Ingrown Toenails: Current Procedures to Treat Acute and Chronic Problems— Steps to Prevent Recurrence
ABSTRACT: Trauma, incorrect toenail trimming, and tight, occlusive footwear are all common causes of ingrown toenails. Mild to moderate inflammation and infection may be relieved by conservative measures, including changing footwear, decreasing activity, warm soaks, antibiotic therapy, elevating the edge of the impinged nail, debridement, or removal of the corner of the toenail containing the spike. For patients who have severe impingement with acute infection, partial or complete nail avulsion is the treatment of choice. If avulsion is followed by recurrent infection, partial or complete ablation of the nail matrix may become necessary after the infectious process has resolved. Teach patients to trim their toenails straight across and not to curve them toward the lateral margins.
________________________________________________________________________________________________________________________________________________________
Although small in size, ingrown toenails can have large ramifications when considering the frequency of the problem and the amount of pain they inflict. The great toe is almost exclusively affected, and the condition may be complicated by bacterial or fungal infection. Depending on the extent of impingement and infection, management of ingrown toenails may involve conservative measures or minor surgery.
Symptomatic ingrown toenails most commonly affect persons in 2 age groups. Acute bacterial infection associated with an ingrown toenail occurs more frequently among younger patients (aged 10 to 20 years) of both sexes. Inflammation and infection frequently develop following trauma, such as stubbing the toe, improper nail trimming (curving the cut at the edge, rather than straight across), and picking or tearing the toenails. As the injured or torn nail grows outward, impingement of its edge may lead to infection.
______________________________________________________________________________________________________________________________________________________
Related Content
Floss Fix for Ingrown Toenails
Toenail Onychomycosis: A Scientifically Designed Topical Treatment Option
_____________________________________________________________________________________________________________________________________________________
A second peak in incidence of ingrown toenails occurs during the fifth and sixth decades, particularly among women. With advancing age, the toenail can become deformed; the subsequent thickening and hypertrophy are associated with chronic fungal infection. Incurving of the outer edges causes significant discomfort. Bacterial infection is uncommon in this scenario.
In this article we describe (and illustrate) several procedures that can be performed in the office, with an explanation of the pros and cons of each. We also outline the technique for placing a digital nerve block. A brief review of the anatomy of the toenail sets the stage.
 THE NORMAL TOENAIL AND NAIL BED
THE NORMAL TOENAIL AND NAIL BED
The toenail is composed of 3 layers of overlapping keratinized cells: a thin, stiff, brittle dorsal layer; a thicker, softer middle layer; and a thin deep layer that is probably derived partly from the nail bed.1 Despite its apparent density, the nail is actually 10 times more permeable to water than the adjacent skin. This permeability enables treatment with topical agents that may be effective against some mycotic infections.
The toenail grows 0.01 to 0.05 mm/d; growth is more rapid in younger persons. Replacement of an injured or avulsed nail can take 3 to 6 months. Accordingly, recurrent ingrown toenails often become symptomatic 3 to 6 months after an initial avulsion procedure.
The toenail is supported by the nail unit: the proximal nail fold, the nail bed, the nail matrix, and the hyponychium. The epithelial surface of the nail bed has undulating ridges that interdigitate with the toenail’s under-surface, creating a firm attachment as the nail grows distally. The proximal nail fold (including the cuticle), the lateral nail folds, and the hyponychium constitute the epithelial borders of the toenail. The hyponychium forms a seal between the distal toenail and the nail bed.
The nail matrix is the main germinative area of the nail unit. It extends proximally from the distal aspect of the lunula for the entire width of the nail. Thus, when excising the matrix region, one must always resect beyond the proximal margin of the lunula to avoid recurrent toenail growth.
The matrix extends proximally 5 to 8 mm above the edge of the cuticle to a point near the insertion of the long extensor tendon and the interphalangeal joint. (This anatomic fact is important; if infection follows a toenail ablation, it may extend into this joint.) The lunula produces the middle layer of the nail; the eponychium contributes the thin outermost layer.
