Peer Reviewed
Cervical Teratoma in a Newborn
AUTHOR:
Nicole A. Bailey, MD1,2,3
AFFILIATIONS:
1Division of Neonatology, Nicklaus Children’s Hospital, Miami, Florida
2Florida International University Herbert Wertheim College of Medicine, Miami, Florida
3Division of Neonatology, Kidz Medical Services, Miami, Florida
CITATION:
Bailey NA. Cervical teratoma in a newborn. Consultant. 2021;61(9):e31-e34. doi:10.25270/con.2020.11.00012
Received June 14, 2020. Accepted October 26, 2020. Published online November 30, 2020.
DISCLOSURES:
The authors report no relevant financial relationships.
CORRESPONDENCE:
Nicole A. Bailey, MD, Nicklaus Children's Hospital, Division of Neonatology, Advanced Pediatric Care Pavilion, 4th Floor, 3100 SW 62nd Ave, Miami, FL 33155 (nicole.bailey@nicklaushealth.org)
A boy with a prenatally diagnosed large neck mass was born early via cesarean delivery at 36 weeks and 5 days of gestation. The pregnancy had been otherwise uncomplicated. The maternal prenatal laboratory test results had been unremarkable, except for an unknown group B streptococcus status.
Her labor had been spontaneous, and her membranes had been ruptured for 7 hours. An ex utero intrapartum treatment procedure was successfully performed to secure the neonate’s airway after delivery of the head but prior to delivery of the entire body. Pediatric surgeons, who had been consulted prenatally, were available in the delivery room in the event that assistance with intubation and/or emergency tracheostomy were needed.
The neonate’s Apgar scores were 8 at 1 minute and 9 at 5 minutes. His birth weight was 2715 g (34.8 percentile), his length was 50 cm (80th percentile), and his head circumference was 34.5 cm (82.1 percentile). The neonate was stabilized in the delivery room and then admitted to the level 3 neonatal intensive care unit (NICU) at a community hospital. Umbilical lines were placed. The patient was then transferred to a NICU at a local children’s hospital at several hours of life for subspecialty evaluation.
Physical examination. Upon admission to the children’s hospital, the patient’s temperature was 37 °C, his heart rate was 153 beats/min, his respiratory rate was 50 breaths/min, and his oxygen saturation was 95% on a ventilator set at 30% fraction of inspired oxygen. Physical examination findings were notable only for a large anterior lobulated neck mass extending from the right side of neck below the right ear to across the midline (Figures 1 and 2). There was no heart murmur or other gross anomalies.


Diagnostic tests. A complete blood cell count showed normal findings, including a white blood count of 6000/µL, a hematocrit level of 55%, and a platelet count of 285 × 103/µL. His electrolyte levels and hepatic function panel test results were also normal. Results of his first thyroid function tests were normal on day of life 7. Additionally, his α1-fetoprotein (AFP) level was normal at 33,312 ng/mL (33,312 µg/L). His β-human chorionic gonadotropin level was reported as less than 2.39 mIU/mL (reference range, 0-1.06 mIU/mL). The lactate dehydrogenase value was 1382 U/L (reference value, up to 2100 U/L).
Radiographs of the neonate’s chest and abdomen showed clear lungs, a normal heart size, and a nonobstructive bowel gas pattern. Ultrasonography of the neck showed a large, complex mass with multicystic and solid components in the right neck. Findings of head ultrasonography and echocardiography were normal.
Differential diagnosis. The differential diagnosis for a large neck mass includes lymphadenopathy, hemangioma, goiter, vascular malformation, cystic hygroma, cervical teratoma, neuroblastoma, ectopic thymus, rhabdomyosarcoma, and sternocleidomastoid tumor (fibromatosis colli).
Clinical course, evaluation, and management. A computed tomography (CT) scan (Figure 3) showed areas of fat and punctate dystrophic areas of calcification seen through the solid and cystic component of the mass. Displacement of the airway was noted. A magnetic resonance imaging (MRI) scan (Figure 4) showed a solid and cystic mass in the neck that involved multiple compartments with significant mass effect on the airway. There was no extension into the spine, brain, or mediastinum. There were associated calcifications.


