Anorectal Complaints: Office Diagnosis and Treatment, Part 2
ABSTRACT: Symptoms associated with anorectal abscesses include throbbing or aching pain, swelling, drainage or bleeding, constipation, urinary difficulty, and fever. Treatment is surgical drainage. About 50% of anorectal abscesses fail to heal after drainage due to formation of an anal fistula. Characteristic findings in pilonidal disease include a painful, fluctuant mass near the posterior midline at the superior aspect of the buttocks and a sinus opening within the intergluteal fold. Treatment consists of drainage of the abscess followed by light daily packing. Patients with rectal prolapse may present with a protruding mass, a history of constipation and incontinence, bleeding, discharge, or a sensation of incomplete emptying. Pruritus ani can be caused by a number of anorectal disorders; however, in about 50% of cases, it is idiopathic. Anal neoplasms appear as unusual masses that arise from the anal or rectal mucosa; biopsy is often needed for diagnosis.
In Part 1 of our article (CONSULTANT, August 2012, page 567), we presented a general approach to the evaluation of patients with anorectal problems and discussed the diagnosis and management of hemorrhoids and anal fissures. Here we discuss a number of other common anorectal conditions: anorectal abscesses and fistulae, pilonidal disease, rectal prolapse, pruritus ani, and anal masses. For each, we outline the typical symptoms and physical findings and review appropriate management strategies.
If you encounter an anorectal disease for which you are unsure of the diagnosis, or if a patient’s complaint does not respond to conventional treatment, consider biopsy of the lesion (if one is present) or referral to a specialist.

ANORECTAL ABSCESSES AND FISTULAE
Anorectal infections may present acutely as abscesses or chronically as fistulae. Anorectal abscesses result from inflammation of the crypts and glands around the dentate line inside the anal canal and spread to various locations (perianal, intersphincteric, ischiorectal, supra-levator). Although a cryptoglandular origin is most common, other causes to consider include Crohn’s disease and a history of previous anorectal surgery.
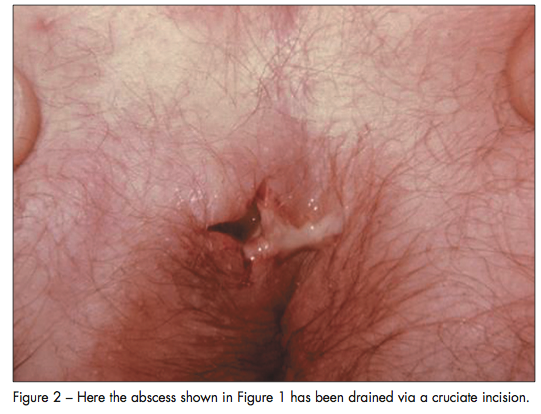
Abscesses. Patients often pre-sent with throbbing or aching pain, swelling, drainage or bleeding, constipation, urinary difficulty, and/or fever. Physical examination usually reveals an erythematous, fluctuant, and occasionally indurated mass that is tender to palpation (Figure 1).
Treatment consists of infiltrating local anesthesia into the overlying skin, followed by abscess drainage via a cruciate incision (Figure 2). Antibiotics are unnecessary in the treatment of anorectal abscesses except in the setting of sepsis, cellulitis, immunocompromise, or recent prosthesis. Keep in mind that only about 50% of abscesses heal primarily after drainage; the remainder result in anorectal fistulae.
Fistulae. Fistulae are the natural sequelae of drained anorectal abscesses that have not healed completely. Anoscopic evaluation typically reveals an internal opening within a crypt near the dentate line, and perineal inspection reveals an external opening in the skin. In the operating room, the fistula tract can often be demonstrated by introduction of a fistula probe (Figure 3). Fistulae can be classified based on their anatomic course in relation to the internal and external anal sphincters. The 4 types of fistulae are:
•Intersphincteric.
•Transsphincteric.
•Suprasphincteric.
•Extrasphincteric.
