are generally on the buccal mucosa or gingiva adjacent to a restored tooth (Figure 5). If a lesion in this location appears atypical, perform a biopsy to differentiate it from a melanoma. Under microscopic examination, an amalgam tattoo demonstrates fragments of foreign-body material within the connective tissue.
 Graphite deposit. The typical injury that causes this lesion occurs when children stick a pencil in their mouth, play around, and accidentally fall. Fragments from the tip of the pencil break off in the palate; the carbon remains inert and is seen as a dark submucosal mass.
Graphite deposit. The typical injury that causes this lesion occurs when children stick a pencil in their mouth, play around, and accidentally fall. Fragments from the tip of the pencil break off in the palate; the carbon remains inert and is seen as a dark submucosal mass.
Other. Various types of embedded foreign bodies or perforating injuries of the oral mucosa may ultimately become pigmented lesions. The foreign substance itself may have extruded or become phagocytized, but hemosiderin is deposited at the injury site and remains as a marker. Biopsy is often necessary to differentiate the lesion from a nevus or a melanoma.
INGESTION OF HEAVY METAL
A rare and distinctive form of oral pigmentation—a lead line—may result from lead ingestion. Similar lesions can develop from ingestion of other heavy metals, principally mercury and bismuth.
Lead. The lead line is a scalloped band of brown-to-black discoloration along the free gingival margin of the teeth, the result of precipitation of lead by sulfide-producing bacteria in the gingival crevice. This condition has been observed in persons who drink moonshine that was distilled in automobile radiators containing a high lead concentration.
Lead line is also seen in children with pica who have eaten paint that contains lead. By the time this lesion appears, however, the children usually have severe anemia with basophilic stippling of the erythrocytes, as well as neurologic and other systemic signs of lead poisoning.
Bismuth and mercury. Ingestion of these two metals can produce gingival border discoloration. However, since they are no longer employed as antisyphilitic agents, their medical use is now principally of historical interest. Bismuth is a constituent of antidiarrheal preparations. If these agents are abused, the potential for toxicity exists.
Silver. Argyria can result when workers in the photographic industry constantly inhale fumes containing high silver concentrations. A blue-gray discoloration develops on the skin and, to a lesser degree, on the mucous membranes. Earlier in this century, the popularity (and overuse) of nose drops containing silver caused a lesser degree of tissue staining.
REACTIVE CAUSES
Areas subjected to chronic irritation both on the skin and on the mucous membrane may develop foci of increased melanin deposition—a phenomenon termed “post-traumatic pigmentation.” Within the oral cavity, erosive lichen planus lesions may be surrounded by a zone of melanosis. These lesions typically occur on the buccal mucosa and are irregular, with patchy peripheral pigmentation; they are not associated with malignant transformation.
Melanoacanthoma arises primarily on the buccal mucosa and lips but can also occur under the dentures of African-American women.5 These lesions appear as brown, flat plaques with an irregular surface. Under microscopic examination, large dendritic melanocytes and keratinocytes are present. Biopsy is necessary in order to differentiate melanoacanthoma from melanoma.
 SMOKER’S MELANOSIS
SMOKER’S MELANOSIS
Tobacco smoking can cause gingival pigmentation.6 There appears to be a predilection for the mandibular anterior gingiva. Unlike heavy-metal pigmentation, which affects the free gingival margin, smoker’s melanosis develops on the attached gingiva. The degree to which melanin is deposited appears to be related to the amount of tobacco used.
NEVI
Although it is a rare occurrence, every type of nevus that develops on the skin can also arise in the oral cavity. This includes intradermal (intramucosal), junctional, compound, combined, and blue nevi. In their study of 130 intraoral nevi, Buchner and colleagues7 found the incidence to be intramucosal, 63%; blue, 19%; compound, 9%; junctional, 5%; and combined, 4%. The mean age of patients was 32 years, with a strong female preponderance. The most common site was the hard palate, 40%; followed by the buccal mucosa, 19%; lip, 11%; gingiva, 9%; labial mucosa, 7%; soft palate, 7%; retromolar pad, 6%; and tongue, 1%.
Nevi are flat (28%) or slightly elevated (72%) macular lesions with irregular borders (Figure 6). They can be gray, brown, blue, or black. Under microscopic examination, clusters of epithelioid nevus cells are seen, with some melanin granules present.7 Since it is impossible to differentiate clinically among nevi, melanotic macules, and early spreading melanoma, biopsy is essential.
