Major Depression: Screening and Diagnosis in Primary Care
ABSTRACT: Major depression is a common illness in primary care that can be under-recognized. The United States Preventive Services Task Force guideline recommends screening for depression in adults when appropriate staff is in place to support depression care and follow-up. Two questions can be used to screen for depression. It is critical to determine the correct diagnosis to provide the optimal care to intervene in the 10% of patients with major depression at risk to commit suicide.
Major depression is a common illness that affects 1 in 6 Americans during their lifetime.1 This disabling condition impacts not only the individual, but also family, friends, and society. The annual cost of depression in the United States is estimated to be $83 billion.2
Depression is under-recognized and challenging to manage because of relapses and recurrences. Half of patients with a first episode of major depression will have a recurrence, 70% after a second episode and 90% after a third episode.
In this 2-part series, I will discuss screening, diagnosing and managing major depression in primar y care. Here, I review the current United States Preventive Ser vices Task Force (USPSTF) guideline for screening and the criteria for diagnosing major depression. In a coming issue, I will focus on the initial treatment options for primary care providers in caring for patients with major depression. The series will be case-based and utilize scenarios to answer a series of questions.
Our first patient is a 35-year-old single mother who has lost her job and reports that she feels tired, has no appetite, has difficulty in sleeping at night, is more forgetful, and does not enjoy her life.
Question 1: How common is major depression in primary care?
A. < 5%
B. 10%
C. 30%
D. 50%
Answer: B. 10%
Patients with multiple somatic complaints are commonly seen in primary care. They should be evaluated for medical conditions, substance abuse, and particular stressors that could contribute to their symptoms. If these have been excluded, consider the possibility of a depressive disorder. This includes major depression, bipolar disorder, minor depression, dysthymia, adjustment disorder with depressed mood, and bereavement. These disorders are clinical diagnoses. They are based on specific symptom-related criteria published in 2000 in the Diagnostic and Statistical Manual of Mental Disorders IV Text Revision (DSM-IV-TR).3 About 10% of outpatients seen by primary care providers meet DSM-IV-TR criteria for major depression; however, only half receive a diagnosis.4-6
Question 2: What does the current USPSTF guideline state about screening adults for depression?
A. Screen all adults
B. Screen some patients
C. Screen when systems are in place
D. Do not screen adults
Answer: C. Screen when systems are in place
SCREENING
The USPSTF guideline for screening for depression in adults was published in 2009.7 The task force’s review of the evidence favors screening adults for depression when staff-assisted depression care supports are in place to ensure the accurate diagnosis, ef fective treatment, and follow-up of patients. It does not support screening in general when no staff is available to help coordinate and provide care for patients with depression. The USPSTF defines staff-suppor ted depression care supports as clinical staff who provide depression care, coordination, case management, or mental health treatment. This can range from a screening nurse in your office to special training for you and your staff or referral to a nurse specialist or behavioral therapist.
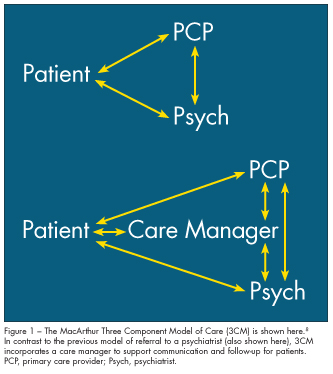
In 1995, the John D. and Catherine T. MacAr thur Foundation organized a multidisciplinary group, including physicians from Harvard University, Duke University, Dartmouth University, and Cornell University, to develop a program to improve primary care management of depression. They created a Three Component Model (3CM) utilizing the USPSTF recommendations, National Institute of Mental Health guidelines, and available evidence to develop a model of care (Figure 1).8 Instead of the previous model of primary care provider referral to a psychiatrist, this model incorporates a care manager to support communication and follow-up for patients. The MacArthur Initiative on Depression and Primary Care provides practical online tools and resources to help enhance the management of depression in primary care.
Question 3: How can you screen for major depression?
A. Forms filled out by patients
B. Asking two questions
C. Genetic testing
D. A and B
Answer: D. A and B
Although screening for depression in primary care may one day involve genetic testing, it currently is not a standard of care in practice. There are, however, several tools to screen for depression. Some examples include the Center for Epidemiologic Studies Depression Scale, Beck Depression Inventory, Symptom-Driven Diagnostic System for Primary Care, Medical Outcomes Study depression measure, and Quick Diagnostic Interview Schedule. These case-finding instruments have sensitivities of 89% to 96% and specificities of 51% to 72% for diagnosing major depression. Many of these screening scales have 15 to 30 questions eliciting symptoms of depression, and it can be time-consuming to complete these forms. The Patient Health Questionnaire–Nine (PHQ-9) has nine questions and can be filled out by patients (Figure 2). It has been found to be a reliable and valid instrument for screening and defining the severity of depression.9
A simple two-question case-finding instrument has been studied; positive responses to both questions resulted in a sensitivity of 96% and a specificity of 57% for major depression (Table 1).10 This may be a convenient way to screen for depression in a busy primary care office.

DIAGNOSIS
Diagnostic criteria. While it may be helpful to consult a psychiatrist for the diagnosis of major depression, you can make the diagnosis by asking about specific symptoms in the history. Major depression is a clinical diagnosis based on a set of symptoms. The DSM-IV-TR criteria for diagnosing major depression are based on asking about nine specific symptoms that occur nearly every day over the same 2-week period and represent a change from previous functioning. The nine symptoms include:
•Feeling sad or depressed mood.