Surgical treatment is the mainstay of fistula management and includes fistulotomy, seton placement, mucosal advancement flaps, fistula plugs, ligation of intersphincteric fistula tract (LIFT) procedure, and fibrin glue injection.1

Figure 3 - The surgeon's probe demonstrates the tract of an intersphincteric fistula. It was successfully treated with fistulotomy.
PILONIDAL DISEASE
Pilonidal disease refers to an abscess or draining sinus that results from a subcutaneous infection in the sacrococcygeal region.
Symptoms and physical findings. Patients typically present with a painful, fluctuant mass near the posterior midline at the superior aspect of the buttocks. Examination of this area tends to reveal both a mass and a sinus opening within the intergluteal fold, which confirms the diagnosis.
Management. Treatment involves drainage of the abscess followed by light daily packing. Improved hygiene and meticulous hair removal (accomplished by shaving around the area) are important for optimal healing.2 Antibiotics are unnecessary except in high-risk populations (patients with sepsis, immunocompromise, or recent prosthesis).
RECTAL PROLAPSE
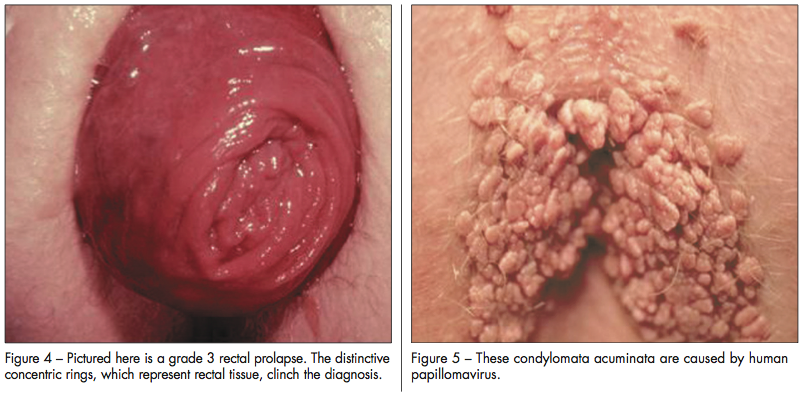
Rectal prolapse, or procidentia, represents an intussusception of the rectum. Its cause is unclear, but a redundant sigmoid colon and loss of rectal support and fixation are contributing factors. Prolapse may involve only the rectal mucosa (partial) or the full thickness of the rectum (complete). Rectal prolapse is classified as follows:
•Grade 1: occult prolapse.
•Grade 2: prolapse to the anus but not through it.
•Grade 3: protrusion through the anus for a variable distance.
Symptoms and physical findings. Patients may present with a protruding mass, a history of constipation and incontinence, bleeding, discharge, or a sensation of incomplete emptying. In patients with a grade 3 prolapse, physical examination reveals visible rectal tissue, which can be identified by its circumferential appearance (Figure 4). Visualization of radial folds or the dentate line may indicate the presence of prolapsed internal hemorrhoids. When the diagnosis is suggested by the history but not confirmed by the physical examination, further studies may be necessary (ie, defecating proctography).
Management. Treatment is surgical, via various abdominal or perineal procedures; the object is to prevent the sequelae of pudendal neuropathy, sphincter weakness, and fecal incontinence.3
PRURITUS ANI
Pruritus ani can result from a variety of causes, including fecal incontinence, systemic diseases such as diabetes, dermatologic conditions, drugs, dietary habits, and environmental factors. In addition, itching can result from any of the anorectal disorders discussed here and in part 1 of our article in the August issue. The physical examination may point you toward one or more of these diagnoses. If the physical findings do not suggest a specific cause, idiopathic pruritus ani is the likely diagnosis. In 50% of cases, perianal itching is defined as idiopathic, although occult fecal incontinence is likely the cause of many of these cases.