Distally, the nail matrix is contiguous with the nail bed. There is germinative potential in the proximal nail fold tissue and in the upper layers of the nail bed as well.2 These areas may be factors in occasional postoperative recurrent nail growth following attempted toenail ablation.
The toenail gives stability to the distal soft tissue of the toe, which frequently becomes elevated following ablation of the nail. As a new nail grows outward, it often impinges against the soft tissue, leading to nail deformity or an ingrown toenail.
The orientation of the nail matrix cells and the longitudinal grooves of the nail bed result in typical distal growth of the toenail. Injury to the toenail matrix or plate may result in elevation of the nail, detachment, or abnormal growth.
HOW AN INGROWN TOENAIL DEVELOPS
The term “ingrown” toenail is unfortunate, because it implies that the nail edge grows laterally and downward into the adjacent soft tissue. In reality, this tissue becomes inflamed and hypertrophied, and as it enlarges the edge of the toenail impinges on it. When the nail plate penetrates the soft tissue, further inflammation and infection frequently follow.
Normally, there is a 0.5- to 1-mm space between the lateral nail fold and the lateral margin of the nail. The nail fold, which is lined with a thin layer of epithelium, is sufficiently wide to avoid irritation from the nail. This space is reduced with trauma, compression from shoes or tight stockings, or other extrinsic pressure. Reactive swelling leads to epithelial hyperplasia and permanent soft tissue hypertrophy. Finally, the toenail margin cuts into the lateral nail fold, resulting in a foreign-body reaction and secondary infection.
Ingrown toenails may be classified according to the magnitude of inflammation and infection:
•Stage 1—Swelling and erythema along the lateral nail border. The toenail edge may be embedded in the lateral nail fold.
•Stage 2—Increased pain, drainage, development of actual infection.
•Stage 3—Chronic infection, with development of granulation tissue; hypertrophy of the adjacent soft tissue (Figure 1).
 ASSESSMENT
ASSESSMENT
A detailed family history may reveal nail problems or familial factors. Genetic disorders, especially those associated with collagen abnormalities (e.g., Darier’s disease, nail-patella syndrome, and pachyonychia congenita), can cause dermatologic and nail disorders. Trauma and mycotic infection are common causes of toenail abnormalities, but rheumatologic, hematologic, endocrine, hepatic, renal, pulmonary, and gastrointestinal disease can also significantly change the texture, shape, color, thickness, or growth rate of the toenail.3
Vascular insufficiency may cause conditions other than ingrown toenail (e.g., fungal infections leading to elevation of the toenail). Inspect the foot and leg for signs of other skin abnormalities, such as blisters, ulcers, rashes, and lesions.
A radiograph of the involved toe is sometimes helpful in evaluating a recurrent toenail infection. Radiographic studies may also help in assessing osteomyelitis of the phalanx and, on occasion, in diagnosing a subclinical subungual exostosis.4 The latter condition may lead to chronic toenail elevation, ulceration, and/or infection.
CONSERVATIVE TREATMENT
Prophylactic measures. Loose-fitting stockings and shoes with a roomy toe box may decrease extrinsic pressure on the toenail. Correct toenail trimming may prevent impingement on adjacent soft tissue. Tell patients to cut toenails straight across; trimming nails in a curve down to the lateral margins promotes nail “spikes” and impingement on the adjacent soft tissue.5 Some advocate trimming the nails with a V-shaped notch in the middle, suggesting that this allows the nail to grow toward the center, thus relieving pressure at the lateral nail margin. We have not found this method to be effective.
General measures. Once inflammation or infection has occurred, conservative measures may help alleviate symptoms. Tell patients to decrease activity, such as running and other sports, as this may reduce inflammation. Soaking the foot in tepid, soapy water 3 times daily often reduces erythema. Massaging the inflamed area will promote drainage. Use of a broad-spectrum, first-generation cephalosporin may counter an early infection.
Elevating the nail edge. If the impingement is not severe, it may be reduced by elevating the advancing edge of the toenail, displacing the soft tissue as the nail slowly grows outward.6 A digital nerve block is usually necessary for the initial procedure in the office.
