Peer Reviewed
Crusted Scabies in a Patient With Cancer
AUTHORS:
Mindy M. Sampson, DO
University of South Florida Morsani College of Medicine, Tampa, Florida
Dhyana Sankar, MD
University of South Florida Morsani College of Medicine, Tampa, Florida
Julie Gibbs, MD
University of South Florida Morsani College of Medicine, Tampa, Florida
Olga Klinkova, MD
University of South Florida Morsani College of Medicine and Moffitt Cancer Center, Tampa, Florida
John N. Greene, MD
University of South Florida Morsani College of Medicine and Moffitt Cancer Center, Tampa, Florida
CITATION:
Sampson MM, Sankar D, Gibbs J, Klinkova O, Greene JN. Crusted scabies in a patient with cancer. Consultant. 2020;60(2):60-61. doi:10.25270/con.2020.02.00008
A 78-year-old man was admitted to the hospital after receiving a new diagnosis of B-cell acute lymphoblastic leukemia (ALL). He reported having fevers, weakness, and a pruritic rash that had been present for at least 2 months.
History. He had recently been admitted to another facility for confusion, where he had been treated for a urinary tract infection and had been found to be anemic, ultimately leading to the diagnosis of ALL. He had not yet started any treatment.
His primary concern at the current visit was a rash that involved his trunk, extremities, buttocks, and groin area. It had become increasingly painful and pruritic over the past 2 weeks. He described the initial development of small red bumps that had progressed to a thickened scaling rash. He also noticed several areas within the rash that had developed fissures and were draining clear fluid. His wife also had recently developed a similar pruritic rash. He denied any recent diarrhea, oral ulcers, cough, dyspnea, urinary tract symptoms, or focal neurologic symptoms.
His medical history was notable for diabetes mellitus type 2 and Parkinson disease. He had been taking carbidopa-levodopa, ropinirole, donepezil, primidone, and sitagliptin for several years. He had recently started diphenhydramine to treat the itching and pregabalin to treat the pain. He had no known drug allergies. Regarding his social history, he had moved from Illinois to Florida at the age of 54. He consumed 3 alcoholic beverages a night and denied any illicit drug or tobacco use. He had previously been a car manufacturer, and he denied any recent travel.
Physical examination. At presentation, the patient appeared chronically ill and was cachectic. Blood pressure was 129/70 mm Hg, pulse was 88 beats/min, temperature was 38.2°C, and respiratory rate was 24 breaths/min. Physical examination revealed diffuse erythema with excoriated papules covering most of the body. Areas of lichenification and thick yellow crusting were present in the finger webs and on the dorsal hands. The buttocks and inguinal creases had developed thick yellow crusting with areas of denuded skin (Figure 1). There was no lymphadenopathy.

Figure 1. Cutaneous examination of the buttocks showing yellow crusting with denuded skin.
Diagnostic tests. The peripheral white blood cell count was 3530/µL (reference range, 4000-10,900/µL) with a neutrophil count of 1270/µL(reference range, 1800-7800/µL), a lymphocyte count of 600/µL (reference range, 1100-3500/µL), and an eosinophil count of 1480 (reference range, 0-450/µL). Results of a comprehensive metabolic panel were significant for a low albumin level of 1.9 g/dL (reference range, 3.5-5.2 g/dL); otherwise, liver enzyme levels, kidney function, and electrolyte levels were normal.
Blood cultures and urine cultures were negative for pathogens. Chest radiographs were negative for infiltrates or consolidations. Due to the patient’s immunocompromised status and fevers, he initially was started on broad antimicrobial coverage with vancomycin and cefepime.
Skin scrapings and biopsy from the fingers and trunk were performed, the results of which were positive for mites and scybala (fecal pellets) on microscopic examination (Figure 2). Results of polymerase chain reaction testing for herpes simplex virus (HSV) were positive from a swab taken of an ulcerative lesion on the chest. Superficial skin cultures taken from areas of denuded skin revealed methicillin-sensitive Staphylococcus aureus. He received a diagnosis of crusted scabies with secondary methicillin-sensitive S aureus and HSV infections.
