Peer Reviewed
Choledochal Cyst
Authors:
Nicole Zeky, DO; Emily Klepper, MD; and Elizabeth McDonough, MD
Pediatric Residency Program, Our Lady of the Lake Children’s Hospital, Baton Rouge, Louisiana
Citation:
Zeky N, Klepper E, McDonough E. Choledochal cyst [published online October 17, 2019]. Gastroenterology Consultant.
A 3-year-old girl presented to the emergency department (ED) with abdominal pain of 1 week’s duration. She also had had nonbloody and nonbilious emesis. She had a history of chronic constipation, so her mother had tried to give the girl an enema. When the enema did not produce a bowel movement and did not seem to help her daughter’s pain, she brought her to the ED.
Physical examination. On initial examination, the girl was in no acute distress. Vital signs were normal, and she was afebrile. She was awake and alert and had moist mucous membranes. She had no scleral icterus. Cardiac examination revealed a normal heart rate and rhythm. Her lungs were clear to auscultation bilaterally. Her abdomen was soft and nondistended with no palpable masses, but she had diffuse abdominal pain without guarding. Her skin was warm and clear of rashes, with normal capillary refill.
Diagnostic tests. Initial laboratory test results showed elevated levels of transaminases, γ-glutamyltransferase (GGT), and lipase (Table). The total bilirubin level was within normal limits, but the direct bilirubin level was minimally elevated at 0.5 mg/dL.
Table. Pertinent Laboratory Test Values on Admission | ||
| Patient’s Value | Reference Range |
GGT | 140 U/L | 6-24 U/L |
Alanine aminotransferase | 212 U/L | 2-35 U/L |
Aspartate aminotransferase | 198 U/L | 16-63 U/L |
Lipase | 1523 U/L | 8-78 U/L |
α1-Fetoprotein | 0.4 ng/mL | >10 ng/mL |
CA 19-9 | 147 U/mL | 0-37 U/mL |
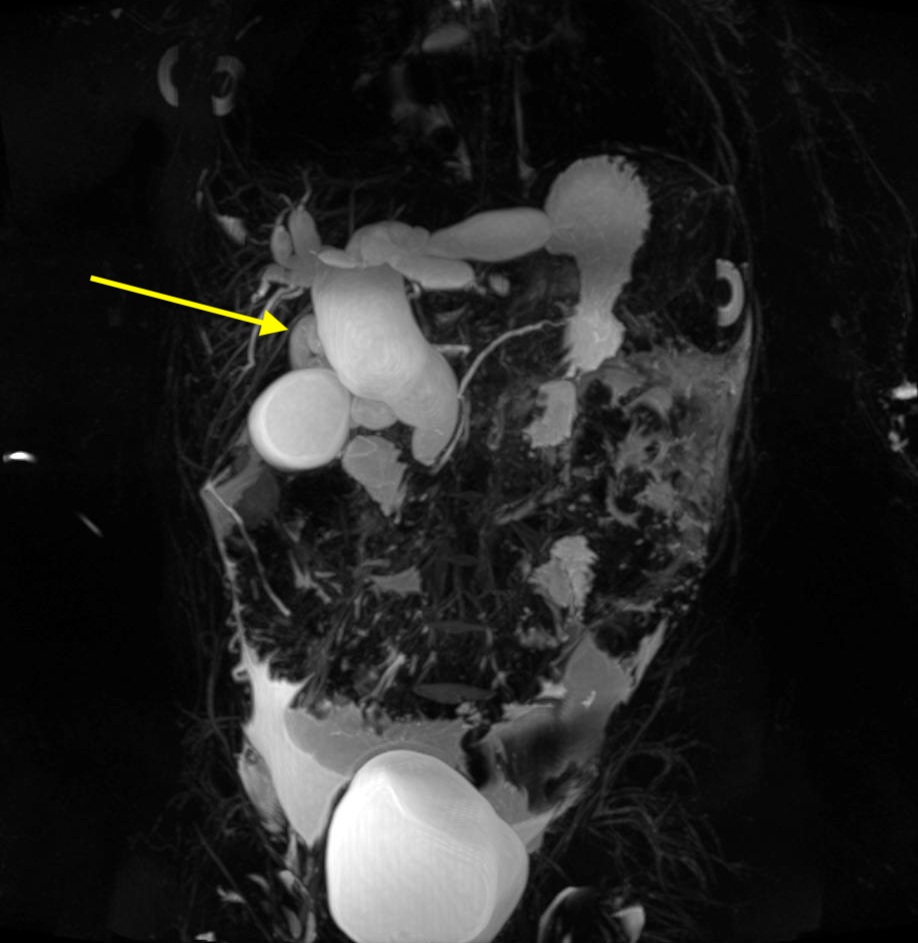
Further workup was ordered to evaluate for biliary disease. Computed tomography scans of the abdomen showed intrahepatic and extrahepatic dilation of the bile ducts, with a common bile duct width of 2.8 cm—findings that were concerning for choledochal cyst. To better evaluate the cyst, magnetic resonance cholangiopancreatography (MRCP) scanning was performed, the results of which confirmed a type IVa choledochal cyst (Figures 1 and 2). Additional laboratory test results showed an elevated cancer antigen 19-9 (CA 19-9) level but a normal α1-fetoprotein level (Table).