After the anesthetic has taken effect, tear a wisp of cotton from a cotton-tipped wooden applicator. Break the wooden stick spirally, and use the sharp point to wedge the cotton beneath the edge of the ingrown toenail. Instruct patients to paint the inflamed area with alcohol 2 or 3 times daily to help resolve the inflammation. Often, they must return to the office for a repacking, after which they may do this at home.
Emphasize that it could take 3 months until the toenail grows beyond the lateral toenail fold and that the packing must remain in place for that period. (Obviously, the more the toenail has been cut back, the longer it will take to regrow.) Instruct patients to soak the toe for 15 minutes every other day, then remove the cotton with fine tweezers and repack it as originally done in the office. Tell them to cut the regrown nail transversely and to avoid picking and tearing it.
With stage 2 and 3 infections, when the nail plate has penetrated deep into the adjacent soft tissue, excision of the lateral nail margin can quickly alleviate symptoms. Whether a diagonal or longitudinal section of nail has been removed, patients must also be counseled about the technique of elevating the advancing nail edge. Failure to do this guarantees a high rate of recurrence of infection.
Nail debridement. Chronic mycotic infection may result in an elevated and deformed toenail (Figure 3A), but it may not need to be removed. Simple debridement, using a hand clipper and power nail sander, may reduce the nail’s size. It may be trimmed back to its attachment to the nail matrix and bed (Figure 3B). Proper nail care every few months thereafter may be sufficient to avoid pain and subsequent infection.

SURGICAL TREATMENT
Triangular excision of the nail. When there is acute inflammation and infection, excision of a triangular segment of the nail edge may reduce severe symptoms. After removal of this portion, however, the adjacent soft tissue may hypertrophy and fill the space. As the remaining nail advances distally, it may then impinge on the elevated and thickened lateral and distal soft tissue, leading to recurrent episodes of infection. Thus, the patient must keep the growing edge of the nail elevated with cotton packing, as described above.
Some physicians advocate cutting a V-shaped wedge from the center of the nail, in the belief that this will decrease the lateral soft tissue impingement. We have found that this treatment is largely ineffective.
Nail edge (partial nail plate) avulsion. For patients with chronic bacterial infections (stages 2 and 3) following toenail impingement in the lateral nail fold, a partial nail plate avulsion is indicated. For this, as well as all following procedures, first place a digital anesthetic block and cleanse the toe with an iodine-povidone solution.
Elevate the outer edge of the nail plate by advancing a small Freer elevator beneath the nail to a level proximal to the cuticle (Figure 5A). Using a small bone cutter or scissors, cut the nail edge longitudinally. Remove the narrow nail section with a hemostat (Figure 5B). Inspect the lateral nail fold to make sure that no nail remains in it. Cover the toe with a compression gauze dressing.

Give patients an analgesic agent, to be used as needed. Although acute infections usually resolve rapidly after nail edge resection, physician preference and/or the severity of the infection will determine the need for a systemic antibiotic. However, recent data suggest that antibiotics may not improve post-procedure infection rates.7
Tell patients to remove the dressing twice daily and soak the foot in a tepid Epsom salt solution (1 tablespoon of Epsom salt per basin of water) to help reduce inflammation. A fresh dressing should be applied after soaking. Once drainage subsides, no dressing is required.
Follow-up care is crucial to avoiding recurrent infection. As the growing nail advances, patients must keep the nail edge elevated with cotton, as previously described, until it grows past the end of the lateral nail fold. Instruct patients in proper toenail trimming techniques.
Complete nail plate avulsion. In extensive (stage 3) or paronychial infection, a complete nail plate avulsion may be necessary. Although this helps resolve an acute infection, it removes soft tissue support of the distal phalanx. As the new nail grows, it frequently impinges on the distal soft tissue. Because of the high rate of recurrence following complete toenail avulsion, reserve this procedure for patients with severe infections (stages 2 and 3).8
After the initial preparations, use a small Freer elevator to lift the entire nail to a point proximal to the cuticle. Grasp and remove the elevated nail with a hemostat. The initial bleeding is usually controlled with a compression dressing. Aftercare is the same as for partial avulsion.