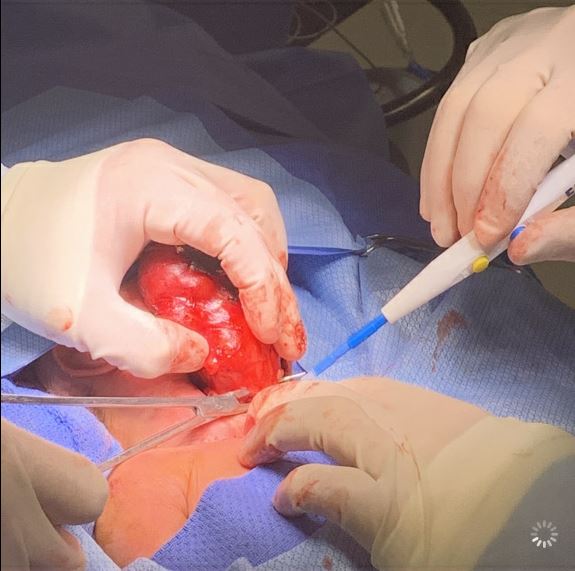
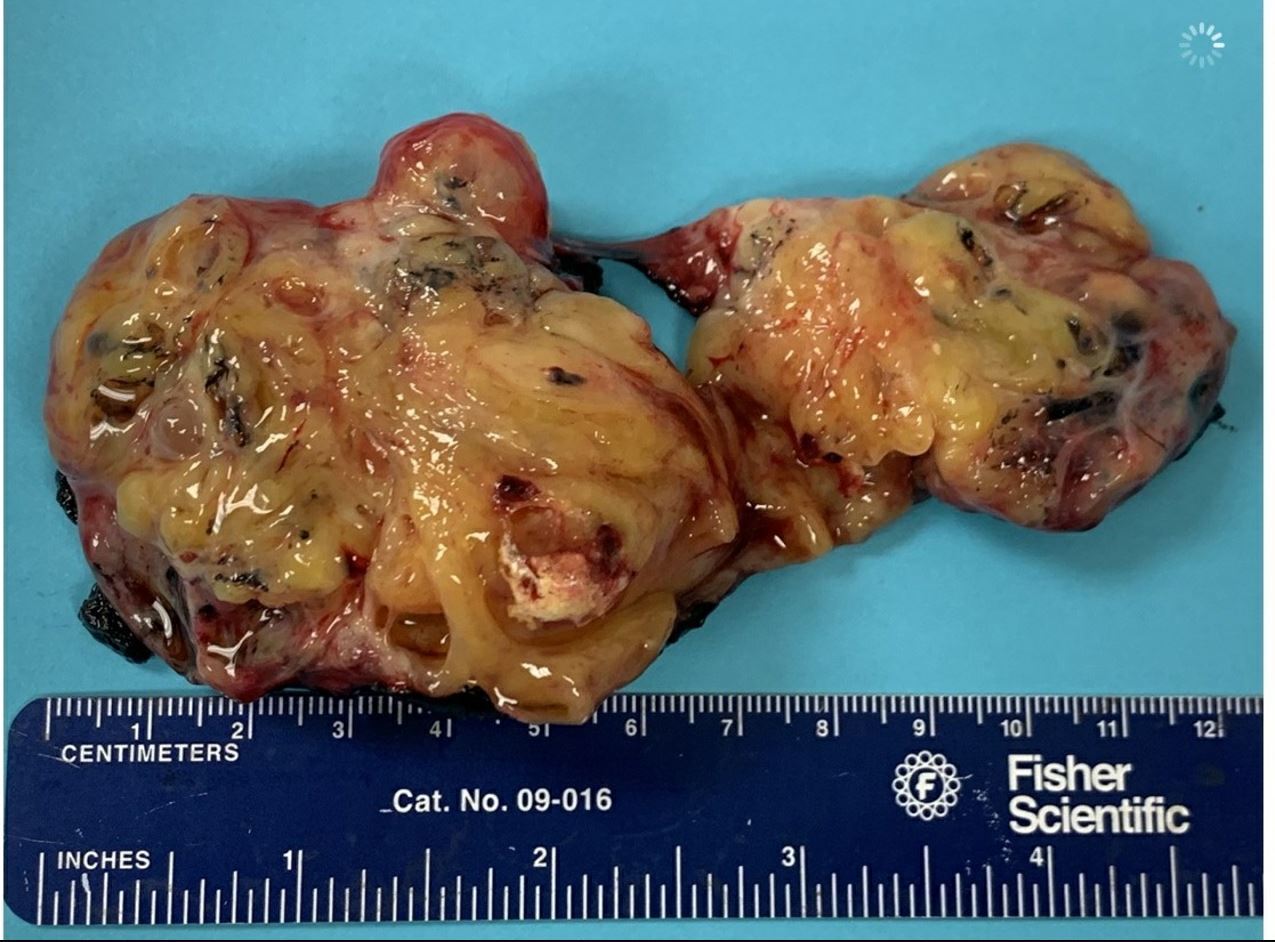
The patient underwent resection of the cervical mass on day of life 6 (Figures 5-7). The mass was noted to be intimately associated with the larynx and trachea. Careful dissection was done to free the tumor from this region. There was no evidence of damage to the trachea, larynx, or major nerves and vessels during the surgical procedure. However, a thyroid gland was not visualized during the procedure. The final surgical pathology report showed an immature teratoma replacing the thyroid gland, and regional cervical lymph nodes replaced by teratoma. There was no evidence of metastasis.

