Impact of Trauma

“Road Rash”
Clad only in shorts, T-shirt, and helmet, a 21-year-old man was involved in a motorcycle accident. He sustained “road rash”—diffuse multiple body abrasions, lacerations, and contusions—particularly on the extremities. Abrasions about the chest wall and abdominal region were also noted. Other injuries included a closed right clavicle shaft fracture and a nondisplaced open fracture of the dorsal aspect of the right olecranon.
Emergent total body irrigation and debridement were performed; pulse lavage and scrub brushes were used. All wounds were dressed with bacitracin ointment, Adaptec, and 4 3 4-in gauze pads.
Postoperative wound care included bedside dressing changes for the first few days. Gradually, some of the wounds were left open to the air. An electric fan directed at the patient helped dry the wounds and ease the pain. Daily, soothing whirlpool treatments were initiated in the hospital and continued as outpatient therapy.
The patient recovered remarkably well; no infections developed. Physical therapy of the right elbow and right knee prevented range-of-motion loss secondary to scarring and contractures. The patient was told to apply either cocoa butter or vitamin E cream to his wounds to decrease scar formation and discoloration.
(Case and photograph courtesy of Dr Jack E. Cohen.)

Nail Gun Injury
While on the job, a 24-year-old construction worker accidentally shot a nail through his right index finger with a nail gun. Roentgenographic studies revealed no damage to the bone. No neurovascular deficit was noted on examination.
Ridges in the nail’s shaft prevented its being pulled out along the same route it went in. Thus, the patient was given digital block anesthesia, the head of the nail was cut off, and the nail was pushed all the way through and out of the finger.
A prophylactic oral antibiotic and a tetanus toxoid injection were given. Healing was uneventful, and the finger remained functional.
(Case and photograph courtesy of Joe R. Monroe, PA-C.)

Stab Wound
A 32-year-old man was brought to the emergency department after being stabbed in the right side of the neck with a broken piece of glass. The patient immediately underwent carotid angiography; the findings were normal.
Results of an indirect laryngoscopic evaluation and an esophageal examination ruled out injury to the larynx and the esophagus. A roentgenogram of the neck revealed the presence of air in the deep fascial tissue planes of the neck. The patient was otherwise hemodynamically stable.
Air in the neck tissue is a cause of concern, since it may lead to pneumomediastinum. Generally, air in fascial planes of the neck is caused by trauma; the condition also may occur secondary to neck surgery, dental extraction, or deep space infection. The underlying cause needs to be identified and treated.
This patient was observed in the intensive care unit. Within a few days, the air in the neck tissue planes resorbed, and the patient recovered.
(Case and image courtesy of Drs Achal Dhupa and Arunabh.)

Lisfranc Ligamental Injury
After a fall during a soccer match 2 weeks earlier, a 26-year-old woman had pain of the right midfoot, with moderate swelling. The pain was aggravated with a normal gait and alleviated with an antalgic gait, specifically with inversion of the right ankle such that most of the weight from heel-strike through toe-off transmitted forces from the lateral calcaneus through the fifth metatarsus to the fifth phalanx.
Two days before presentation, the patient had swelling and pain of the superior aspect of the right knee. This was presumed to be related to the antalgic gait.
Point tenderness was noted over the right midfoot. No plantar ecchymosis was evident. Results of squeeze, Thompson, anterior drawer, and talar tilt tests were negative. Further squeeze testing of the metatarsal rays elicited pain in the midfoot.
Anteroposterior radiographs of the right foot demonstrated a gap larger than 3 mm between the bases of the first and second metatarsals as well as between the first and second medial cuneiforms, with loss of alignment of the medial edge of the base of the second metatarsal with the medial edge of the medial cuneiform. This was a stage II sprain according to the Nunley and Vertullo classification.1 There was no fracture of the base of the second metatarsal.
Capsuloligamentous disruption of the Lisfranc joint is most often seen in patients who have sustained high-velocity trauma in motor vehicle crashes. However, it can also result from low-velocity twisting-type injuries that occur in athletes.2
A clinical diagnosis can be made on the basis of midfoot swelling and tenderness; plantar ecchymosis; and assessment of gait, medial longitudinal arch, and ability to bear weight on the toes. Pain on squeezing the metatarsal rays in frontal and coronal planes is diagnostic.
The evaluation of a suspected Lisfranc joint injury should include weight-bearing anteroposterior, oblique, and lateral radiographs of the foot.1 About 20% of Lisfranc joint injuries are missed on conventional radiographs, presumably because of lack of fracture or history to correlate with the findings.3
Treatment is based on the degree of separation between the bases of the first and second metatarsals and the relationship of the medial cuneiform:
•Stage I sprain (no diastasis or arch height loss) is treated with cast immobilization and protected weight bearing for 4 to 6 weeks.
•Stage II sprain (2- to 5-mm diastasis) is treated with immobilization and non–weight-bearing status, which in this patient consisted of a Jones splint, or short leg cast, and the use of crutches.
•Stage III sprain (greater than 5-mm diastasis and loss of arch height) is treated with open reduction and internal fixation, although some experts have advocated
this treatment in all stage II and III sprains in athletes to stabilize bony alignment and support of the arch.2
Patients with stage I and II sprains require follow-up with an orthopedic surgeon or podiatrist; those with stage III sprains and fractures require follow-up with a foot and ankle subspecialist.
REFERENCES:
1. Nunley JA, Vertullo CJ. Classification, investigation, and management of midfoot sprains: Lisfranc injuries in the athlete. Am J Sports Med. 2002;30:871-878.
2. Mullen JE, O’Malley MJ. Sprains—residual instability of subtalar, Lisfranc joints, and turf toe. Clin Sports Med. 2004;23:97-121.
3. Umans HR. Imaging sports medicine injuries of the foot and toes. Clin Sports Med. 2006;25:763-780.
(Case and image courtesy of Matthew J. Letizia, DO and Clayton Everline, MD.)