Tell patients to start tepid soaks in Epsom salt baths after 24 hours to help diminish inflammation. Again, use of antibiotics depends on physician preference and the severity of the infection. Patients must change dressings daily until drainage subsides. The toe may be painted with alcohol to diminish drainage. Instruct patients about maintaining elevation of the distal and lateral nail margins for several months during nail regrowth, to prevent recurrent infection.
Complete toenail avulsion has a poor long-term success rate, probably because patients fail to comply with follow-up care. Reported rates of recurrent infection are as high as 86%.9,10 Both partial and complete toenail avulsion may require further procedures such as partial or complete onychectomy (ablation) to prevent recurrent infection.
PARTIAL ONYCHECTOMY
Nail edge ablation (partial onychectomy, or Winograd procedure11) can be performed only after complete resolution of an acute infection. Following nail edge avulsion, a 4- to 6-week wait may be required for the infection to subside.
After obtaining anesthesia and cleansing the toe, use a Penrose drain as a tourniquet around the base of the toe. Make an oblique incision at the apex of the nail plate and a longitudinal incision along the lateral nail fold, excising the lateral cuticle and eponychium (Figure 7A).
Resect the matrix down to the phalanx and laterally to include the nail fold in this region (Figure 7B). Some physicians carry the excision just to the distal edge of the lunula, while others (believing there is significant germinative tissue in the nail bed) continue the incision along the lateral nail fold as well. (We prefer the latter procedure.) In other cases, only the proximal and lateral nail matrix in the area of the lunula is resected. Excise all matrix from the cortex of the distal phalanx.
Approximate the skin edges with interrupted sutures (Figure 7C), and apply a gauze compression dressing. Have the patient return after 24 hours to have this dressing changed. Although fairly brisk bleeding occurs initially, it usually subsides within 48 hours. Remove the sutures after 2 to 3 weeks. Nail regrowth varies following this procedure, but it usually occurs in fewer than 10% of patients.

Sleeve method. An alternative to partial onychectomy has been described by several authors,12-14 although results have been similar to the traditional Winograd procedure. Following is a brief description of the procedure, included for completeness.
After initial preparations as above, remove any granuloma that may have developed along the lateral nail margin with electrocautery or sharp dissection. Some also advocate subsequent phenol application to prevent recurrence of granuloma.12 Next, elevate the lateral nail margin using a Freer elevator or similar blunt device. Cut and remove the lateral margin of the nail using a small bone cutter or scissors. Limit resection to the lateral quarter of the nail (just enough to allow insertion of the plastic sleeve). Insert a piece of plastic tubing (e.g., sterilized IV tubing that has been split longitudinally down the side) along the lateral margin of the nail. Fix the tubing in place with a nylon suture through the nail (taking care not to penetrate any soft tissue). Cover the toe with a soft gauze dressing.
Give the patient an analgesic agent and instruct him or her to change the dressing daily for 1 week, at which time the patient should be seen in the office. The tube should be kept in place for 6 to 8 weeks, after which time it may be removed at home by the patient. Patients should also be instructed on proper nail trimming.
COMPLETE ONYCHECTOMY
In the case of a severe toenail deformity or when significant deformity results from a chronic mycotic infection, a complete toenail ablation (Zadik procedure15,16) may be indicated. If the patient has an acute bacterial infection, avulse the toenail first, and carry out ablation after the infection has subsided. With chronic nail infection or a mycotic infection with deformity, avulsion and ablation may be performed at the same time.