On postoperative day 1, an extubation attempt was made, but the extubation failed within 20 minutes due to severe respiratory distress, and the patient was immediately reintubated. Rigid bronchoscopy was performed several days later, and the results showed a vestibular fold granuloma with some ulceration and erythema. There was no tracheomalacia. The patient was successfully extubated to room air on postoperative day 7 after having been given 4 doses of dexamethasone to facilitate the extubation.
Several days postoperatively, routine blood test results showed that the patient had subclinical hypothyroidism and transient hypocalcemia. However, subsequent laboratory test results within a week after surgery indicated normalization of thyroid function and calcium levels without the need for supplementation. Later, ultrasonography of the thyroid showed an absent right lobe of the gland. The left thyroid lobe was present and measured 1.4 × 0.8 × 0.6 cm. A hematologist/oncologist was consulted and recommended observation and following of tumor markers.
Several weeks postoperatively, the patient remained hospitalized to work on oral feedings. A swallow study was also performed at nearly 1 month of age, and the results showed no aspiration with an extra-slow-flow nipple. The infant was eating all feeds by mouth at 1 month of age and was discharged home at that time.
Several months after discharge, the patient continues to do well. He has no swelling or problems with the right neck surgical scar. He continues outpatient follow-up with specialists in pediatric surgery, endocrinology, and hematology/oncology.
Discussion. Cervical teratomas are rare benign tumors in neonates, comprising 3% to 5% of all teratomas in children.1,2 The vast majority of teratomas in newborns contain immature tissue components but are still considered benign.3 Teratomas are derived from all 3 germ cell layers—ectoderm, mesoderm, and endoderm.4,5 Histologic features may include cystic or solid areas as well as mature or immature components.1
Teratomas are more commonly found in the sacrococcygeal region, followed by the ovaries, testes, anterior mediastinum, retroperitoneum, and less commonly, the head and neck.2 While the exact etiology of cervical teratomas is unknown, they are usually diagnosed prenatally on ultrasonography and can present with polyhydramnios. They can grow very rapidly in late gestation.6 Postnatally, facial disfigurement, airway obstruction, and respiratory distress are common complications.
Cervical teratomas tend to be more anterior and midline in the neck, whereas lymphangiomas and hemangiomas are more posterior and lateral in location.7 Congenital soft-tissue sarcomas of the neck and goiter are very rare but can mimic congenital cervical teratomas.7 Preoperative imaging can assist in differentiating these tumors and should include ultrasonography, CT, and/or MRI. The presence of multiple calcified foci on radiographic imaging is highly consistent with the diagnosis of a teratoma.1 Preoperative thyroid function tests should be done in all patients with cervical teratomas, since these tumors frequently contain thyroid tissue.1 Hypothyroidism also can be seen postoperatively.1
Complete surgical excision is the treatment for congenital cervical teratomas. Chemotherapy and/or radiation therapy are usually not required unless malignancy is confirmed.
The long-term prognosis is good for patients with cervical teratomas. Recurrence rates are very low. However, recurrence has occurred in a small subset of patients. Despite the low malignancy rates in these tumors, markers for malignancy should still be checked. Postoperative surveillance should include assessing AFP levels at monthly intervals in infancy and yearly thereafter, up to 3 years of life.4 MRI scanning twice a year for the first 3 years of life also has been suggested.4
In conclusion, neonatal cervical teratomas are rare and are usually not cancerous. However, they can be associated with respiratory and endocrine complications. Surgical resection is curative. Long-term follow-up and a multidisciplinary team approach are needed to ensure a good prognosis.
- Chakravarti A, Shashidhar TB, Naglot S, Sahni JK. Head and neck teratomas in children: a case series. Indian J Otolaryngol Head Neck Surg. 2011;63(2):193-197. doi:10.1007/s12070-011-0224-8
- Jang J, Park J. Huge congenital cervical immature teratoma mimicking lymphatic malformation in a 7-day-old male neonate. J Pediatr Surg Case Rep. 2016;8:16-18. doi:10.1016/j.epsc.2016.03.005
- Tjalma WAA. The value of AFP in congenital cervical teratoma. J Pediatr Surg. 2003;38(12):1846. doi:10.1016/j.jpedsurg.2003.08.022
- Mohanty MK, Sahu P, Jaiswal AA, et al. A huge immature cervical teratoma; antenatal diagnosis, and its management—an unusual entity. J Clin Neonatol. 2013;2(1):42-45. doi:10.4103/2249-4847.109249
- Fernández KS. Solid tumors in the neonatal period. NeoReviews. 2014;15(2):e56-e68. doi:10.1542/neo.15-2-e56
- Hochwald O, Gil Z, Gordin A, et al. Three-step management of a newborn with a giant, highly vascularized, cervical teratoma: a case report. J Med Case Rep. 2019;13(1):73. doi:10.1186/s13256-019-1976-0
- Herman TE, Siegel MJ. Cervical teratoma. J Perinatol. 2008;28(9):649-651. doi:10.1038/jp.2008.84