MELANOMA
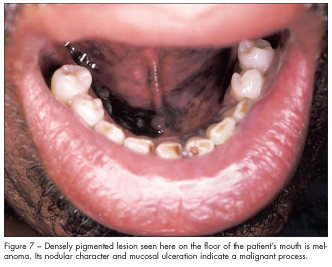
About 1% of all melanomas occur in the oral cavity. In a review of 177 cases of oral melanoma, Rapini and co-workers8 reported that the majority developed after age 40, with a slight male predominance. Eighty-eight lesions occurred on the palate, 46 on the maxillary gingiva, 18 on the buccal mucosa, 10 on the lip, 9 on the mandibular gingiva, 6 on unspecified gingiva, 4 on the tongue, and 1 on the floor of the mouth (Figure 7). Preexisting melanosis was identified in about a third of the cases.
Melanoma may be seen in the mouth as a pigmented macule or nodule, an exophytic mass, or an amelanotic lesion. Except for the last type, the lesion begins as a localized, blue-black patch with diffuse borders. Mucosal streaking develops with continued growth. Melanoma has a marked tendency to ulcerate in the oral cavity, which is of diagnostic importance. The amelanotic form, which is estimated to account for a quarter of the cases, may be mistaken for a pyogenic granuloma. Accordingly, all lesions of this type require biopsy.
Melanoma is highly malignant and carries a poor prognosis (a 5-year survival rate of 3% to 20%). Treatment consists of radical surgery. Local recurrences as well as regional and distant metastases are common.

Lentigo maligna. Also known as melanotic freckle of Hutchinson, lentigo maligna is a slow-growing, precancerous, pigmented lesion composed of melanocytes. It generally arises on the face, primarily in elderly persons; a few cases have been reported in the oral cavity, half of which became malignant. Accordingly, complete excision should be performed.
Nevus of Ota. Take care not to confuse lentigo maligna with nevus of Ota (oculodermal melanocytosis), which involves the eye, facial skin, and oral cavity. Although it resembles lentigo maligna, it rarely becomes malignant. The diagnosis of nevus of Ota is confirmed by the clinical picture; it occurs principally in Japanese persons, and onset is generally in infancy and childhood.
 HIV INFECTION
HIV INFECTION
Brown-black macules and diffuse areas of melanosis have been noted in HIV-infected persons, principally on the buccal mucosa, gingiva, hard palate, and lateral border of the tongue. In some patients, these lesions represent a reaction to drug therapy with clofazimine and ketoconazole; however, in most patients, the cause is unknown.9 No treatment is necessary.
IDIOPATHIC ORIGIN
Pigmentation on the lips, buccal mucosa, hard and soft palates and, occasionally, gingiva of adults that is of unknown cause has been termed the “Laugier-Hunziker syndrome.”10 In some patients, longitudinal pigmented bands in the nails also occur. No treatment is necessary.
1. Buchner A, Hansen LS. Melanotic macule of the oral mucosa: a clinicopathologic study of 105 cases. Oral Surg. 1979;48:244-249.
2. Cook CA, Lund BA, Carney JA. Mucocutaneous pigmented spots and oral myxomas: the oral manifestations of the complex of myxomas, spotty pigmentation, and endocrine overactivity. Oral Surg Oral Med Oral Pathol. 1987;63:175-183.
3. Merchant HW, Hayes LE, Ellison LT. Soft palate pigmentation in lung disease, including cancer. Oral Surg Oral Med Oral Pathol. 1976;41:726-733.
4. Eisen D. Minocycline-induced oral pigmentation. Lancet. 1977;349:400.
5. Tomich CE, Zunt SL. Melanoacanthosis (melanoacanthoma) of the oral mucosa. J Dermatol Surg Oncol. 1990;16:231-236.
6. Pindborg JJ. Atlas of Diseases of the Oral Mucosa. 5th ed. Copenhagen: Munksgaard; 1993.
7. Buchner A, Leider AS, Merrell PM, Carpenter WM. Melanocytic nevi of the oral mucosa: a clinicopathologic study of 130 cases from northern
California. J Oral Pathol Med. 1990;19:197-201.
8. Rapini RP, Golitz LE, Greer RO, et al. Primary malignant melanoma of the oral cavity: a review of 177 cases. Cancer. 1985;55:1543-1551.
9. Langford A, Pohle HD, Gelderblom H, et al. Oral hyperpigmentation in HIV-infected patients. Oral Surg Oral Med Oral Pathol. 1989;67:301-307.
10. Veraldi S, Cavicchini S, Benelli C, Gasparini G. Laugier-Hunziker syndrome: a clinical, histopathologic, and ultrastructural study of four cases
and review of the literature. J Am Acad Dermatol. 1991;25:632-636.