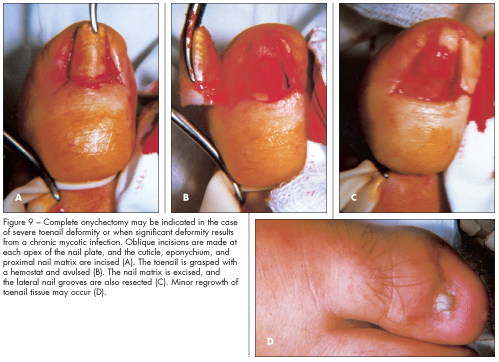 After the usual preparations and the placement of a tourniquet, make oblique incisions at each apex of the nail plate (Figures 9A and 9B). Excise the entire cuticle, eponychium, and proximal nail matrix, extending into the lateral nail folds (Figure 9C). Leave the toenail bed in place; its removal would leave a large area deficient of any soft tissue coverage. Carry out a loose skin closure with interrupted sutures.
After the usual preparations and the placement of a tourniquet, make oblique incisions at each apex of the nail plate (Figures 9A and 9B). Excise the entire cuticle, eponychium, and proximal nail matrix, extending into the lateral nail folds (Figure 9C). Leave the toenail bed in place; its removal would leave a large area deficient of any soft tissue coverage. Carry out a loose skin closure with interrupted sutures.
Apply a gauze compression dressing, to be changed after 24 hours. The initial brisk bleeding usually subsides in 24 hours. Remove sutures 2 to 3 weeks following surgery. After a few days, patients can apply a desiccating agent on the operative area to reduce drainage.
Warn patients that there may be a minor regrowth of nail tissue from germinative tissue along the course of the nail bed (Figure 9D). A recurrence rate as high as 30% following complete onychectomy has been reported.3,9 This rarely presents a problem, but reexcision occasionally becomes necessary when recurrence is significant.
SOFT TISSUE RESECTION
The Vandenbos procedure17 has been suggested as an alternative to partial or complete onychectomy. This procedure involves resecting the soft tissue along the lateral margins of the nail, rather than resecting the nail and its bed.
After initial preparations and tourniquet placement as above, an incision is made along the lateral border of the nail. The incision starts just proximal to the cuticle and extends distally just beyond the edge of the nail plate. A second incision is made on the other side of the nail. The incisions should be elliptical in shape and remove a wedge of tissue 3 to 5 mm wide on either side of the nail, but leave the nail plate and the nail bed intact (Figure 10A). Light cautery may be used along the skin margins to reduce postoperative bleeding. The incisions may be loosely sutured (Figures 10B and 10C) or left open to heal by secondary intention.17
Apply a gauze compression dressing and instruct the patient to elevate the limb and change the bandage the next day. As with complete onychectomy, brisk bleeding usually subsides within 24 to 48 hours. Tepid Epsom soaks can begin after 48 hours. If used, sutures should be removed at 3 weeks. Healing can be expected at 4 to 6 weeks if wounds are left open, although patients must be diligent in performing Epsom soaks and dressing changes to prevent infection.
PHENOL MATRIXECTOMY
Surgical ablation can be avoided with an alternative procedure involving use of phenol (carbolic acid).8 After placing an anesthetic block, partially or completely avulse the affected toenail, as necessary. After partial avulsion, curette the toenail edge.
Spread a protective coat of petroleum jelly on areas adjacent to the exposed matrix, and sponge the matrix dry with cotton swabs. Dip a swab into a fresh 88% phenol solution and make 2 or 3 brief applications to the matrix; follow each application with an alcohol rinse to dilute the acid.
Phenol matrixectomy is technically easy and often causes less postoperative pain than the other procedures described.18 Nevertheless, a high rate of recurrence (from 3% to 20%) has been reported because of difficulty in ablating the proximal and peripheral nail matrix.4,11
Bipolar cautery19 and carbon dioxide laser cautery20 have been suggested as alternatives to phenol or surgical matrixectomy. Results have been on par with traditional forms of matrixectomy.
SYME AMPUTATION
Occasionally, when a more extensive excision is necessary or a more reliable procedure is desired, a Syme amputation of the distal phalanx is performed. Following preparation of the toe and application of a tourniquet, make an elliptical incision to excise the nail matrix and bed, the lateral and proximal nail folds and cuticle, and the skin adjacent to the distal phalanx (Figure 11A). Then excise the distal half of the distal phalanx (Figure 11B); this enables closure of the distal plantar skin to the dorsal skin (Figure 11C). Apply a compression gauze dressing, to be changed daily until drainage subsides.