Treatment of idiopathic pruritus ani is multimodal. Instruct patients to use baby wipes instead of toilet tissue; use a cotton “plug” at the anus while sleeping to decrease anal drainage; take frequent warm baths; use psyllium or other bulking agents; apply topical hydrocortisone, anesthetic, and analgesic ointments; and use cornstarch to keep the perianal skin dry. Perform a skin biopsy if the pruritus is refractory to treatment.

ANAL MASSES
Anal masses can represent a variety of entities. The history of the mass, (including the time of its initial appearance, any variation in its size, and any recent change), the patient’s sexual preferences, and any history of a prior mass are important details that can help with diagnosis. Also, ask whether there has been associated pain, bleeding, pruritus, or discharge. Consider evaluation with a rigid sigmoidoscope to determine whether the mass extends from the rectum. The appearance of the mass on physical examination may make the diagnosis evident.
 Condylomata acuminata. These venereal warts are caused by the human papillomavirus (HPV) (Figure 5). The presence of warts, along with a history of anal intercourse, or of HIV infection or another immunocompromised state, strongly suggests the diagnosis. Treatment options include caustic agents (podophyllin, trichloroacetic acid), immunotherapy (imiquimod, interferon, autologous vaccines), chemotherapy (5-fluorouracil), and surgical treatment (excision, fulguration, laser therapy, cryotherapy). Because recurrence rates often exceed 50%, multiple treatments may be necessary. Of the various therapeutic modalities available, surgical excision has the lowest recurrence rate.
Condylomata acuminata. These venereal warts are caused by the human papillomavirus (HPV) (Figure 5). The presence of warts, along with a history of anal intercourse, or of HIV infection or another immunocompromised state, strongly suggests the diagnosis. Treatment options include caustic agents (podophyllin, trichloroacetic acid), immunotherapy (imiquimod, interferon, autologous vaccines), chemotherapy (5-fluorouracil), and surgical treatment (excision, fulguration, laser therapy, cryotherapy). Because recurrence rates often exceed 50%, multiple treatments may be necessary. Of the various therapeutic modalities available, surgical excision has the lowest recurrence rate.
HPV infection is associated with an increased risk of anal intraepithelial neoplasia (AIN), a dysplasia of the anal epithelium that can lead to anal carcinoma in situ or invasive anal cancer.4 Anal Papanicolaou tests can be used to screen for AIN. In patients with low-grade AIN, perform follow-up Papanicolaou tests at 6-month intervals. Patients with higher-grade dysplasia require biopsy with or without high-resolution anoscopy to evaluate for invasive anal cancer.
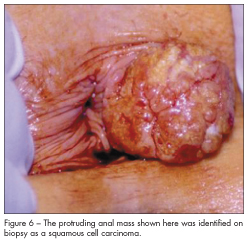
Anal neoplasms. These appear as unusual masses that arise from the anal or even rectal mucosa (Figure 6). They may be benign or malignant, and biopsy is often needed for diagnosis. Treatment options include wide local excision of the tumor, chemoradiation, and abdominoperineal resection with permanent colostomy; the optimal strategy depends on the histologic type and stage.
1. Shawki S, Wexner SD. Idiopathic fistula-in-ano. World J Gastroenterol. 2011;28;17(28):3277-3285.
2. Humphries AE, Duncan JE. Evaluation and management of pilonidal disease. Surg Clin North Am. 2010;90(1):113-124.
3. Maher C, Feiner B, Baessler K, Adams EJ, Hagen S, Glazener CM. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2010 Apr 14;(4):CD004014.
4. Simpson JA, Scholefield JH. Diagnosis and management of anal intraepithelial neoplasia and anal cancer. BMJ. 2011;343:d6818.
FOR MORE INFORMATION:
- Heard S. Pruritus ani. Aust Fam Physician. 2004;33:511-513.
- Kim DS, Tsang CB, Wong WD, et al. Complete rectal prolapse: evolution of management and results. Dis Colon Rectum. 1999;42:460-469.