•Sleep disturbance.
•Loss of interest or pleasure in doing things.
•Inappropriate guilt feelings.
•Fatigue or loss of energy.
•Difficulty in concentrating or indecisiveness.
•Change in appetite or weight (ie, defined as 5% change in body weight in 1 month).
•Psychomotor retardation or agitation.
•Recurrent thoughts of death or suicide.
Patients with major depression must have at least five of these nine symptoms. One of the symptoms must be a depressed mood or loss of interest or pleasure.
One method of remembering these symptoms is an abbreviation for prescribing “energy pills” to help treat patients with depression or “Sign for Energy Capsules” or “Sig E Caps.” Clearly, it is not appropriate to prescribe antidepressants for all patients with depression; however, this can be a helpful tool in remembering the questions to ask to determine the diagnosis. The mnemonic “Sig E Caps” was devised by Carey Gross, MD, at the Massachusetts General Hospital and refers to eight of the nine symptoms of depression.11 If we add the letter “D,” we have “D Sig E Caps,” all nine symptoms (Table 2).

Question 4: How can you distinguish between major depression, bipolar disorder, minor depression, dysthymia, adjustment disorder, and bereavement?
A. History
B. Physical examination
C. Genetic testing
D. MRI
Answer: A. History
Differential diagnosis. The history is essential for primary care practitioners and psychiatrists in distinguishing the various depres- sive disorders. Major depression is also called unipolar depression. This is impor tant to distinguish from bipolar disorders, in which patients have major depression with episodes of mania (bipolar I disorder) or hypomania (bipolar II disorder). The symptoms of mania and hypomania can be unmasked in patients who are treated for major depression but who actually have bipolar disorder. Patients with bipolar disorders have periods of elevated, expansive, or irritable moods that can be accompanied by inflated self-esteem, grandiosity, decreased need for sleep, pressured speech, racing thoughts, distractibility, psychomotor agitation, or excessive involvement in pleasurable activities that could lead to harm. Some sample questions to ask patients with suspected bipolar disorders are listed in Table 3.
Patients with minor depression have two to four of the nine symptoms listed in Table 2 for 2 weeks. This must include either a depressed mood or anhedonia. If these symptoms persist for 2 or more years, dysthymia is diagnosed. Patients receive a diagnosis of adjustment disorder with depressed mood if they have an identifiable stressor, symptoms out of proportion to what is expected, social and occupational impairment lasting up to 6 months, and insufficient criteria to meet the diagnosis of major depression. Bereavement may be diagnosed if patients have symptoms that resemble those of major depression which last less than 2 months and are related to the death of a loved one. It is critical to establish the correct diagnosis in patients with depressed mood because management may not treat the underlying problem and could cause harm (Table 4).
Question 5: How common is suicide among patients with major depression?
A.<5%
B. 10%
C. 30%
D. 50%
Answer: B. 10%
ASSESSMENT OF SUICIDE RISK
About 10% of all patients with major depression will eventually commit suicide. Some of the risk factors include prior suicide attempts, hopelessness, living alone, psychotic symptoms, substance abuse, age-specific risk (ie, older white men, young black men), and family history of suicide attempts. Question all depressed patients specifically about thoughts of harm to self or others (Table 5). It is imperative to develop a safe treatment plan, which may range from continued primary care follow-up to immediate emergency department psychiatric referral.
1. Kessler RC, Berglund P, Demlar O, et al. The epidemiology of major depressive disorder. JAMA. 2003;289:3095-3105.
2. Donohue JM, Pincus HA. Reducing the societal burden of depression: a review of economic costs, quality of care and effects of treatment. Pharmoco- economics. 2007;25:7.
3. American Psychiatric Association. Diagnostic
and Statistical Manual of Mental Disorder, 4th ed, Text Revision. Washington, DC: American Psychiatric Association; 2000.
4. Shurman RA, Kramer PD, Mitchell JB. The hidden mental health network. Treatment of mental illness by nonpsychiatrist physicians. Arch Gen Psychiatry. 1985;42:89-94.
5. Simon GE, Von Korff M. Recognition, manage- ment, and outcomes of depression in primary care. Arch Fam Med. 1995;4:99-105.
6. Von Korff M, Shapiro S, Burke JD, et al. Anxiety and depression in a primary care clinic. Comparison of Diagnostic Interview Schedule, General Health Questionnaire, and practitioner assessments. Arch Gen Psychiatry. 1997;44:152-156.
7. U. S. Preventive Services Task Force. Screening for Depression in Adults: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2009;151:784-792.
8. MacArthur Initiative on Depression in Primary Care website: http://www.depression-primarycare. org/.
9. Kroenke K, Spitzer RL, Williams JB. The PHQ-9 validity of a brief depression severity measure.
J Gen Intern Med. 2001;16:606-613.
10. Whooley MA, Avins AL, Iranda J, Browner WS. Case-finding instruments for depression: two questions are as good as many. J Gen Intern Med. 1997;12:439-445.
11. Brigham and Women’s Hospital. Depression:
A Guide to Diagnosis and Treatment. 2001. National Guideline Clearinghouse. Available at www.guide- line.gov/summar y/summar y.aspx?doc_id=3432. Accessed November 17, 2011.
12. Bostwick JM. A generalist’s guide to treating patients with depression with an emphasis on using side effects to tailor antidepressant therapy. Mayo Clin Proc. 2010;85:538-550.