Skull Depression
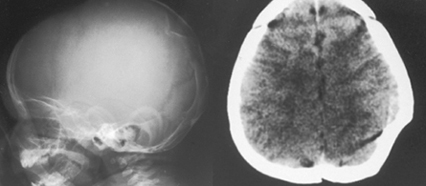
A 5-month-old boy’s head hit the floor after he tumbled from his mother’s arms. No injury was noted by the parents, and the infant immediately began to cry. His mother brought him to the emergency department just to be sure he was not seriously injured.
The asymptomatic child was alert and playful in the emergency department and had no seizures. A “ping-pong ball” depression was evident in the left parietal region. A skull indentation measuring 2.5 cm in diameter and 1.5 cm in depth was revealed in a tangential view roentgenogram. The CT scan disclosed no hematoma and no abnormality to the underlying brain.
Elevation of the depression was performed. Despite elevation of this type of skull fracture, post-traumatic epilepsy may develop. Injury to the underlying brain is thought to be the cause of this sequela.
(Case and images courtesy of Robert P. Blereau, MD.)
 Orbital Floor Fracture
Orbital Floor Fracture
Four hours before he arrived at the emergency department, a 33-year-old man had been struck in the face by a rock. A laceration and periorbital hematoma were noted on the left side of the patient’s face. He complained of pain in this area. There was no history of intraocular disease. The left globe was intact, and no neurologic deficit was found.
A supine radiograph demonstrated interruption and widening of the floor of the left orbit (A). An upright radiograph revealed fluid in the left maxillary sinus (B, arrow), consistent with hemorrhage. Orbital floor fracture was diagnosed.
An axial CT scan of the orbits demonstrated widening and increased density in the periorbital fat, which indicated soft tissue swelling (C). The scan was performed to evaluate the medial and lateral walls of the orbit, which were determined to be intact.
A direct coronal CT scan showed the depressed fracture of the orbit floor, hemorrhagic debris in the left maxillary sinus (D, white arrow), and intraorbital emphysema (D, red arrow); air was noted passing through the fracture from the left maxillary sinus into the left orbit. Coronal imaging is best for visualizing the roof and floor of the orbit. If direct coronal imaging cannot be performed, thin-section axial images can be obtained with generation of coronal reformats.
Orbital floor fractures may be caused by direct trauma to the inferior orbital rim, which results in buckling of the orbital floor. Fractures may also occur when rapidly increased intraorbital pressure is decompressed at the weakest point of the bony confines of the orbit.
Suspect an orbital fracture when a patient has a history of trauma, ecchymosis with or without edema of the lids, diplopia, hypoesthesia of the cheek (related to injury to the infraorbital nerve), or emphysema of the orbit or lids. Enophthalmos and ptosis of the globe indicate a large fracture.
Fractures of the orbit frequently involve the weakest part of the bony orbit—the lamina papyracea or medial wall. If the medial wall is involved, hemorrhagic debris is seen in the ethmoid complex, and air that emanates from the ethmoid results in intraorbital emphysema.
Fractures of the orbit roof and lateral wall are much less common. They can be complicated by cerebrospinal fluid leak and herniation of intracranial contents into the orbit; entrapment of the superior rectus muscle is rare.
Most orbital floor fractures heal without treatment, as in this case. Consider surgical repair in the event of complications, such as sensory disturbance as a result of injury of the infraorbital nerve, muscle entrapment when the inferior rectus herniates through the fracture defect, and enophthalmos from herniation of large portions of orbit contents into an adjacent sinus.
(Case and images courtesy of Drs Carol A. Lundin and Joel M. Schwartz.)