The patient is allowed to walk, wearing a postoperative shoe or a sandal until the swelling subsides. Remove the sutures 3 weeks after the surgery. In comparison with onychectomy and phenol matrixectomy, Syme amputation carries a decidedly lower recurrence rate (4% to 12%).4,11 This quality renders it desirable to many patients, but some (especially women) consider the procedure cosmetically unacceptable.
1. Dockery GL. Nails, fundamental conditions and procedures. In: McGlamary ED, ed. Comprehensive Textbook of Foot Surgery. Baltimore: Williams & Wilkins; 1987:3-37.
2. Johnson M, Comaish J, Shuster S. Nail is produced by the normal nail bed: a controversy resolved. Br J Dermatol. 1991;125:27-29.
3. Coughlin MJ. Toenail abnormalities. In: Mann RA, Coughlin MJ, eds. Surgery of the Foot and Ankle. St Louis: Mosby-Year Book Inc; 1993:1033-1071.
4. Coughlin MJ. Abnormalities of the toenail. In: DeLee JC, Drez D, eds. Orthopaedic Sports Medicine: Principles and Practice. Philadelphia: WB Saunders Company; 1994:1878-1891.
5. Johnson KA. Ingrown toenails. In: Johnson KA, ed. Surgery of the Foot and Ankle. New York: Raven Press; 1989:83-100.
6. Ceh SE, Pettine KA. Treatment of ingrown toenail. J Musculoskeletal Med. 1990;7(5):62-82.
7. Bos AM, van Tilburg MW, van Sorge AA, Klinkenbijl JH. Randomized clinical trial of surgical technique and local antibiotics for ingrowing toenail. Br J Surg.2007;94(3):292-296.
8. Mann RA, Coughlin MJ. Toenail abnormalities. In: Mann RA, Coughlin MJ, eds. Videotextbook of Foot and Ankle Surgery. St Louis: Medical Video Productions; 1991:56-66.
9. Pettine KA, Cofield RH, Johnson KA, Bussey RM. Ingrown toenail: results of surgical treatment. Foot Ankle. 1988;9:130-134.
10. Dixon GL. Treatment of ingrown toenail. Foot Ankle. 1983;3:254-260.
11. Winograd AM. A modification in the technique of ingrown nail. JAMA. 1929;91:229-230.
12. Abby NS, Roni P, Amnon B, Yan P. Modified sleeve method treatment of ingrown toenail.
Dermatol Surg. 2002;28(9):852-855.
13. Heidelbaugh JJ, Lee H. Management of the ingrown toenail. Am Fam Physician. 2009;79(4):
303-308.
14. Peyvandi H, Robati RM, Yegane RA, et al. Comparison of two surgical methods (Winograd and sleeve method) in the treatment of ingrown toenail. Dermatol Surg.2011;37(3):331-335.
15. Murray WR. Onychocryptosis. Clin Orthop. 1979;142:96-102.
16. Zadik FR. Obliteration of the nail bed of the great toe without shortening the terminal phalanx. J Bone Joint Surg. 1950;32:66-67.
17. Chapeskie H. Ingrown toenail or overgrown toe skin? Alternative treatment for onychocryptosis. Can Fam Physician. 2008;54(11):1561-1562.
18. Kuwada G. Long-term evaluation of partial and total surgical and phenol matrixectomies.
J Am Podiatr Med Assoc. 1991;81:33-36.
19. Farrelly PJ, Minford J, Jones MO. Simple operative management of ingrown toenail using bipolar diathermy. Eur J Pediatr Surg. 2009;19(5):304-306.
20. Ozawa T, Nose K, Harada T, Muraoka M, Ishii M. Partial matricectomy with a CO2 laser for ingrown toenail after nail matrix staining. Dermatol Surg. 2005;31(3):302-305.


