Peer Reviewed
Iliofemoral DVT Progressing to Phlegmasia Cerulea Dolens in a Woman With May-Thurner Syndrome
Authors:
Lauren A. Hutson, MD, MBA; Braden Harold Danbury; and Tapasdip Maheshkumar Gajjar, MD
Citation:
Hutson LA, Danbury BH, Gajjar TM. Iliofemoral DVT progressing to phlegmasia cerulea dolens in a woman with May-Thurner syndrome [published online August 22, 2018]. Cardiology Consultant.
A 48-year-old woman with a history of left ankle tendonitis 3 months prior and long-term use of estrogen oral contraceptives presented to the emergency department (ED) with pain and swelling in her left leg.
History. The pain had begun the night before and had ascended from her left leg to include her groin and back. She had until recently been using an orthopedic boot and crutches as a result of her ankle tendonitis. She denied other recent trauma, chest pain, dyspnea, cough, hemoptysis, fever, chills, abdominal pain, nausea, and vomiting. She also denied recent surgical procedures, recent travel, prolonged immobilization, and any history of coagulopathies, cancer, or cardiac disease. She denied smoking.
Physical examination. Her vital signs were within normal limits, except for an oxygen saturation of 87%. Cardiac and respiratory examinations revealed no abnormalities. Her left lower extremity was nontender without palpable cords, exhibited nonpitting edema from groin to foot, and had soft compartments, palpable pulses, and full range of motion. The skin was dry and cooler to the touch than that of the right leg.
Doppler ultrasonography of the leg revealed slow venous blood flow, normal luminal compressibility, and color flow without evidence of thrombi in the common femoral, femoral, deep femoral, popliteal, peroneal, or posterior tibial veins. She was discharged home in stable condition with a compression stocking and instructions to follow up with her primary care physician.
The next morning, she presented to a different ED for worsening pain and swelling despite medication, compression, and elevation. Her vital signs were still normal; her oxygen saturation was then 96%. Cardiac and respiratory examination findings were benign. Her left lower extremity was edematous and tender from hip to foot, with diminished pulse in the left ankle and decreased capillary refill in the left foot.
Diagnostic tests. A complete blood cell count with differential revealed leukocytosis (17,900 white blood cells/µL) and neutrophilia (15,560 neutrophils/µL). Prothrombin time was 13.3 seconds, the international normalized ratio was 1.0, and the activated partial thromboplastin time was 29.3 seconds. The lactate level was elevated at 27.9 mg/dL.
Results of computed tomography arteriography (CTA) of the abdomen with runoff including extremities revealed edema around the left femoral vein and possible expansion, in addition to dilation of the left external iliac vein with edema in the surrounding tissues. The left common iliac vein could not be visualized clearly. Findings from venous ultrasonography of the left leg revealed an extensive occlusive deep-vein thrombosis (DVT). Findings of CTA of the chest were negative for pulmonary emboli.
An intravenous heparin drip was started. Her condition progressed with pain in her left lower abdomen and discoloration of her left leg (Figure 1). She was admitted to the intensive care unit with diagnoses of DVT of the left deep femoral vein, systemic inflammatory response syndrome, phlegmasia cerulea dolens of the left lower extremity, and possible May-Thurner syndrome (MTS).

Figure 1. The patient’s legs on presentation to the ED.
Cardiology and interventional radiology specialists were consulted and intervened with urgent revascularization. Venography findings showed that the clot extended proximally to the iliac veins with concurrent high-grade stenosis of the left common iliac vein. An overnight catheter-directed infusion of tissue plasminogen activator was started in addition to continued heparin and pain medications.
The next day, the laboratory values had improved, but she still reported having severe pain. The limb remained swollen and tender with intact sensation and diminished pulse at the ankle.
A thrombectomy and thrombolysis were performed on the left superficial femoral vein, the left common femoral vein, the left external iliac vein, and the left common iliac vein. Findings from venography of the inferior vena cava and iliac veins followed by intravenous ultrasonography confirmed compression of the left common iliac vein between the right common iliac artery and the spine, with resulting stenosis (Figure 2 and Video).
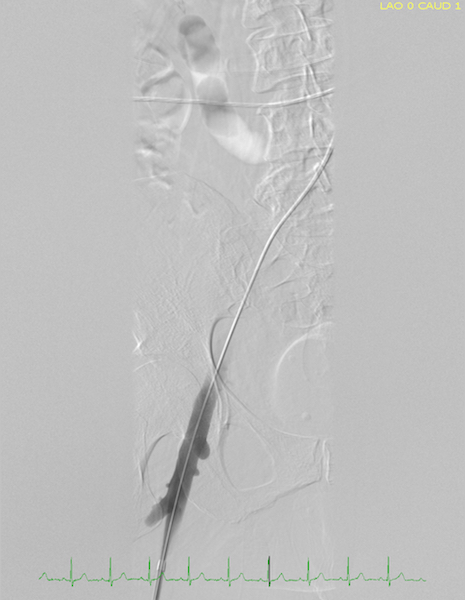
Figure 2. Image of venous flow during catheterization before stent placement.
Percutaneous transluminal valvuloplasty of the left common iliac vein, external iliac vein, and common femoral vein was done. A stent was deployed across the area of stenosis in the left common iliac vein and external iliac vein. Subsequent imaging showed excellent results (Figure 3 and Video). The patient reported relief of her pain following the procedure (Figure 4).
