Peer Reviewed
Severe Anemia Associated With Intracranial Hemorrhage in an Infant
Authors:
Lin Lin Kin, MD, DCH, and Mrudula Premkumar, MD
Department of Pediatrics, BronxCare Health System, Bronx, New York
Citation:
Kin LL, Premkumar M. Severe anemia associated with intracranial hemorrhage in an infant. Consultant. 2019;59(7):218-220.
A 5 ½-month-old girl was referred to the pediatric emergency department (ED) by her primary care provider (PCP) for a temperature of 39.2°C. The infant’s mother had taken her to the PCP for evaluation of fever and constipation. The mother said that the infant had felt warm for the past 2 days and had had cough, congestion, and rhinorrhea. The infant had bowel movements once every 2 to 3 days and had been feeding and urinating well.
History. The girl had been born via elective cesarean delivery at 29 weeks of gestation due to decreased fetal movement. Apgar scores were 6 at 1 minute and 8 at 5 minutes. Severe intrauterine growth restriction was noted at birth due to poor placental perfusion and placental calcifications.
She had been admitted to the neonatal intensive care unit (NICU) for 2 months for respiratory distress, during which time multiple sepsis workups were performed and antibiotics administered, but all blood culture results had been negative for bacteria. She also had received 3 transfusions of packed red blood cells (PRBC), epoetin alfa for anemia of prematurity, phototherapy for jaundice, and ursodiol for cholestasis.
Ultrasonography of the head done while in the NICU had shown an intraparenchymal bleed of 1.5 cm in the right occipitoparietal area, with no ventriculomegaly or midline shift. Follow-up head sonograms and magnetic resonance imaging without contrast of the brain after discharge from the NICU had shown resolution of the bleed. She also had had a left inguinal hernia repair at 3 months of age with no complications or bleeding problems.
Physical examination. At the current presentation, her temperature was 39.1°C, heart rate was 166 beats/min, respiratory rate was 48 breaths/min, and oxygen saturation was 95%. General physical examination revealed a very pale infant who was awake and not in acute distress. Her anterior fontanel was open, and sutures splayed. S1 and S2 heart sounds were present but with no murmur; capillary refill was less than 2 seconds. She had normal tone and equal power in all limbs, and no cranial nerve deficits were noted.
Diagnostic tests. Results of a complete blood cell count showed that the hemoglobin level was only 5.6 g/dL (reference range, 12-16 g/dL) and the platelet count was 341 × 103/µL. The white blood cell count was normal. Subsequent repeated hemoglobin levels were 5 g/dL and then 4.6 g/dL. After consultation with a pediatric hematologist, the patient was admitted to the pediatric unit for observation and for repeated hemoglobin tests, a parvovirus panel, and monitoring of epoetin alfa levels. Blood type and cross-match testing was done, and PRBC transfusion was initiated. Blood and urine culture results were negative for bacteria.
Because of the significant fever and anemia and the patient’s history of an intracranial bleed at birth, head ultrasonography was done, which showed a large, right-sided, extra-axial hematoma overlying the temporal, parietal, and likely occipital lobes. The hematoma appeared lentiform on coronal images, although the distribution on sagittal images suggested blood in the subdural space rather than the epidural space. Intraventricular hemorrhage was noted in the right lateral ventricle with a 3-mm midline shift from right to left at the foramen of Monro (Figure 1).
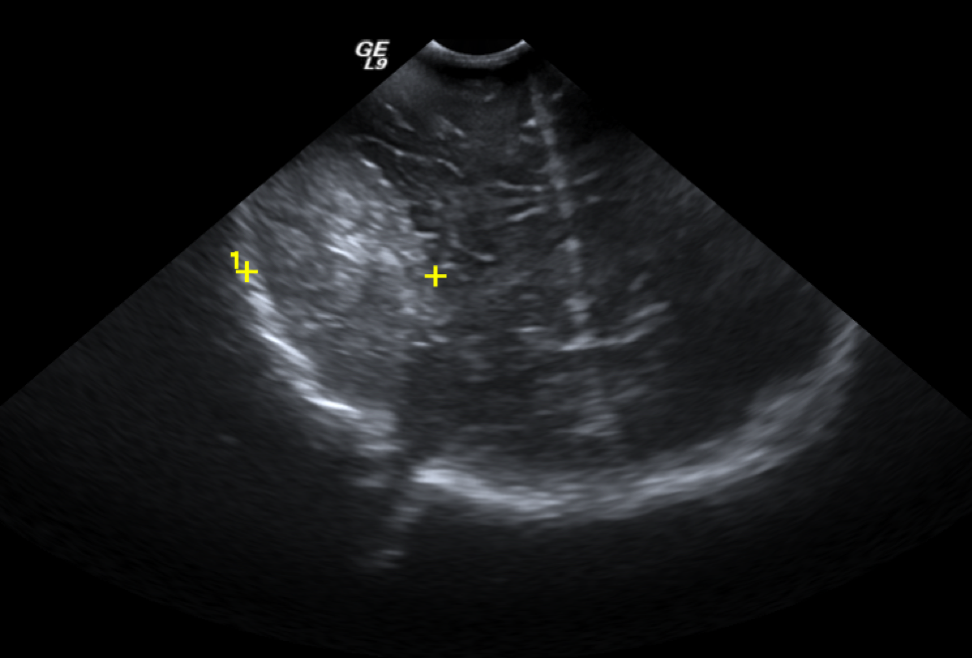
Figure 1. Head ultrasonogram showing large, right-sided, extra-axial hematoma overlying the temporal, parietal, and likely occipital lobes.
