Pericardial Effusion With Heart Failure: Initial Sign of SLE in a Teenage Girl

A 13-year-old girl was admitted to the inpatient cardiology unit because of progressive dyspnea. She had a history of shortness of breath off and on for the past 2 months, and her symptoms had worsened on the day of admission. She reported having general malaise, insomnia, a 10-kg weight loss, and amenorrhea for the past 4 months. She had no known drug allergies; her immunizations were up-to-date.
On examination, the patient appeared anxious. Ear, eye, nose, and throat findings were unremarkable. Chest expansion was symmetrical, with clear breathing sounds. Heart rate was 150 beats per minute. A grade 3 to 4/6 systolic murmur was audible over the left sternal border fourth to fifth intercostal space. Her extremities were freely movable without edema.
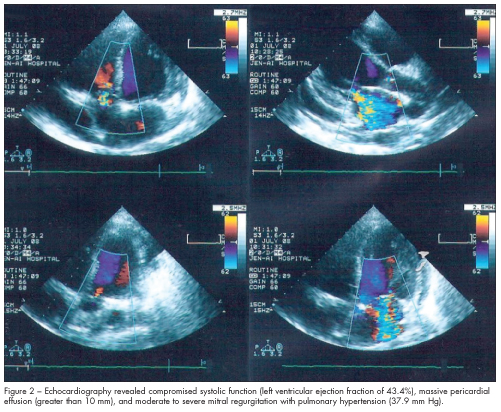
An ECG showed sinus tachycardia, with a heart rate of 130 beats per minute. A chest film taken on admission showed cardiomegaly with pericardial effusion (Figure 1). Echo-cardiography confirmed the cardiomegaly with compromised systolic function (left ventricular ejection fraction of 43.4%), massive pericardial effusion (greater than 10 mm), and moderate to severe mitral regurgitation with pulmonary hypertension (37.9 mm Hg) (Figure 2).
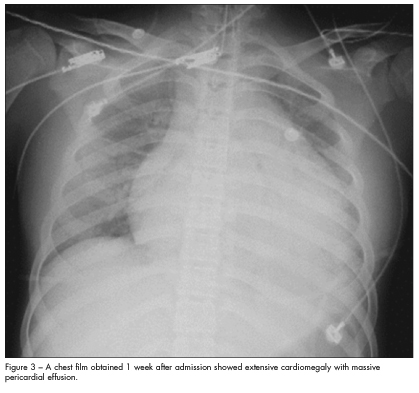
Heart failure from massive pericardial effusion was highly suspected. Treatment with high-dose intravenous corticosteroids was initiated; however, the dyspnea persisted and the patient’s symptoms worsened. A chest film obtained 1 week after admission showed extensive cardiomegaly with massive pericardial effusion (Figure 3). Extracorporeal membrane oxygenation therapy was started. The differential diagnosis of cardiomegaly with and without pericardial effusion in children was considered (Table).
An immunologist was consulted because of concern for systemic lupus erythematosus (SLE)–related cardiac abnormalities. Results of serologic tests for SLE were positive; these included rheumatoid factor (1520 U/mL), antinuclear antibodies (1:640), anti–double-stranded DNA antibodies (1:20), and anti-cyclic citrullinated protein antibodies (601 U/mL).
CARDIAC MANIFESTATIONS OF SLE
Cardiac disease affects many patients with SLE. Pericarditis is the most common cardiac manifestation, with a reported prevalence rate of 60%.1 Other cardiorespiratory problems associated with SLE include pleurisy, pericardial effusions, and myocarditis.2 Cardiac manifestations usually occur at the time SLE is diagnosed or within 6 months of diagnosis.3 Pericardial effusion causing heart failure is a rare initial manifestation of SLE.4
Findings associated with cardiac involvement in SLE. Common clinical features of large pericardial effusion in SLE are Raynaud phenomenon, arthralgia, and lupus nephritis class III or IV. On further questioning, the 13-year-old girl in this case reported having arthralgia. She also had a systolic murmur, which is another common finding in patients with SLE. The cardiomegaly with pericardial effusion in this patient prompted us to consider the differential diagnosis of this entity in children, which led to the evaluation for SLE.
Echocardiography is particularly sensitive and specific in detecting cardiac abnormalities, such as mild pericarditis, valvular lesions, and myocardial dysfunction. It should be performed periodically in patients with SLE.5
Serological findings in SLE typically include positive screens for antinuclear antibody and anti–double-stranded DNA antibody and low C4 and C3 complement levels.6Cardiac involvement in children with SLE has been found to correlate significantly with the presence of anti-Ro and anti-La antibodies.3
 Management of cardiac complications in SLE. After excluding infective endocarditis, a short trial of high-dose corticosteroids can effect overall improvement in carditis of SLE.7 Prednisolone therapy has led to a dramatic decrease in pericardial effusion and improvement in left ventricular diastolic dysfunction in some patients with SLE.2
Management of cardiac complications in SLE. After excluding infective endocarditis, a short trial of high-dose corticosteroids can effect overall improvement in carditis of SLE.7 Prednisolone therapy has led to a dramatic decrease in pericardial effusion and improvement in left ventricular diastolic dysfunction in some patients with SLE.2
Cardiomyopathy that occurs relatively early in the course of SLE may lead to severe cardiac dysfunction despite corticosteroid therapy and appears to be responsive to cytotoxic therapy.7 Pericardial effusion with extensive capillary hyperplasia in SLE may be resistant to medical treatment and may require surgical fenestration.8
Our patient required cytotoxic therapy in addition to supportive extracorporeal membrane oxygenation therapy. She was treated in the pediatric ICU for 2 weeks and then received general ward care for another 2 weeks. During that time, her symptoms resolved and she was
discharged.
1. Bijl M, Brouwer J, Kallenberg GG. Cardiac abnormalities in SLE: pancarditis. Lupus. 2000;9:236-240.
2. Camilleri F, Mallia C. Male SLE patients in Malta. Adv Exp Med Biol. 1999;455:173-179.
3. Oshiro AC, Derbes SJ, Stopa AR, Gedalia A. Anti-Ro/SS-A and anti-La/SS-B antibodies associated with cardiac involvement in childhood systemic lupus erythematosus. Ann Rheum Dis. 1997;56:272-274.
4. Inoue Y, Anzawa R, Terao Y, et al. Pericarditis causing congestive heart failure as an initial manifestation of system lupus erythematosus. Int J Cardiol. 2007;119:e71-e73.
5. Doria A, Iaccarino L, Sarzi-Puttini P, et al. Cardiac involvement in systemic lupus erythematosus. Lupus. 2005;14:683-686.
6. Weich HS, Burgess LJ, Reuter H, et al. Large pericardial effusions due to systemic lupus erthematosus: a report of eight cases. Lupus. 2005;14:450-457.
7. Chockalingam A, Prabhakar D, Gnanavelu G, Chockalingam V. Pancarditis as initial presentation of systemic lupus erythematosus. Int J Cardiol. 2003;87:111-114.
8. Kamata Y, Iwamoto M, Aoki Y, et al. Massive intractable pericardial effusion in a patient with systemic lupus erythematosus treated successfully
with pericardial fenestration alone. Lupus. 2008;17:1033-1035.