Treatment. She was taken to the operating room for excision and Roux-en-Y hepaticojejunostomy. During the procedure, the choledochal cyst was found to encompass the entire length of the extrahepatic biliary tree and bilateral intrahepatic systems, consistent with a type IVa biliary cyst. Tissue was sent for pathology.
Discussion. Choledochal cysts are dilations that form along the biliary tree.1,2 Biliary cysts are rare findings, with a reported annual incidence of 1 in 13,500 births in the United States.3 A 3 to 1 female predominance has been reported.1,4
The classic presentation of choledochal cysts is the triad of abdominal pain, jaundice, and abdominal mass.5,6 However, only 20% of patients will present in this manner.1 Infants with choledochal cysts usually present with cholestatic jaundice.6 More commonly, cysts tend to be incidental findings during the evaluation of persistent abdominal pain.5 Most patients will present in the first decade of life, with only 20% of patients presenting in adulthood.1
The pathogenesis of choledochal cysts is unknown.3,5 It had been thought previously that a single, common channel develops that is part of the mature pancreatic duct and biliary duct.4 This common channel allows the reflux of pancreatic enzymes into the biliary duct, causing inflammation and subsequent dilation of the biliary tree.4 Another theory holds that these cysts are simply congenital, where the epithelial cells of the biliary duct go through increased proliferation, leading to ductal dilation.3
There are 5 subtypes of choledochal cysts.3-5 Type I, the most common subtype, consists of cystic dilation of the common bile duct.6 Type II is described as diverticula of the extrahepatic bile duct only.3-5 Type III, also called choledochocele, is described as dilation of the intraduodenal portion of the common bile duct only.3-5 Type IV is subcategorized as type IVa and type IVb.5 Our patient had a type IVa choledochal cyst, which is characterized as having multiple intrahepatic and extrahepatic dilations.3-5 Type IVb consists of only extrahepatic cystic dilations of the biliary ducts.3-5 Type V consists of multiple intrahepatic dilations only, also known as Caroli disease.3-5
The diagnosis choledochal cyst must be considered when evidence of obstructive jaundice in infants is present.6 Abdominal ultrasonography might show evidence of a cystic mass near the porta hepatis.1,6 MRCP, however, is the imaging modality of choice for classifying the cyst in preparation for surgical resection.4,6
A Roux-en-Y hepaticojejunostomy with complete cyst excision is the treatment of choice.1 Patients who do not undergo surgery have an increased risk of developing hepatic fibrosis, pancreatitis, acute cholangitis, biliary rupture, peritonitis, portal hypertension, and cholangiocarcinoma.1,2 The success rate of Roux-en-Y hepaticojejunostomy is as high as 90% with surgical removal.4 Postsurgical complications can include stenosis of the anastomosis site, pancreatitis, and acute cholangitis.1,2
Type I and IV cysts have an increased risk of development of cholangiocarcinoma if any residual cystic tissue is left behind, highlighting the importance of early detection and surgical removal.4,5 The average age at diagnosis of cholangiocarcinoma in patients with a previously diagnosed biliary cyst was in the third decade of life, approximately 15 years before the general population without this risk factor.2 Tumor markers such as CA 19-9 and α1-fetoprotein are nonspecific inflammatory markers that can be monitored postoperatively; increased levels might be a sign that residual cystic tissue was left operatively.1,4 Approximately 85% of patients with cholangiocarcinoma will have an elevated CA 19-9 tumor marker level; therefore, this might be a clue that residual tissue from the biliary cyst has remained.4
Outcomes of the case. Pathology results were consistent with a choledochal cyst and were negative for malignancy. The patient was doing well at discharge, tolerating a normal diet with no abdominal pain. Six months postoperatively, laboratory test results showed that her transaminase levels had normalized. Right upper-quadrant ultrasonography findings showed no biliary ductal dilation. Tumor marker tests were not repeated.
- Forny DN, Ferrante SMR, Silveira VGd, Siviero I, Chagas VLA, Méio IB. Choledochal cyst in childhood: review of 30 cases. Rev Col Bras Cir. 2014;41(5):331-335.
- Singham J, Yoshida EM, Scudamore CH. Choledochal cysts: part 3 of 3: management. Can J Surg. 2010;53(1):51-56.
- Singham J, Yoshida EM, Scudamore CH. Choledochal cysts: part 1 of 3: classification and pathogenesis. Can J Surg. 2009;52(5):434-440.
- Jabłońska B. Biliary cysts: etiology, diagnosis and management. World J Gastroenterol. 2012;18(35):4801-4810.
- Mieli-Vergani C, Hadžic N. Biliary atresia and neonatal disorders of the bile ducts. In: Wyllie R, Hyams JS, Kay M, eds. Pediatric Gastrointestinal and Liver Disease. 5th ed. Philadelphia, PA: Elsevier; 2016:chap 69.
- Brumbaugh D, Mack C. Conjugated hyperbilirubinemia in children. Pediatr Rev. 2012;33(7):291-302.