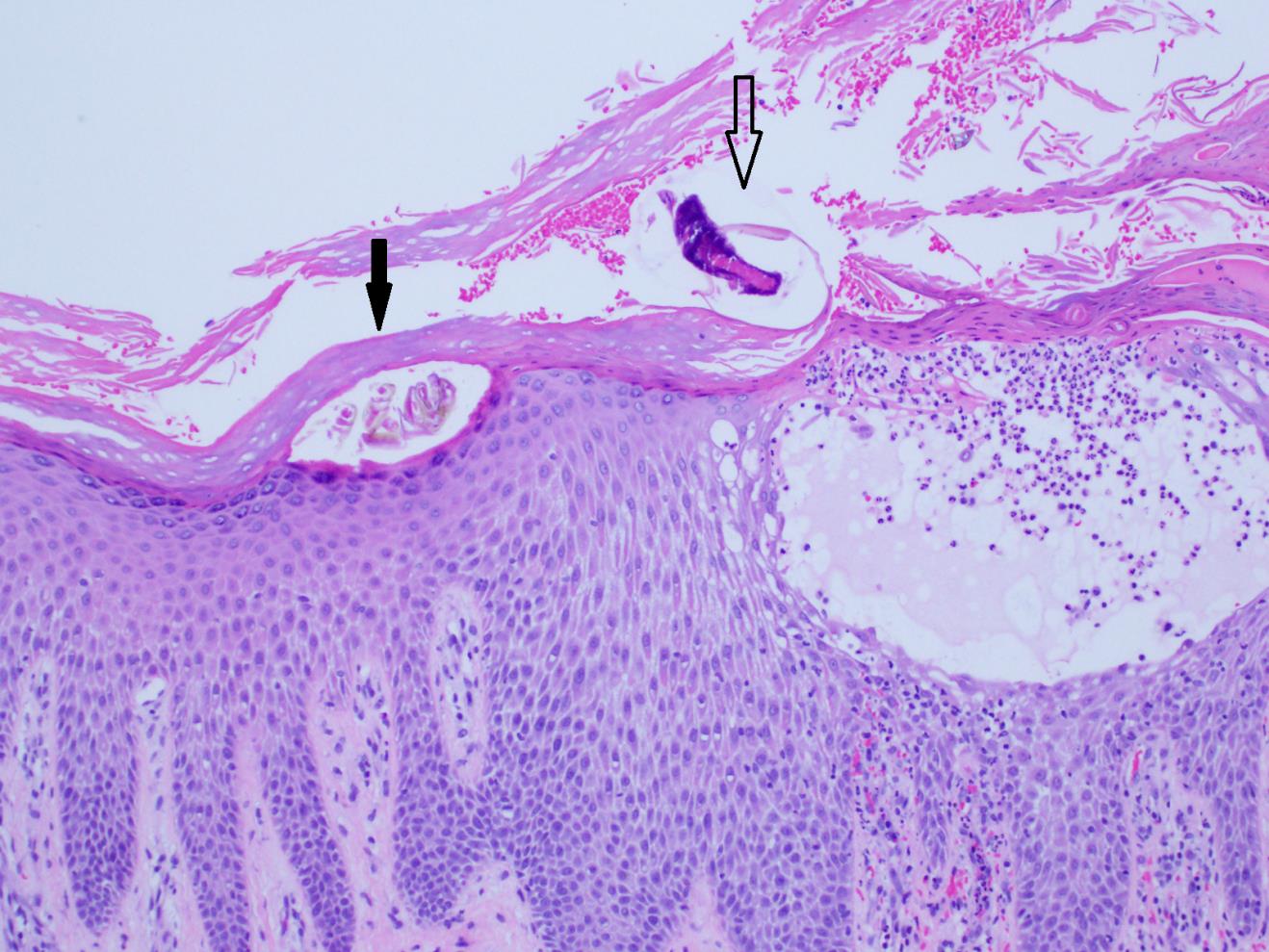
Figure 2. Histopathologic examination revealed a scabetic mite within the stratum corneum (open arrow) and a scybalum (black arrow). The epidermis showed acute spongiosis with a mixed infiltrate containing neutrophils and eosinophils.
Outcome of the case. The patient was treated with permethrin cream, 5%, which was applied from the neck down. He also received 1 dose of ivermectin, 0.2 mg/kg. The HSV infection was treated with oral famciclovir, 500 mg twice daily for 7 days. While awaiting finalization of cultures, and out of concern for secondary bacterial infection, broad-spectrum antibiotics were continued. Over the next 2 days his health continued to decline, however, and he chose to pursue comfort care and was discharged to hospice.