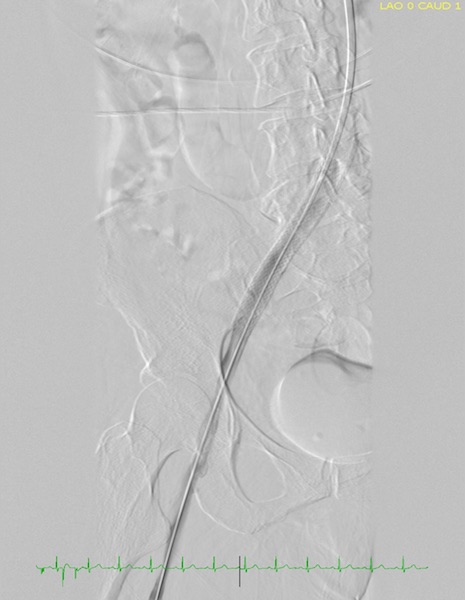
Figure 3. Image of venous flow during catheterization after stent placement.

Figure 4. The patient’s legs after treatment with catheter-directed tissue plasminogen activator.
She started anticoagulation prophylaxis with apixaban for 6 months. On hospital day 5, she was discharged home with instructions to stop taking estrogen oral contraceptives. She has not experienced another venous thrombus.
Discussion. MTS is an anatomic condition in which the right common iliac artery overlies and compresses the left common iliac vein against the fifth lumbar vertebra. This restricts the venous lumen and causes stenosis of the vessel wall. Based on their cadaver studies in 1957, May and Thurner estimated that the classic variant of the syndrome is present in 22% of the population.1 Others have described variants of the syndrome in which the common iliac veins and external iliac veins are compressed at different points by overlying arteries and become stenotic.2
Surprisingly, a newer study suggests that MTS is the cause of lower-extremity thromboses only 2% to 3% of the time.3 Additionally, MTS occurs twice as often in women than in men, and women are significantly more likely to also have a pulmonary embolism on presentation.4
This patient’s case differs from the common course of MTS. First, the patient’s clot burden was not detected on the initial ultrasonogram. A literature search revealed only one other record of an iliofemoral DVT in which the ultrasonogram was negative.5 It is unclear why the initial ultrasonogram failed, considering that the patient was not obese, the imaging was not abdominal, and the next day’s ultrasonogram revealed extensive venous occlusion. The authors of a recent case report and literature review suggest that in patients with a high suspicion for MTS, CT contrast venography, magnetic resonance venography, or intravenous ultrasonography is preferred to standard ultrasonography of the lower extremities for improved visualization of the iliac veins.6 The misleading initial ultrasonography result delayed the delivery of thrombolytic therapies and allowed the condition to progress, requiring intensive-care interventions.
Also noteworthy is the severe degree of circulatory compromise in this patient’s case. Phlegmasia cerulea dolens is a limb-threatening circulatory dysfunction and is one of the most severe consequences of a proximal DVT in MTS.7
The take-home message. It is important to include MTS in the differential diagnosis of a swollen lower extremity. It is not often considered as a cause of lower-extremity venous thrombus, but the subset of patients with it requires immediate intervention and extended care. MTS should also be part of the differential diagnosis in patients who decompensate after stenting of the common iliac artery for treatment of peripheral artery disease.8 This patient’s case emphasizes the importance of recognizing and addressing iliofemoral thrombus in MTS quickly.
Lauren A. Hutson, MD, MBA, is a resident physician at the Texas A&M Health Science Center College of Medicine–Baylor Scott & White Family Medicine Residency Program in Round Rock, Texas.
Braden Harold Danbury is a third-year medical student at the Texas A&M University College of Medicine in Austin, Texas, and a scholar of the National Health Service Corps.
Tapasdip Maheshkumar Gajjar, MD, is a hospitalist and physician advisor for utilization review at Baylor Scott & White Medical Center; an assistant professor at Texas A&M Health Science Center College of Medicine; and core faculty at the Texas A&M Health Science Center College of Medicine–Baylor Scott & White Internal Medicine Residency Program, all in Round Rock, Texas.
References:
- May R, Thurner J. The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veins. Angiology. 1957;8(5):419-427. doi:10.1177/000331975700800505
- Abboud G, Midulla M, Lions C, et al. “Right-sided” May-Thurner syndrome. Cardiovasc Intervent Radiol. 2009;33(5):1056-1059. doi:10.1007/s00270-009-9654-z
- O’Sullivan GJ, Semba CP, Bittner CA, et al. Endovascular management of iliac vein compression (May-Thurner) syndrome. J Vasc Interv Radiol. 2000;11(7):823-836. doi:10.1016/s1051-0443(07)61796-5
- Kaltenmeier CT, Erben Y, Indes J, et al. Systematic review of May-Thurner syndrome with emphasis on gender differences. J Vasc Surg Venous Lymphat Disord. 2018;6(3):399-407.e4. doi:10.1016/j.jvsv.2017.11.006
- Kiritsy M, Morley C, Habboushe J. Woman with left leg pain and swelling. Ann Emerg Med. 2017;69(3):375-381. doi:10.1016/j.annemergmed.2016.08.455
- Kalu S, Shah P, Natarajan A, Nwankwo N, Mustafa U, Hussain N. May-Thurner syndrome: a case report and review of the literature. Case Rep Vasc Med. 2013;2013:740182. doi:10.1155/2013/740182
- Mahomed A, Williams D. Phlegmasia caerulea dolens and venous gangrene. Br J Surg. 1996;83(8):1160-1161. doi:10.1002/bjs.1800830844
- Hermany PL, Badheka AO, Mena-Hurtado CI, Attaran RR. A unique case of May-Thurner syndrome: extrinsic compression of the common iliac vein after iliac stenting. JACC Cardiovasc Interv. 2016;9(5):e39-e41. doi:10.1016/j.jcin.2015.11.042