Computed tomography (CT) of the head without contrast showed a large, right-sided epidural hematoma overlying the frontal, temporal, and parietal lobes with mass effect and midline shift from right to left (Figure 2).

Figure 2. Noncontrast CT of the head showed a large, right-sided epidural hematoma overlying the frontal, temporal, and parietal lobes with mass effect and midline shift from right to left.
Upon further questioning, the mother reported retrospectively that the girl had a history of a fall 5 days prior to presentation. There had been no loss of consciousness, vomiting, or abnormal movements. The mother said that she had called and informed the PCP, who advised her to observe the infant and to take her to the ED if there were any changes in mental status, vomiting, or seizures.
The patient was intubated to protect the airway and was transported to the neurosurgical unit at the tertiary hospital, where she underwent evacuation of the hematoma, which was subdural according to the operative report. She was discharged home in stable condition.
Discussion. The presence of fever and anemia are common in patients with intracranial hemorrhage. Anemia is present in up to 25% of cases at admission and is associated with larger hematoma volumes. PRBC transfusion in these patients has been found to be associated with improved survival, although the ideal target hemoglobin level has not been determined.1
There are 4 types of intracranial hemorrhages: epidural, subdural, subarachnoid, and intracerebral.
Epidural hemorrhage refers to bleeding between the dura mater and the skull. The bleeding is rapid, usually from dual arteries or veins, may or may not present with loss of consciousness then a lucid period, followed by loss of consciousness with increased in intracranial pressure, abnormal posturing, and an ipsilateral dilated pupil, and finally death from brainstem herniation.
In a subdural hematoma, blood accumulates between the dura mater and the arachnoid mater. It can be classified as acute, subacute, or chronic. A subdural hematoma usually is venous but can still be life-threatening when acute or massive. The mortality rate can approach 80%.2 Most acute subdural hematomas are hyperdense compared with the cerebral cortex on CT images, such as in our patient’s case as demonstrated in Figure 2. They became isodense or hypodense 7 to 10 days later.3
Subarachnoid hemorrhage is bleeding into the subarachnoid space, between the arachnoid mater and the pia mater. Subarachnoid hemorrhages are very dangerous; approximately half of all people with subarachnoid hemorrhages die from them, and a large percentage of those who survive sustain some form of brain damage.4
Intracerebral hemorrhage, also known as a cerebral bleed, is bleeding within the brain tissue or ventricles. It is most common in premature neonates at birth and also can occur with head trauma, cerebral aneurysms, and bleeding disorders. Symptoms are mostly acute with a sudden onset of headache, weakness, paresis/paralysis, confusion, and delirium. Older children and adults can present with dysarthria, loss of balance and coordination, lethargy, and loss of consciousness. Fever is also common.
Our patient, who had multiple medical problems including anemia of prematurity, was admitted for evaluation of a fever and severe anemia. A severe drop in the hemoglobin level, as in this patient’s case, should prompt clinicians to look for serious potential causes. Moreover, not all lentiform intracranial hemorrhages are epidural hemorrhages. Our patient had an acute subdural bleed and was clinically stable initially, but she had a progressive drop in hemoglobin due to a massive subdural hemorrhage causing midline shift.
- Caceres JA, Goldstein JN. Intracranial hemorrhage. Emerg Med Clin North Am. 2012;30(3):771-794.
- Meagher RJ, Young WF. Subdural hematoma. Medscape. https://emedicine.medscape.com/article/1137207-overview#a7. Updated July 26, 2018. Accessed May 13, 2019.
- Connolly ES Jr, McKhann GM II. Contemporary management of subdural hematomas. Neurosurg Clin N Am. 2017;28(2):ix.
- van Gijn J, Kerr RS, Rinkel GJE. Subarachnoid haemorrhage. Lancet. 2007;369(9558):306-318.