In our case, infection control was notified to prevent the spread of scabies. Our patient had potentially been infested for months and had been to at least 2 other medical facilities, possibly resulting in institutional outbreaks given the contagious nature of scabies. In our institution, 34 health care workers were found to have had contact with the patient, and 18 opted to be treated with permethrin cream. None of the health care workers developed scabies.
Discussion. Crusted scabies is characterized by a hyperinfestation of the skin by the mite Sarcoptes scabiei. For crusted scabies to manifest, a patient must be infested with millions of mites, which differentiates it from a typical scabies infestation, wherein a patient may be infested with as few as 5 to 15 mites.1,2 Crusted scabies mostly affects immunocompromised persons such as those with advanced HIV infection and hematologic malignancies.3,4
Given that the infestation is highly contagious, scabies can spread easily among individuals who are living in close quarters or crowded living spaces, such as nursing homes and prisons.1 This disease is transmitted by a direct skin-to-skin contact of an infested person. Skin manifestations typically occur 1 to 2 months after being infested; however, the incubation period may be as short as 1 week in crusted scabies due to a larger infestation of the mite.1 In crusted scabies, the skin appears grossly thickened with large hyperkeratotic crusts involving the palms and soles, trunk, flexor surfaces of the elbows and knees, and the scalp.4,5
The diagnosis of scabies is confirmed based on the identification of mites, eggs, eggshell fragments, or mite feces on a microscopic examination of skin samples.6 The differential diagnosis of crusted scabies includes psoriasis, eczema, keratosis follicularis (also known as Darier disease), ichthyosis, eczema herpeticum, and cutaneous T-cell lymphoma.6 Secondary bacterial infections frequently occur, with common pathogens being S aureus and Streptococcus pyogenes.3,5,7
When treating crusted scabies, it is strongly recommended to use combination therapy with systemic and topical agents. A standard combination regimen is topical permethrin cream, 5%, and oral ivermectin, 200 µg/kg/dose, given on days 1, 2, 8, 9, and 15.2,6,8,9
Recognition of crusted scabies is critical to allow for aggressive treatment of the patient and to prevent spread of infestation to other patients and health care workers. Because its presentation differs from classic scabies, this condition can be easily misdiagnosed. It is particularly important for the providers working in the institutional settings or treating immunocompromised patients to be aware of this condition.4,10
- Executive Committee of Guideline for the Diagnosis and Treatment of Scabies. Guideline for the diagnosis and treatment of scabies in Japan (third edition): Executive Committee of Guideline for the Diagnosis and Treatment of Scabies. J Dermatol. 2017;44(9):991-1014.
- Salavastru CM, Chosidow O, Boffa MJ, Janier M, Tiplica GS. European guideline for the management of scabies. J Eur Acad Dermatol Venereol. 2017;31(8):1248-1253.
- Romani L, Steer AC, Whitfeld MJ, Kaldor JM. Prevalence of scabies and impetigo worldwide: a systematic review. Lancet Infect Dis. 2015;15(8):960-967.
- Ghosh T, Jandhyala D, Bhatti MM, Pritt BS. The brief case: crusted scabies in a leukemic patient following a stay in a long-term acute care facility. J Clin Microbiol. 2017;55(5):1233-1236.
- McCarthy JS, Kemp DJ, Walton SF, Currie BJ. Scabies: more than just an irritation. Postgrad Med J. 2004;80(945):382-387.
- Chosidow O. Scabies. N Engl J Med. 2006;354(16):1718-1727.
- Hay RJ, Steer AC, Engelman D, Walton S. Scabies in the developing world—its prevalence, complications, and management. Clin Microbiol Infect. 2012;18(4):313-323.
- Mounsey KE, McCarthy JS. Treatment and control of scabies. Curr Opin Infect Dis. 2013;26(2):133-139.
- Currie BJ, McCarthy JS. Permethrin and ivermectin for scabies. N Engl J Med. 2010;362(8):717-725.
- Institutional settings. Centers for Disease Control and Prevention website. https://www.cdc.gov/parasites/scabies/health_professionals/institutions.html. Reviewed November 2, 2010. Accessed October 9, 2019.


